|
INTRODUCTION
Post-partum ovarian vein thrombosis (POVT) is an uncommon clinical presentation. The incidence being 0.02-0.05%.1,2 Most of the patients present within 10 days of the puerperal period with symptoms of right loin and right iliac fossa pain. Two patients who were referred to the imaging department at the Sultan Qaboos Hospital, Salalah for suspected appendicitis and right ureteric colic, are reported. Both patients showed right hydronephrosis and hydroureter by ultrasound along with evidence of right ovarian vein thrombus. The findings seen on imaging may be difficult to interpret unless the diagnosis of POVT is considered and looked for. Hence there is a definite need to suspect this condition even though the incidence is low and include the same in the differential diagnosis of patients presenting with acute abdomen during the puerperal period. POVT can be accurately diagnosed by appropriate non-invasive investigations to enable early therapy with anti-coagulants and intravenous antibiotics which are the mainstay in the treatment of this condition. Surgery can be avoided if diagnosis is made early.3
CASE REPORT:1
A 27-year-old female, gravida 2, para 1, presented with gradual onset of right loin pain radiating to the right iliac fossa and fever, 10 days after an uncomplicated vaginal delivery. She was referred from the obstetrics unit for an Ultrasound evaluation for suspected ureteric colic. There was no nausea or vomiting. Clinical examination showed that the patient was febrile with right loin tenderness. No mass was felt in the right loin. The rest of the clinical examination was normal. Blood picture showed leucocytosis. Ultrasound examination of KUB was done, which showed a mild prominence of the pelvicalyceal system of right kidney and right ureter with an elongated distended tubular structure seen in the right iliac fossa placed more laterally. Subsequently, an abdominal ultrasound with color-flow Doppler showed a suspicious thrombus distending and occluding the right ovarian vein with no flow seen on Doppler. (Figs. 1, 2)
.jpg)
Figures 1: USG-RIF Showing thrombosed ovarian vein
Figure 2: Doppler-showing no flow
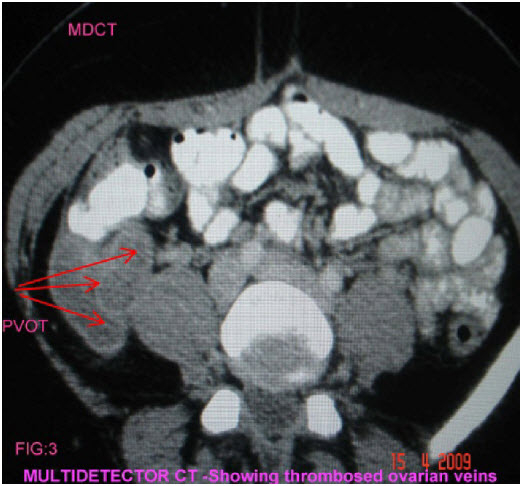
Figure 3: MDCT-Axial
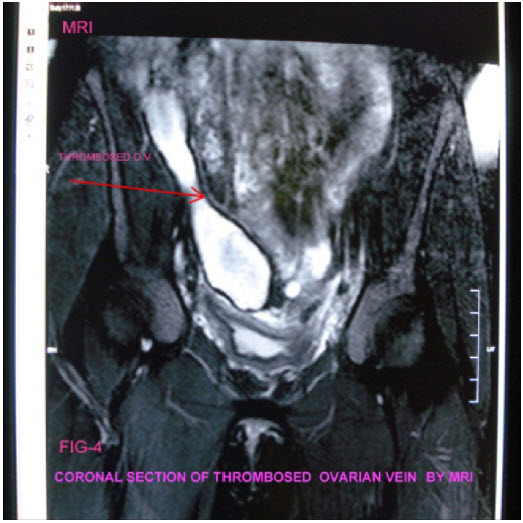
Figure 4: MRI-Coronal
A diagnosis of distended right ovarian vein with an intraluminal thrombosis was made and the patient was taken up for contrast Multidetector computerized tomography (MDCT). MDCT showed a thrombus within the right ovarian vein. (Figs. 3, 5)
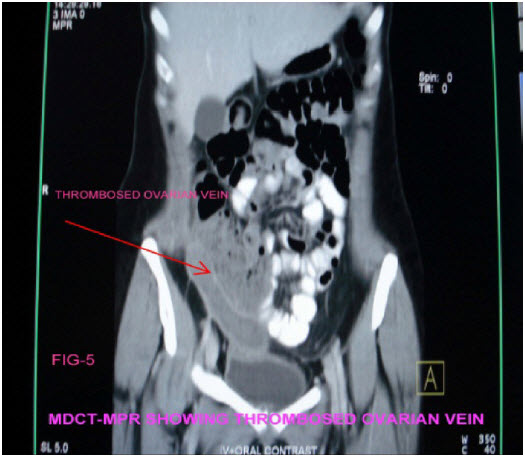
Figure 5: MDCT-Coronal
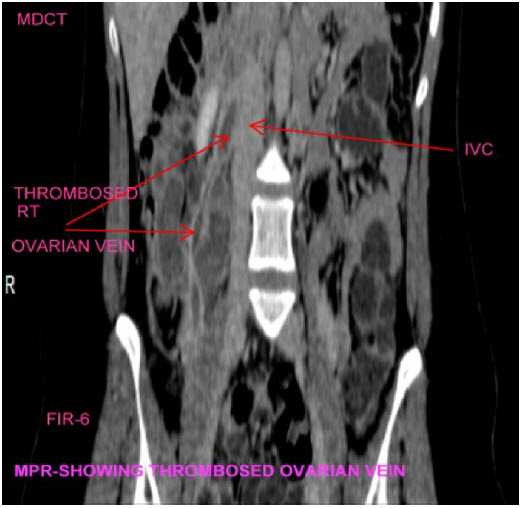
Figure 6: MDCT-Coronal
Magnetic resonance imaging (MRI) was also done which confirmed the diagnosis of post-partum ovarian thrombosis (POVT), (Fig. 4). The patient was treated for 10 days with intra-venous heparin, cefuroxime, gentamicin and metronidazole. The pain and fever resolved and the patient was discharged on warfarin.
CASE REPORT: 2
A 23-year-old female, gravida 1, para 1, seven days after a normal vaginal delivery was referred to the urology department with symptoms suggestive of right ureteric colic, as the patient complained of right loin pain radiating to the right iliac fossa. There was no nausea or vomiting. On examination, the patient was febrile, with right lower quadrant tenderness and no mass was felt clinically. The blood picture showed leucocytosis. An abdominal Ultrasound performed showed mild right hydronephrosis and right hydroureter with thrombosis of the right ovarian vein extending into the inferior vena cava (POVT), (Fig. 6). This was confirmed by MDCT and MRI. The patient was treated for one week with intravenous heparin, amoxycillin, gentamicin and metronidazole. The pain and fever resolved and she was discharged on warfarin and was doing well.
DISCUSSION
Ovarian vein thrombosis occurs in post partum women due to the combination of venous stasis and hypercoagulability, which are commonly seen in that period. The incidence of post-partum ovarian vein thrombosis is 1:2000 deliveries.4 The majority of cases occur within one week of delivery. Both the reported cases presented within 10 days of delivery.
The ovarian veins form a plexus near the ovary within the broad ligament and communicate with the uterine plexus. These veins ascend in pairs in the retroperitoneum adjacent to the psoas muscle, and then combine to form a single vein before their termination.5
80-90% of POVT occur in the right ovarian vein. The right ovarian vein terminates in the inferior vena cava at an acute angle and the left ovarian vein terminates in the left renal vein at right angles. Retrograde flow in the left ovarian vein and antegrade flow in the right ovarian vein have been observed in the immediate post-partum period.6
Regarding the hydroureter, it is believed to be due, in part, to the commonly occurring dextro torsion of the enlarged uterus, which causes compression of the right ovarian vein and right ureter as they cross the pelvic rim.7 The right ovarian vein is also longer than the left ovarian vein and has many valves within its length. These valves may act as a nidus for thrombosis.8
The veins enlarge greatly during pregnancy to accommodate increased blood volume and following childbirth, a period when venous stasis occurs. The right ovarian vein and the right ureter are more likely to be compressed by the dextro rotation of the involuting uterus.9 Both reported cases presented with right hydronephrosis and hydroureters. Complications include ovarian vein thrombophlebitis, which can result in sepsis, thrombosis of the inferior vena cava and renal veins, and can lead to pulmonary embolism (25%) and death (5% of complicated cases, with estimated 18 deaths per million pregnancies).10,11 The pathogenesis of thrombus formation in the ovarian vein involves many factors. In addition to the existing hyper-coagulable state during pregnancy and puerprium, there is also a decrease in blood flow velocity immediately following delivery.
This may also contribute to the development of a thrombus. If there is an associated endometritis, the blood flowing from the uterus could carry pathogenic bacteria to the right ovarian vein thereby predisposing it to septic thrombosis. Puerperal endometritis has been postulated as a possible cause of POVT. Anaerobic bacteria, which are usually present in the lower genital tract, are able to generate endothelial injury and stasis with secondary thrombosis of the pelvic veins. The bacteria gain access to the ovarian veins from the septic endometrium by crossing the uterine and vaginal venous, and lymphatic plexus.12
The usual clinical features of POVT are as described in the cases above. 80% of patients present with pyrexia. Lower quadrant pain and flank pain with associated nausea is a common presentation. In some cases, mass may be palpable in the right iliac fossa. The differential diagnoses of ovarian vein thrombosis are appendicitis, septic pelvic thrombophlebitis, Ureteric colic with sepsis, peritonitis, adnexal torsion, pyelonephritis and tubo-ovarian abscess.13
A positive diagnosis of POVT can be made by Ultrasonography, Magnetic resonance imaging (MRI) or MDCT scan with a sensitivity of 52%, 92% and 100%, respectively.14 Doppler Study of inferior vena cava (IVC) and ovarian veins also show the thrombus and is a useful tool for follow up.15 Magnetic resonance angiography can provide a better and more reliable visualization of the vascular systems and the coronal source images are useful in evaluating the extent of the thrombus. MDCT study with bolus injection of iodinated contrast and a conventional venography are also accurate methods for diagnosing POVT.
Dilated, thick-walled ovarian veins with rim enhancement and a central hypodensity are considered to be the main CT findings of POVT as seen in the reported cases.16 Regarding treatment, most studies suggest the use of low molecular weight heparin (LMWH) and broad-spectrum antibiotics in non-complicated cases of POVT, but there is no consensus about the class of antibiotics that are used and the dosage or duration of treatment.17 After initiating thrombolysis with heparin, it is maintained with Warfarin orally for three months as was done in these two patients. When conservative line fails to control symptoms or when there is a high risk of pulmonary embolism, endovascular or surgical procedures, such as thrombectomy, Inferior Venacaval filters, Ovarian vein or Venacaval ligation, may be indicated.18
CONCLUSION
Diagnosis and treatment of POVT are non-invasive in 90% of cases. It is therefore necessary to entertain a diagnosis of POVT when faced with a post-partum patient with lower quadrant abdominal pain and fever. The initial modality of study is an Ultrasound examination with Doppler. A high index of clinical suspicion should necessitate a CT or MRI scans for confirmation. As POVT commonly mimics Appendicitis clinically, early diagnosis by the discussed modalities can help to avoid unnecessary surgery.
ACKNOWLEDGEMENTS
The authors reported no conflict of interest and no funding was received on this work.
|