Scarf osteotomy - Is it the procedure of choice in hallux valgus surgery? A preliminary report
S.S.Suresh
ABSTRACT
Many procedures are described in the literature for the surgical management of hallux valgus. There are over 130 surgical procedures described but the surgeon usually limits these to a few which he is comfortable with and which gives the best aesthetic and functional result to the patient. There is ever rising enthusiasm among orthopaedic surgeons regarding diaphyseal osteotomy ever since Burutaran described the procedure in 1973. Weil in United States and Barouk in Europe popularized the technique. Scarf is a double chevron diaphyseal osteotomy which is inherently more stable than other osteotomies on the first metatarsal and allows early return to work. The author reports his early experience with SCARF osteotomy, which is a comparatively new technique for hallux valgus correction which was done in Ibri Regional Hospital in the Sultanate of Oman. All patients who presented with symptomatic hallux valgus were taken up and there were three patients who required surgical intervention for hallux valgus. The purpose of this study was to find its effectiveness in terms of stability of the osteotomy and early return to work. Proximal phalangeal osteotomy was not found necessary in none of the three cases operated by us. Scarf osteotomy is safe and found to give better aesthetic and functional result and early return to work. All our three patients had good functional recovery and early return to work.
Keywords: Hallux Valgus, metatarsal osteotomy, Scarf osteotomy
Submitted: 20 August 2007
Reviewed: 29 August 2007
Accepted: 4 September 2007
From the Department of Orthopedics, Ibri Regional Hospital, Ibri, Sultanate of Oman
Address correspondence and reprint request to: S.S. Suresh, Department of Orthopedics, Ibri Regional Hospital, Sultanate of Oman.
Email: dr.s.s.suresh@gmail.com
INTRODUCTION
Numerous osteotomies have been described for the surgical correction of metatarsus primary varus component of the hallux valgus deformity. Over 130 metatarsal osteotomies have been described in the world literature for the surgical management of hallux valgus. In clinical practice most of the surgeons limit these to a few procedures which invariably include soft tissue release, medial exostostomy combined with either proximal or distal osteotomy of the first metatarsal. The outcome of surgical correction is sometimes unsatisfactory to the surgeon and undesirable for the patient. Any surgical procedure should result in a congruous first metatarso-phalangeal joint, painfree motion, improved cosmesis and ability to wear desirable footwear. The procedure should also result in the least number of complications and should be easily reproducible. The first metatarsal scarf osteotomy has significantly improved the correction in hallux valgus and has recently gained popularity among European surgeons.1 It can be extended to a wide range of indications and result in early functional recovery with least number of complications.
METHOD
Three cases of hallux valgus were operated by this technique from August 2005 till December 2006. The patients were operated for forefoot pain in one case, whose occupation is driver. One girl was operated for cosmetic concern. And Shoe wearing problem was the presentation in a serving soldier. The patients were evaluated with radiographs, both weight bearing and non weight bearing films in antero posterior and lateral planes. Intermetatarsal and hallux valgus angles were measured. The first metatarso phalangeal joint was mobile and didn’t show any signs of degenerative arthritis in all patients. A clinical photograph also was taken for pre operative record. All cases were operated and followed up by the author.
SURGICAL PROCEDURE
All cases were done under epidural anaesthesia under tourniquet control.
Technique of First Metatarsal Osteotomy
A median incision was done under tourniquet control from the midshaft level of the proximal phalanx distally to the base of the first metatarsal proximally. The plantar blood supply was taken care of during the procedure. The capsule and periosteal structures were elevated from the metatarsal head and neck. Divide the thin septum joining the abductor muscle to the medial border of the first metatarsal. Thus the first metatarsal medial border and its medial plantar surface were clearly visible. Carefully preserve the dorsal synovial fold attached just proximal to the first metatarsal articular cartilage. The periosteal tissue about the first metatarsal shaft are incised in line with the proposed osteotomy and elevated plantarly and dorsally for few millimeters.
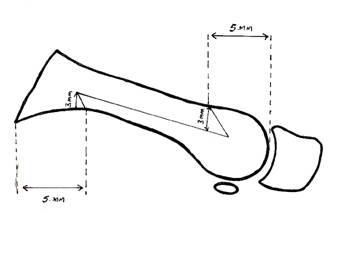
Fig 1: Z osteotomy cuts and measurements
There are two components after the scarf osteotomy cuts are made - a proximally based dorsal fragment and a plantar fragment, which comprises the plantar surface and the metatarsal head. The longitudinal cut is then followed by two transverse cuts- making this a double chevron. Median eminence resection is done. Proximal cut is located 3 mm above the medial border, 5 mm distal to the articular surface of base of metatarsal. The distal end is located 3 mm below the dorsal medial edge, located at the level of the proximal end of articular cartilage of the dorsal surface. The cut is made from proximal to distal. The longitudinal cut is made laterally and plantarward so that it reaches the lateral surface near its plantar border. This lowers the plantar head fragment and preserves the lateral surface which acts as a strong strut. The osteotomy is done in a through and through fashion and is usually between 40 to 50 mm in length.
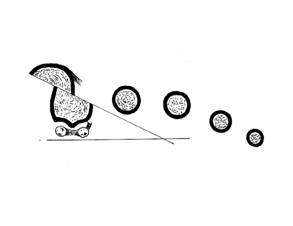
Fig 2: Orientation of the transverse cut
The transverse cuts are both chevron, directed proximally and at 60 degrees to the longitudinal cuts. The proximal cut is performed first, around 5 mm from the articular surface and 2-3 mm from the plantar surface.
 
Fig 3: Pre and post operative X-rays
While doing the distal transverse cut care is taken to avoid damage to the dorsal lateral blood supply. Once the cuts are made a spatula is inserted to separate the fragments. The fragments can be displaced two thirds to three-fourths of the surface depending on the correction required. The displacement is done by the “push and pull” technique popularized by Barouk. This is achieved by pushing the plantar fragment and pulling the dorsal fragment. By medially rotating the head and plantar fragment the lateral inclination of the articular cartilage of the head can be corrected thereby correcting the DMAA (Distal Metatarsal Articular Angle). Fixation of the osteotomy is done with AO screws - we used 2 mm screw in one case and 3.5 mm screws in two cases. The distal fixation is done about 1 cm proximally from the distal end of the dorsal fragment. The screw is directed 45 degrees oblique, distally and plantar ward. Care is taken to prevent screw penetration into the plantar cortex or articular cartilage. The screw was countersunk in the dorsal fragment. The proximal screw is placed in an oblique direction to reach the plantar cortex in a stronger part of the shaft. The bone excess on the medial distal part of the dorsal fragment after displacement of the osteotomy is resected, and this can be used as bone graft if required.
Lateral Release of The Metatarso Sesamiodal – Phalangeal Complex (Mspc)
The lateral release releases the sesamoids from the head of the metatarsals so that after displacement osteotomy it lies in correct position above the sesamoids. The lateral sesamoid attachment to the adductor is not released and the inter metatarsal ligament is undisturbed. The phalangeal insertional band of the sesamoid is released. The lateral capsule is released with multiple punctures with a number 11 blade. The release is done through a small lateral intermetatarsal approach. In addition to the phalangeal insertional band, the metatarsal sesamoid suspensory ligament is cut, taking care not to damage the lateral blood supply to the plantar head. The adductor tendon is not detached from the lateral sesamoid in this approach.
Medial Capsulorrhaphy
Medial capsular closure is an important step in hallux valgus corrective surgery. The great toe is held in plantar flexion during closure of the capsule, Ensuring that there is ideal repositioning of the sesamoid underneath the metatarsal head while closure. A compression dressing is applied and a below knee cast is given. The patients wore a forefoot cast for 3 weeks. Progressive weight bearing is started while in the cast with heel touch down. The patient was allowed to wear their normal footwear after 3 weeks. In none of our cases a proximal phalangeal osteotomy of Akin or other metatarsal osteotomies were necessary as there was good correction of the hallux valgus preoperatively and there was no residual deformity while doing the “Load stimulation test”.1
RESULTS
All parameters were significantly improved by the surgery, and all patients got the desired cosmetic result. All patients were pain free at follow up. The longest follow up was 18 months and the shortest was 5 months. This is only a preliminary report of a technique which is comparatively new and gaining popularity among foot and ankle surgeons world over.
Table 1: Characteristics of patients undergoing Scarf Osteotomy
|
No |
Age |
Sex |
Side |
Pre Op IMT |
Pre Op
HV |
Post Op
IMT |
Post Op
HV |
DOS |
|
1 |
17 |
F |
L |
12 |
50 |
10 |
15 |
20/8/05 |
|
2 |
55 |
M |
L |
35 |
26 |
12 |
16 |
22/4/06 |
|
3 |
27 |
M |
L |
20 |
36 |
09 |
17 |
11/12/06 |
DISCUSSION
More than 130 procedures are described for the surgical treatment of hallux valgus. These include distal osteotomies (Chevron, Mitchell, Wilson osteotomies) or proximal metatarsal osteotomies.1,2 The procedure gaining popularity among surgeons especially in Europe is the diaphyseal Z step cut osteotomy named as scarf osteotomy. Scarf is the English translation for the phrase” le trait de Jupiter des Charpentiers”- a technique used by carpenters to increase the size of an entrance by beveling two beams to correspond.1,3, 4 It was in 1973 that Burutaran described a similar cut in the first metatarsal for lengthening of the first ray.1 Zygmunt in 1983 started performing Z cuts with lateral shift of the first metatarsal head.3 The method gained momentum after the description of the technique by Borrelli and Weil in 1984, they gave the name “scarf” to this technique.1 The technique is popularized in Europe by Barouk who has done more than 2300 scarf osteotomies. Scarf is a combination procedure which includes median eminence resection and medial capsular plication, metatarsal osteotomy, lateral soft tissue release and if required proximal phalangeal osteotomy (Akin). The procedures are done in combination.
In addition to the above techniques the metatarsal can be lengthened as described by Burutaran. It should be reserved for young patients with normal first MP joints (Weil).3 There are many methods of fixation described by different authors. Barouk has developed a specific cannulated scarf screw, with a threaded head,1 which is self tapping, with a long distal thread. Scwartz and Groves reported their results after fixation with internal threaded Kirschner wires.5 Other modalities of fixation were with AO cancellous screws, 2 mm and 3.5 mm and with asymmetric pitched screws. We use either a 2 mm AO screw or 3.5 mm screw depending on the bone quality and size. Popoff has shown that the ultimate load and stiffness of scarf osteotomy fixed with cannulated symmetric pitched screws were not superior to the AO screws.6 There is rigid compression of large areas of bone on bone which provides environment for primary bone healing.
The head of the first metatarsal can be lowered as much as 7 mm. Lowering occurs automatically by the orientation of the cuts combined with the lateral shift. Lowering reduces metatarsalgia of the second ray and significantly reduces the need for osteotomies of the second metatarsal for metatarsalgia. The possible complications include under and over correction and stress fracture of the proximal first metatarsal. Barouk reported over correction in 3 (0.3%) cases in a series of 920 scarf osteotomies. He concluded that the lateral soft tissues should be carefully preserved and he advocates limited medial capsular plication. He also performs the load stimulation test to see if the correction is acceptable while weight bearing.1,4 Barouk also reported 5 (0.55%) under correction in a series of 920 cases which he attributed to insufficient lateral displacement. Freson in a study of 123 surgeries found the correction better when scarf osteotomy is combined with phalangeal osteotomy.7 Stress fracture of the proximal part of first metatarsal is reported in the literature by various authors. Barouk reported 17 (3%) stress fractures in his early series of 565 cases, which he attributed later to improper placement of the proximal screw and not respecting the strong lateral surface of the first metatarsal. In Coetzee’s series, 2 (10%) out of 20 cases developed stress fracture.8 All these studies showing high incidence of stress fractures were done by inexperienced surgeons or during their early cases.
Other complications like post operative stiffness of the first meta tarso phalangeal joint, infection, avascular necrosis of head of first metacarpal and prominent hardware are only rarely reported in the literature.9,10 Coetzee could not reproduce the excellent results reported by others in his analysis of 20 patients. He encountered troughing of the metatarsal with loss of metatarsal height, delayed union, proximal fracture and infection. There was 25% early recurrence of the deformity in his series.8 He concluded that scarf osteotomy has multiple potential pitfalls and he advised to reserve this procedure for moderate hallux valgus in young people with good bone stock. The configuration of the scarf osteotomy is found more stable to the weight bearing stresses than the proximal or distal osteotomies.9, 10, 11, 12 However, in a study of over 1000 cases done in Belgium by Dereymaeker, none of the cases went for non union and they encountered stress fracture only in two cases, which healed eventually.13 Barouk reported up to 03% of stress fractures in his early series. He also reported that under correction and over correction is very rare.1 The author found this procedure versatile and surgeon friendly in correcting hallux valgus. The sample size is too small to make any judgments at this stage and needs a larger series with comparison with various other procedures.
CONCLUSION
Scarf osteotomy is a powerful and versatile procedure to correct hallux valgus deformity. This allows the patient to ambulate post operatively early, as the osteotomy is inherently stable and return to work at an earlier date as compared to other procedures. Bilateral procedures are also possible. Scarf osteotomy provides a predictable and satisfying result. Scarfs are not considered as a single osteotomy but as a combination of several procedures and displacement in several planes are possible. The indication can be extended to severe hallux deformities including secondary deformities as in juvenile and rheumatoid hallux deformity. The author reports early experience with the above technique which is described in detail. Though the author got good functional and cosmetic outcome with the technique the sample size is too small for a comparative study. The aim of this paper was to create awareness of this diaphyseal osteotomy the indications of which could be extended to even severe hallux valgus.
ACKNOWLEDGEMENTS
The author thanks the Director General of Health Services Mr.Ali Khalfan Al Mandhary, Dr John Idikula, Executive Director, Ibri hospital and Mr. Fahad Masoud Al Jassasi, Director of Administrative and Financial Affairs for their encouragement and support. The author also thanks Mr. Sukumar of Radiology department for the illustrations.
REFERENCES
-
Barouk LS. Scarf osteotomy for hallux valgus correction localanatomy,surgical technique, and combination with other forefoot procedures. Foot and clinics, 2000; 5:525-558.
-
Robinson A.H.N, Limbers J.P. Aspects of current management-concepts in thetreatment of hallux valgus. J Bone Joint Surg Br 2005; 87:1038-1045.
-
Weil L.S. Scarf osteotomy for correction of hallux valgus. Historical prospective, surgical technique and results. Foot Ankle Int 2000; 5:559-580.
-
Jones S, Al Hussainy H.A, Ali F. Scarf osteotomy for hallux valgus- A prospective clinical and pedobarographic study. J Bone Joint Surg 2004; 86:830-836.
-
Schwartz N, Groves E.R. Long-term follow-up of internal threaded Kirschner wire fixation of the scarf bunionectomy. J Foot Surg 1987; 26:313-316.
-
Popoff I, Negrine J.P, Zecovic M et al.The effect of screw type on the Bio- mechanical properties of SCARF and cresentic osteotomies of the first metatarsal. J Foot Ankle Surg 2003; 42:161-164.
-
Fresion M, Gayet L.E, Bouche G etal. Scarf osteotomy for the treatment of hallux valgus: a review of 123 cases with 4.8 years of follow-up. Rev Chir Orthop Reparatrice Appar Mot 2005; 91:257-266.
-
Coetzee J.C. Scarf osteotomy for hallux valgus repair: the dark side. Foot Ankle Int 2003; 24:29-33.
-
Acevedo J.I, Sammarco V.J, Boucher H.R et al. Mechanical comparison of cyclic loading in five different first metatarsal shaft osteotomies. Foot Ankle Int 2002; 23:711-716.
-
Trnka H.J, Parks B.G, Ivanic G. Six first metatarsal shaft osteotomies: Mechanical and immobilization comparisons. Clin Orthop Relat Res 2000; 381:256-265.
-
Smith A.M, Alwan T, Daview M.S. Perioperative complications of the Scarf osteotomy. Foot Ankle Int 2003; 24:222-227.
-
Dereymaeker G. Scarf osteotomy for correction of hallux valgus. Surgical technique and results as compared to distal chevron osteotomy. Foot Ankle Int 2000; 5:513-524.
-
Creviosier X, Mouhsine E, Ortalano Vet al. The scarf osteotomy for the treatment of hallux valgus deformity: A review of 84 cases. Foot Ankle Int 2001; 22:970-976.
-
Kristen K.H, Berger C, Stelzig S et al. Scarf osteotomy for correction of hallux valgus deformities. Foot Ankle Int 2002; 23:221-229.
|