| |
Abstract
Subcutaneous fat necrosis of newborn is a form of panniculitis that often occurs in term and post-term neonate with predisposing risk factors such as perinatal asphyxia and maternal gestational diabetes. A cutaneous involvement may be associated with metabolic complications such as hypoglycemia, hypercalcemia and hypertriglyceridemia. Here, we present a case of Subcutaneous fat necrosis of newborn with bilateral symmetrical involvement of both axillas in a perinatal asphyxiated newborn that has not been previously described in the literature. In this case, there were no major complications apart from asymptomatic hypercalcemia.
Keywords: Subcutaneous fat necrosis; Neonate; Hypercalcemia.
Introduction
Subcutaneous fat necrosis of newborn (SCFN) is uncommon, acute, transient, self-limiting panniculitis of newborns that usually occurs in full-term infants with predisposing risk factors such as birth asphyxia, therapeutic hypothermia and maternal gestational diabetes. SCFN typically presents in the first 6 weeks of life and a characterized by indurated and erythematous nodules or plaques over bony prominences such as back, buttocks, thighs and arms.1-7 Prognosis is considered good with complete resolution within few weeks. Many rare but acute important complications have been noticed including hypercalcemia, thrombocytopenia, hypoglycemia, and hypertriglyceidemia.1-8 We are presenting a rare case of bilateral symmetrical SCFN that was complicated with asymptomatic hypercalcemia.
Case Report
A 2920-g male infant was born at 36-2/7 weeks of gestation to a noninsulin-dependent diabetic mother via emergency LCS due to moderate fetal distress. Standard maternal prenatal checkup revealed iron deficiency anemia with fair glycemic control of diabetes mellitus on insulin. The baby was depressed at birth and required positive pressure ventilation for three minutes after which the color improved. His heart rate increased to 120 BPM, but he remained with weak breathing effort and poor tone, and was thus intubated and admitted to NICU. The APGAR score was 2/1, 5/5 minutes. Cord blood gas showed mixed respiratory and metabolic acidosis (pH 6.95, pCO2 102, HCO3 13, BE-9.3).
During the first 24 hours of life, he required inotropic support because of hemodynamic instability. He had two episodes of hypoglycemia that required two boluses of 10% dextrose. In view of suspected sepsis, a septic workup was done and antibiotics were started. He was ventilated with minimal settings for two days then he was extubated. On his 5th day of life, he developed bilateral symmetrical axillary swellings (Fig. 1), tender on touch, lobulated and measuring 3 × 3 cm. The overlying skin was normal with no redness or draining sinus. Ampicillin was changed to cloxacillin, and cefotaxime was continued after consulting pediatric surgeons. Further workup was done because the swellings were increasing rapidly in size including screening for CMV, TORCH, syphilis, HIV, which all reported as negative.

Figure 1: Large, erythematous, indurated, smooth swelling on the right axilla of the neonate on day 5 of life.
Soft tissue ultrasound was done and showed partially necrotic lymph node. On day 11 of life, a biopsy of the right-sided skin nodule was taken and histopathology examination revealed subcutaneous fat necrosis. Because of the self-limiting nature of the disease, the baby did not receive any therapy. The antibiotics were stopped and supportive care was provided. Throughout his stay, he remained afebrile. Blood cultures were done twice and both showed no growth. Serum calcium levels were monitored during admission and it remained normal. When it was repeated 3 days after discharge, it showed a mild increase in levels up to 2.96 mmol/L. He was monitored closely in OPD until the levels normalized after 6 weeks. Throughout, he remained asymptomatic and required no intervention.
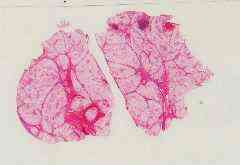
Figure 2: Biopsy from the subcutaneous tissue showed the pathology in subcutaneous tissue (lower power).
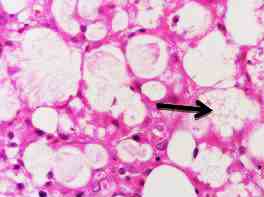
Figure 3: A high-power view showing adipocyte necrosis and inflammation with presence of giant foamy macrophages in the hypodermis (headed arrow).
Discussion
Subcutaneous fat necrosis of the newborn was described for the first time in 1875 by Cruise. Initially, it was called scleroderma of newborn infant.4 It is an uncommon benign, self-limiting condition seen primarily in term and post-term neonate,1-4 and there are only a few reported cases of SCFN among pre-term neonates.5 The SCFN may develop in the first 6 weeks of life, with one study reporting 45% of lesions appearing in the first week of life.1,7 It is characterized by multiple erythematous, indurated, firm, non-pitting plaques or nodules over fat-bearing surfaces like the back, buttocks, thighs and arms.1,3-7 Rarely, face and anterior trunk are involved.3 The case presented here showed bilateral symmetrical SCFN over the inferior aspect of both axilla, which has not been previously described in the literature. Only three cases have been reported with bilateral involvement, all of them after therapeutic hypothermia.6
The exact mechanism is unknown but may be initiated by ischemic injury, hypoxia and hypothermia. Most affected neonates had a history of perinatal asphaxia.4,5,7 Other predisposing factors include hypothermia, meconium aspiration, obstetric trauma, sepsis, gestational diabetes, pre-eclampsia,1-7 and Rh incompatibility.6,7 The diagnosis is clinical, but when the clinical diagnosis is not typical, skin biopsy is helpful.4 Another reported alternative method for diagnosis is fine needle aspiration of the subcutaneous lesions.3 The typical histopathological findings of SCFN are lobular panniculitis, with extensive fat necrosis, numerous radial eosinophilic crystals, and an infiltrate of lymphocytes, histiocytes and multinucleated giant cell.1,4-8
SCFN is a benign condition that generally follows an uncomplicated course with complete resolution without scarring within several weeks to 6 months.3 However, there are many rare important reported complications for which the patient must be monitored closely. These include hypercalcemia, thrombocytopenia, hypertriglyceridemia, hypoglycemia,1-8 local tissue breakdown, and abscess formation.6 The patient developed asymptomatic hypercalcemia that resolved spontaneously within 6 weeks. Treatment includes supportive care, topical antibiotics and dressing for ulcerated lesion.
Conclusion
We reported this case to highlight the rare site of this rare condition. It is a benign condition but it can lead to many complications which may be life threatening if left untreated. This necessitates careful followup until full resolution.
Acknowledgments
The authors reported no conflict of interest and no funding was received for this work.
References
1. Wiadrowski TP, Marshman G. Subcutaneous fat necrosis of the newborn following hypothermia and complicated by pain and hypercalcaemia. Australas J Dermatol 2001 Aug;42(3):207-210.
2. Mahé E, Girszyn N, Hadj-Rabia S, Bodemer C, Hamel-Teillac D, De Prost Y. Subcutaneous fat necrosis of the newborn: a systematic evaluation of risk factors, clinical manifestations, complications and outcome of 16 children. Br J Dermatol 2007 Apr;156(4):709-715.
3. Tran JT, Sheth AP. Complications of subcutaneous fat necrosis of the newborn: a case report and review of the literature. Pediatr Dermatol 2003 May-Jun;20(3):257-261.
4. Singalavanija S, Limponsanurak W, Wannaprasert T. Subcutaneous fat necrosis of the newborn. J Med Assoc Thai 2007 Jun;90(6):1214-1220.
5. Mitra S, Dove J, Somisetty SK. Subcutaneous fat necrosis in newborn-an unusual case and review of literature. Eur J Pediatr 2011 Sep;170(9):1107-1110.
6. Hogeling M, Meddles K, Berk DR, Bruckner AL, Shimotake TK, Cohen RS, et al. Extensive subcutaneous fat necrosis of the newborn associated with therapeutic hypothermia. Pediatr Dermatol 2012 Jan-Feb;29(1):59-63.
7. Borgia F, De Pasquale L, Cacace C, Meo P, Guarneri C, Cannavo SP. Subcutaneous fat necrosis of the newborn: be aware of hypercalcaemia. J Paediatr Child Health 2006 May;42(5):316-318.
8. Ladoyanni E, Moss C, Brown RM, Ogboli M. Subcutaneous fat necrosis in a newborn associated with asymptomatic and uncomplicated hypercalcemia. Pediatr Dermatol 2009 Mar-Apr;26(2):217-219.
|
|