|
Introduction
Mullerian duct anomalies are congenital anomalies of the female genital tract resulting from non-development or non fusion of the mullerian ducts, or failed resorption of the uterine septum.1 Duplication of the uterus results from the lack of fusion of the paramesonephric ducts in a local area or throughout their normal line of fusion. In uterus didelphys, individual horns are fully developed, normal in size with two cervices inevitably present. Each hemiuteri is associated with one fallopian tube. Ovarian malposition may also be present. A longitudinal or transverse vaginal septum may be noted.
The vagina may be single or double. Duplicated vagina is more likely in a didelphic uterus. Ipsilateral renal agenesis with partial vaginal septum on the same side and didelphys uterus is explained by embryologic arrest at the 8th week of gestation affecting simultaneously the mullerian and metanephric ducts.2 True prevalence of this anomaly is unknown as it may be discovered in later part of patients life when presenting with infertility. The incidence of mullerian duct anomalies in literature ranges from 0.5 and 5.0%. Approximately 11% of uterine malformations are didelphic uteri.3
Case Report
A 25 year-old woman married for one year and half presented for the first time in the outpatient department with complaints of frequent, heavy, painful menstruation and foul smelling vaginal discharge. General physical examination was unremarkable. Vaginal examination showed a large cystic bulge in the right lateral vaginal wall with foul smelling discharge from the same side. On the left side, cervix was palpable easily, whereas the right side cervix could not be felt as there was a vaginal septum partially obstructing the vagina. Pelvic ultrasonography showed two widely divergent uterine horns with two cervical canals (Fig. 1). The right cervix was distended with fluid up to the right lateral vaginal wall (Fig. 2). Pelvic MRI confirmed the findings of uterus didelphys with right hemivagina, a right lateral vaginal wall swelling with ipsilateral renal agenesis (Figs. 3,4,5 are axial, sagittal and coronal views). Intravenous urogram reported as incomplete duplex of the left kidney with non visualized right kidney. Left kidney was mildly enlarged with two upper and lower pelvicalyceal systems. The ureters of the left upper and lower moities united at the level of left transverse process of L3 vertebra forming a single left ureter (Fig. 6). On the basis of imaging and clinical association a diagnosis of uterus didelphys with unilateral obstructed hemivagina with ipsilateral renal agenesis was recognized in this case (OHVIRA Syndrome).
The patient's complaints of dysmenorrhoea continued with regular menstrual cycles. Diagnostic laparoscopy confirmed the findings of double uterus with normal fallopian tubes and ovaries on either side. A vaginal septotomy was performed and 200 ml of purulent discharge was drained (Fig. 7). Post operative period was uneventful, and she was relieved of complaints after surgical excision of the partial vaginal septum. Vaginal examination at postoperative visit confirmed double cervices. She conceived spontaneously in the left uterine horn after 3 months (Fig. 8), and is presntly following in the antenatal clinic at Nizwa hospital.
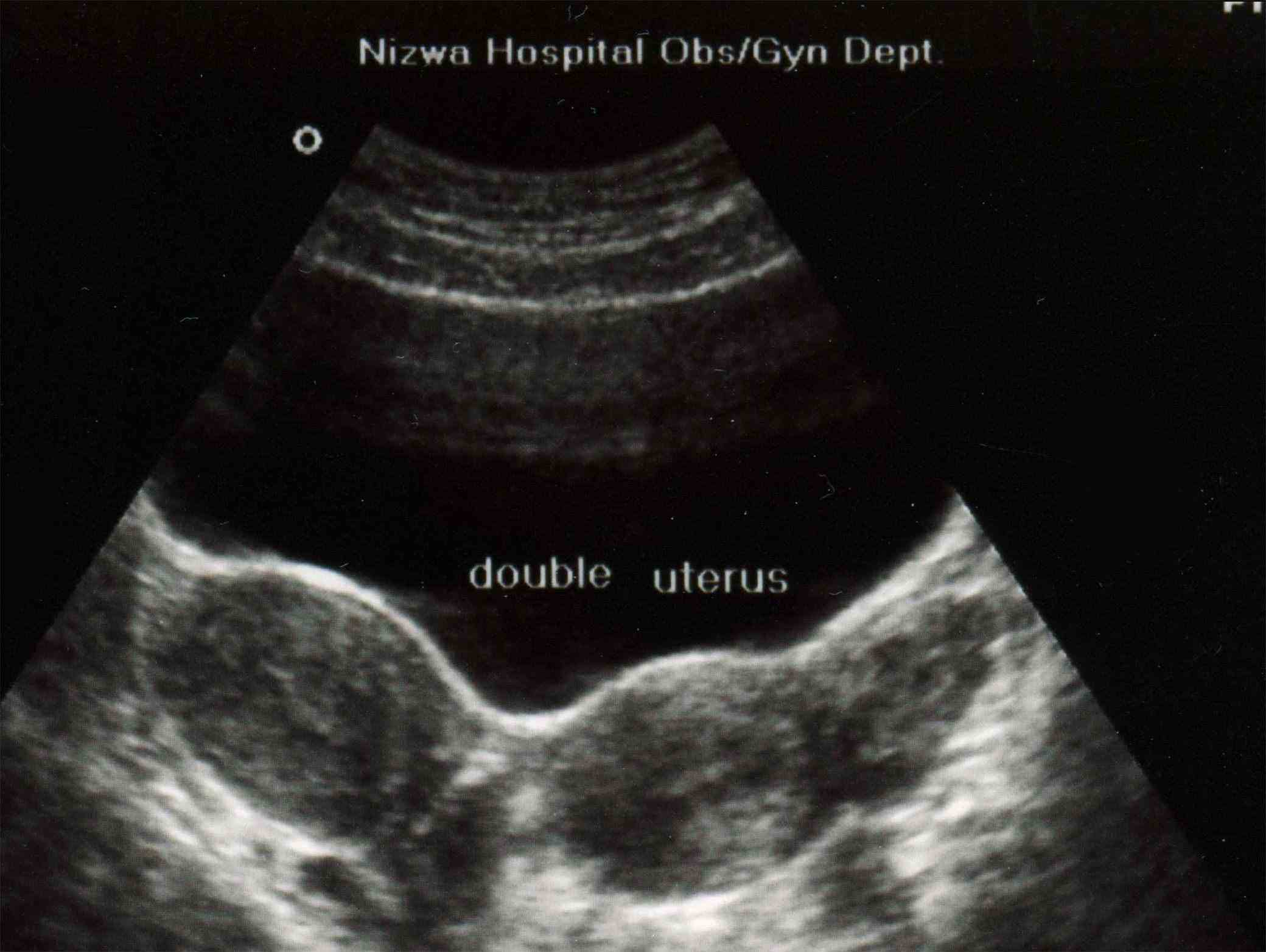
Figure 1: Transverse transabdominal sonographic image through the pelvis demonstrates the two uteri.
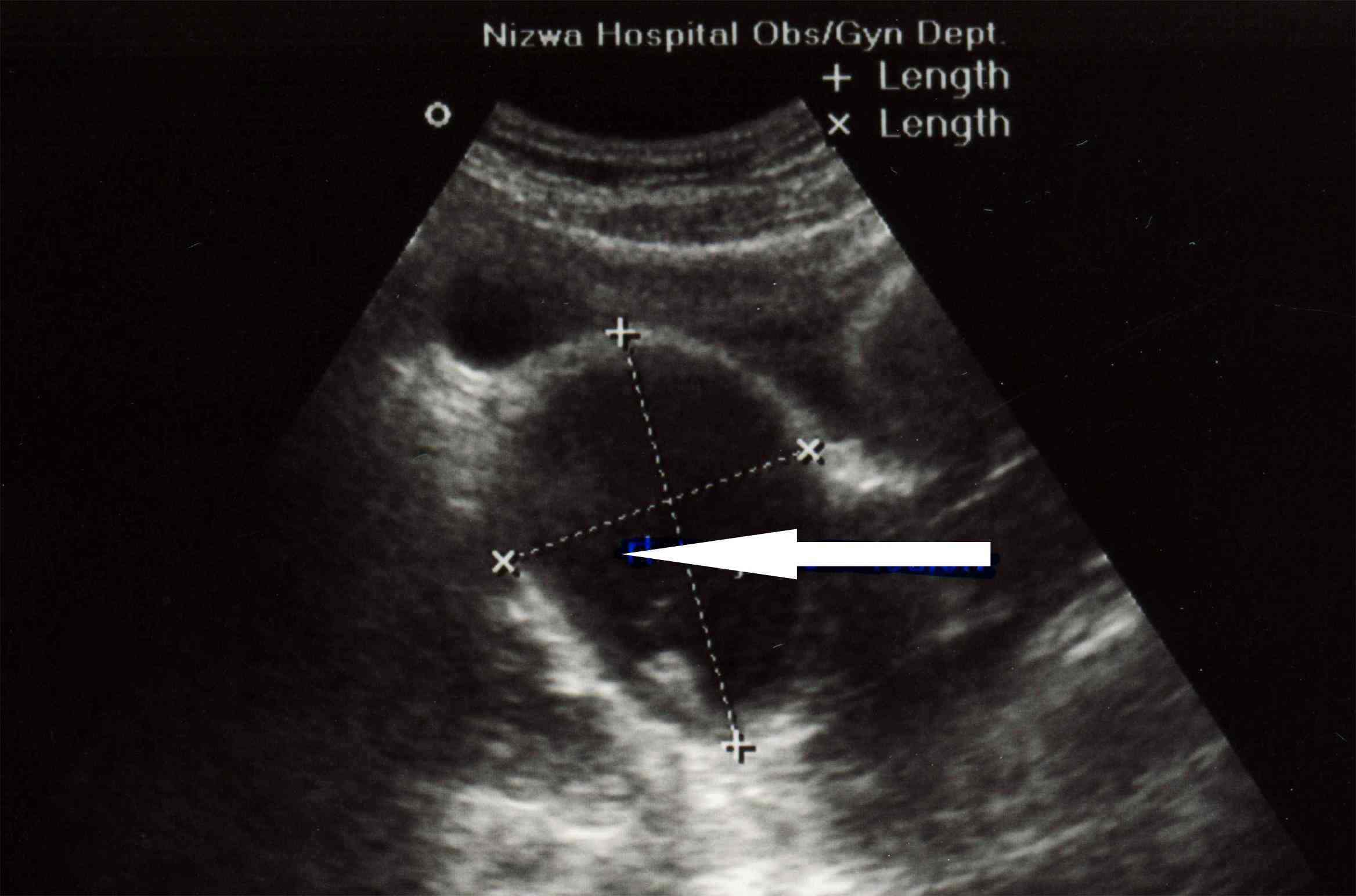
Figure 2: Right pyocolpos: Longitudinal transabdominal sonographic image through the pelvis demonstrates cystic structure with echogenic material inside, representing distended right upper hemivagina.

Figure 3: Axial T2-weighted MR image demonstrates dilated right hemivagina with high T2-signal-intensity fluid (pyocolpos, P) compressing the left hemivagina (V). Normal appearance both uteri (U) with normal endometrium plate.
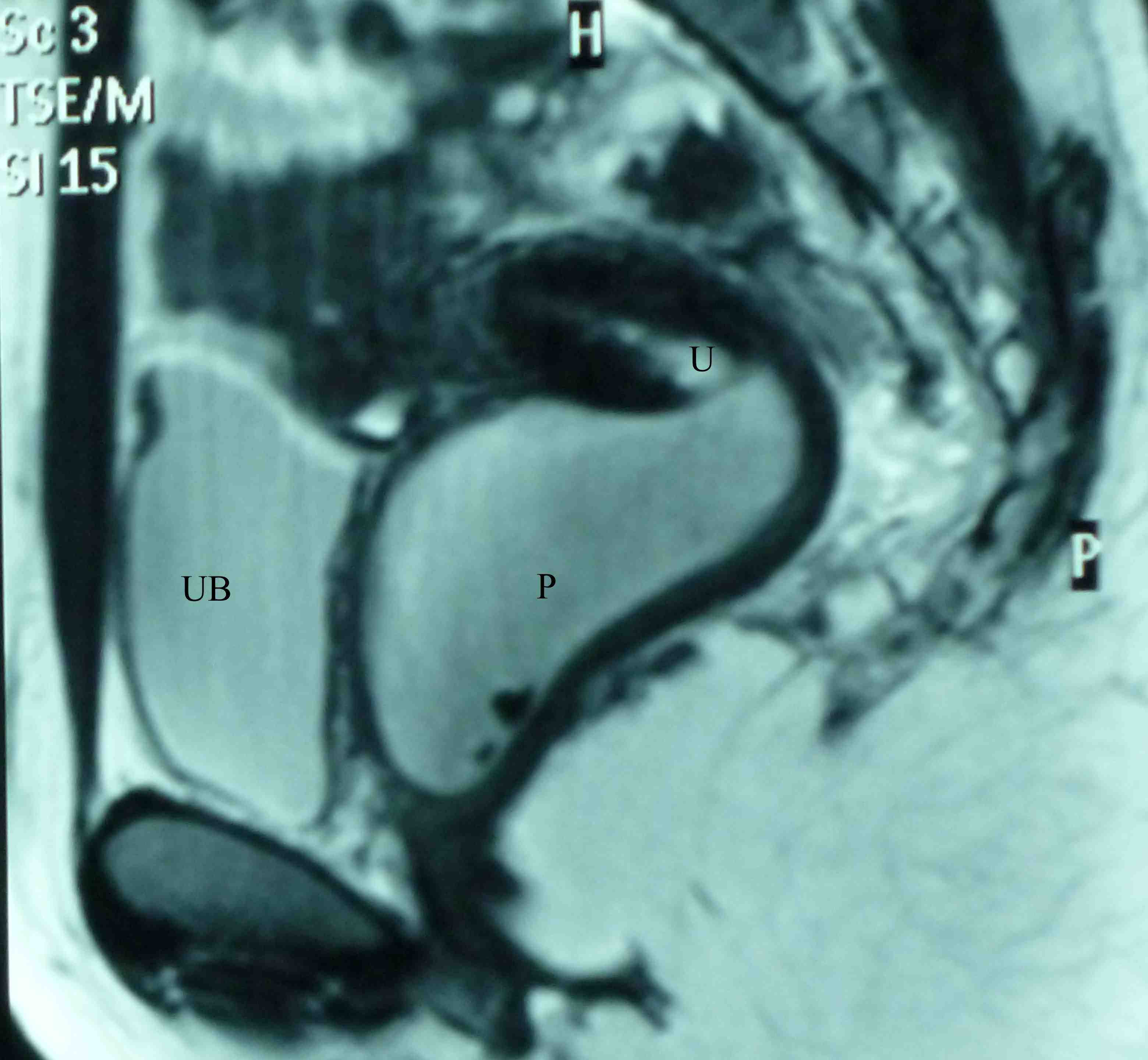
Figure 4: Sagittal T2-weighted MR image demonstrates dilated right hemivagina with high T2-signal-intensity fluid (pyocolpos, P) extending into endocervical canal of right uterus (U), Urinary bladder (UB).
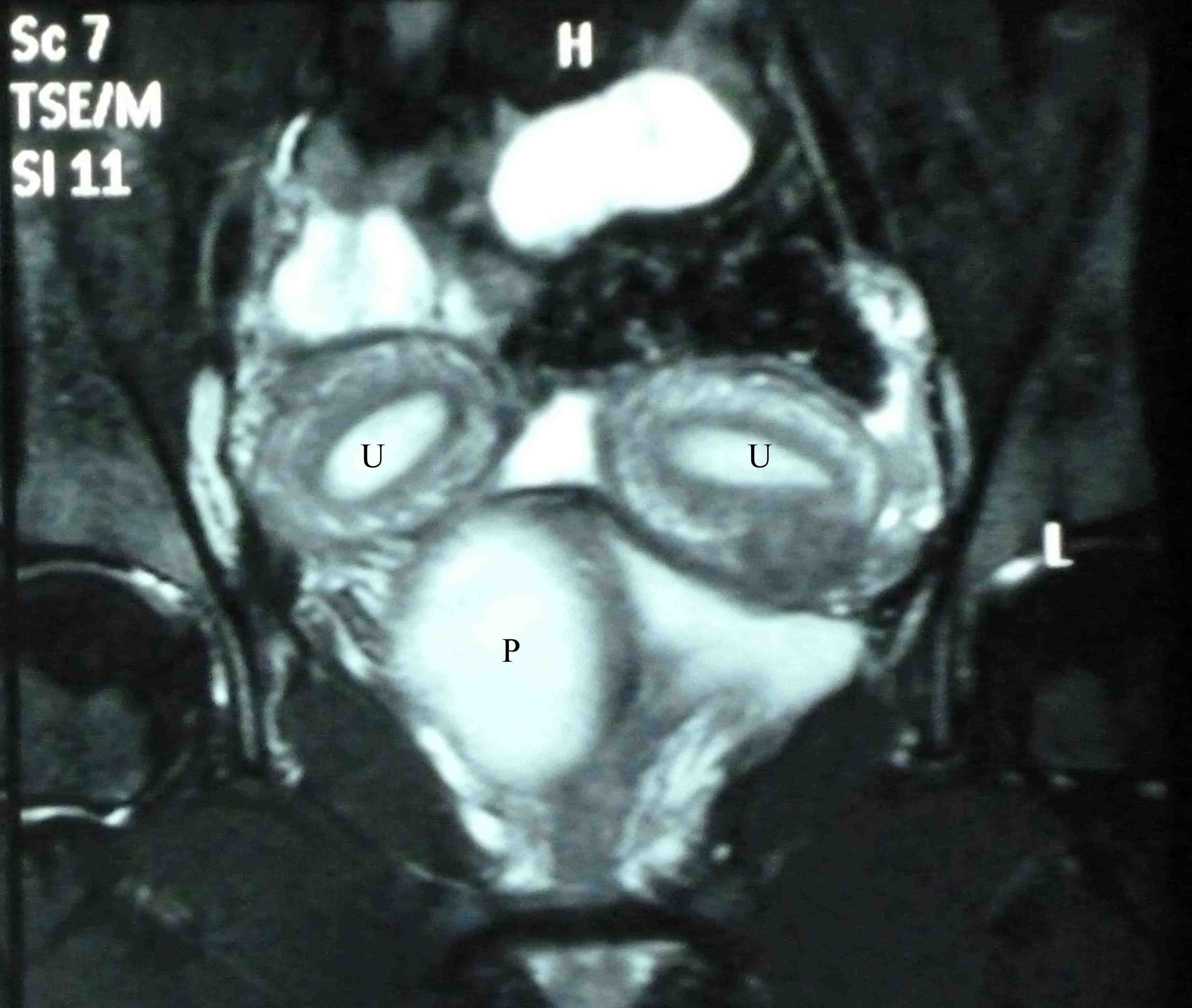
Figure 5: Coronal T2-weighted MR image with fat suppression, demonstrates dilated right hemivagina with high T2-signalintensity fluid (pyocolpos, P). Normal-appearing both uteri (U) with normal endometrium plate.

Figure 6: Intravenous urogram (IVU) demonstrates incomplete duplex of left kidney with ureters of upper and lower moieties seen united at level of L3 transverse process level.
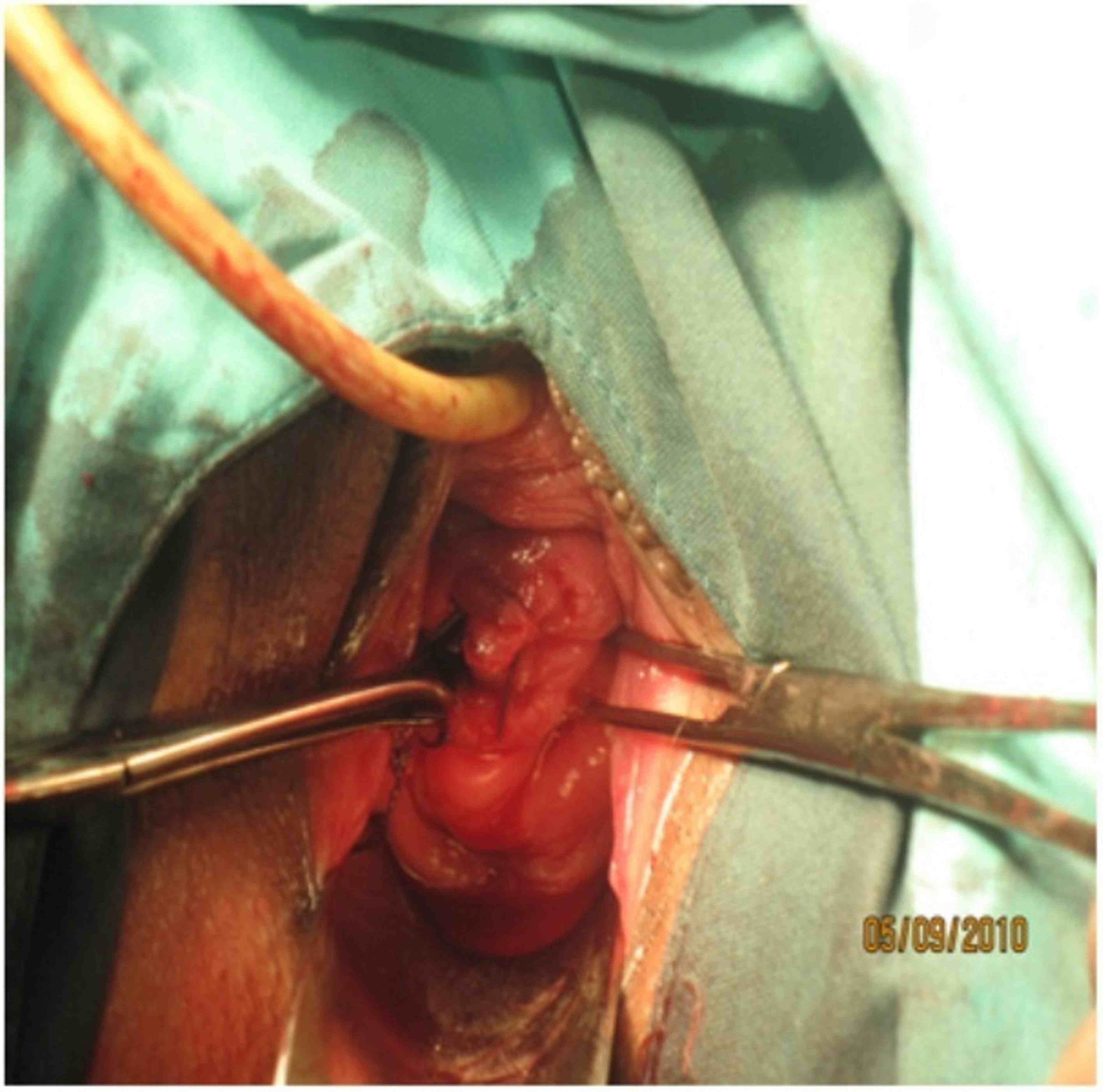
Figure 7: Double cervices in volsellum after right side septotomy

Figure 8: Transverse transabdominal sonographic image through the pelvis demonstrates the two uteri with gestational sac and fetal pole in the left uterus.
Discussion
There is a high association between mullerian duct and renal anomalies such as unilateral agenesis. Patients most often present for medical attention because of infertility and repeated pregnancy loss. Routine imaging for infertility workup often detects the anomaly.
Uterus didelphys with obstructed hemivagina is an obstructive mullerian anomaly caused by the lateral nonfusion of the mullerian ducts with asymmetrical obstruction. Renal agenesis most commonly occurs in association with uterine didelphys than with any other type of mullerian anomaly. The reported incidence of renal anomalies in this group is 20%.4 OHVIRA syndrome represents obstructed hemivagina with ipsilateral renal anomaly and is classically associated with uterus didelphys.5,6 Obstructed unilateral vagina in patients with uterus didelphys is frequently associated with ipsilateral renal and ureter agenesis. Resection of the vaginal septum is the treatment of choice for obstructed hemivagina for symptom relief and preservation of reproductive capabilities. Hysteroscopic resection of the septum under transabdominal guidance may also be carried out so as to preserve the hymenal integrity in young females.2 In transverse ultrasound vaginal septum, a vertical fusion disorder exists between the mullerian ducts and the urogenital sinus. It may be complete or incomplete and it is not usually associated with other urologic or mullerian anomalies.7 Didelphic uteri have the highest association with transverse vaginal septum.8
The role of imaging is to help detect, diagnose and distinguish surgically correctable forms of mullerian malformations from inoperable forms.9 Abdominal or transvaginal ultrasound is cheap and noninvasive. Three-dimensional (3D) has higher sensitivity and specificity to evaluate malformations. While Computed tomography (CT) has a limited role in the evaluation of female pelvis, whereas magnetic resonance imaging (MRI) is highly sensitive. The vaginal septum is difficult to visualize on ultrasound and is best shown on MRI.10
Uterus didelphys has been associated with higher rate of infertility, spontaneous abortion, intrauterine growth retardation, preterm labor and postpartum bleed.11 Patients may present with severe dysmenorrhoea, lower abdominal pain, paravaginal mass, excessive foul smelling mucopurulent discharge and intermenstrual bleeding depending on the existence of uterine or vaginal communications.12
In patients presenting with palpable abdominal, pelvic or vaginal mass (mucocolpos or pyocolpos), mullerian duct anomalies must be excluded.13,14 The diagnosis of this rare mullerian anomaly, also known as Herlyn-Werner-Wunderlich Syndrome (HWWS) should be suspected in women who have ipsilateral renal agenesis with a pelvic mass.15
Conclusion
Early diagnosis of this condition with appropriate surgical intervention decreases the long term morbidity. Untreated cases develop retrograde tubal reflux and endometriosis. It causes impaired fertility and other obstetric complications later in life. The rarity and unusual presentation may contribute to diagnostic delay as in this case with regular menstrual cycles, she was asymptomatic and uterine abnormality was diagnosed years after menarche.
Acknowledgements
The authors reported no conflict of interest, and no financial or personal relationship with people or organizations that could inappropriately influence this work.
|