|
Introduction
The nose is of critical aesthetic and functional significance, and nasal reconstruction requires an appreciation of facial, aesthetics and physiological functional factors. Without a comprehensive evaluation of the nasal defects and the anticipated reconstructive outcome; re-establishment of facial balance and nasal breathing can be lost. Due to its projection, the nose is one of the most common anatomical structures of the face to get injured, and the common causes of nasal injury include; fall, road traffic accidents, sport injuries and assaults. Besides trauma, other causes of iatrogenic vestibular stenosis include; nasal trauma and infection secondary to iatrogenic insults for oxygen therapy.1 The sequelae of trauma to nose include; nasal deformity, nasal obstruction leading to negative impact on patients’ quality of life. In the pediatric age group; obstructions to the anterior portion of the nasal passage (that is the vestibule and external nasal valves) are typically of congenital, traumatic, or iatrogenic etiology.2
Nasal trauma may result in a combination of soft tissue injury, fracture of nasal bones and the septum; the risk of occurrence of nasal septal deformities increases after nasal injuries.3 Other possible complications include; septal hematoma, aesthetic complications like disfigurement of the nose, and saddling of the nasal bridge; besides these patients are liable to suffer from lifelong functional problems like vestibular stenosis- a possible stenosis of the external and internal nasal valves.1
The nasal valve is the mobile, airflow-regulating part of the nose that serves as the bridge between the bony skeleton and the nasal tip.4 This valve is the narrowest part of the nasal airway and poses the greatest resistance to nasal airflow. The valve is bound superolaterally by the caudal edge of the upper lateral cartilage, and the lateral border includes the bony piriform aperture and the fibrofatty tissue of the ala. The nasal valve ends inferiorly at the nasal floor; the head of the inferior turbinate forms the posterior limit of the nasal valve and it includes the area between the caudal end of the upper lateral cartilages and the superior septum, forming an angle of 10-15 degrees. Changes in this angle can induce airflow turbulence and nasal obstruction.
Most authors have concluded that following any type of trauma to the nose; it is desirable to avoid vestibular stenosis, because once nasal vestibular stenosis occurs, it is a very difficult functional problem to treat.5,6 The stenting can be used for re-canalization post- Young’s procedure and nasal valve preservation. This article presents for the first time, a novel method of stenting of the nasal vestibule and cavity in a 16 month old child presenting with an extensive injury to the nose.
Case Report
A sixteen month old child was brought to the accident and emergency department at Sultan Qaboos University Hospital. The parents gave a history of falling on a sharp edge of a metallic bed. Following the injury; the child had a profuse nasal bleeding and a deep lacerated nasal wound. There was no history of loss of consciousness or vomiting. On examination, the child was irritable with profuse epistaxis, and there was a deep lacerated wound extending from the collumellar base toward the tip of the nose with nasal bleeding.
Primarily, the child was managed in the emergency department by arresting the nasal bleeding with bilateral merocel 4 cm nasal packs. The child was hemodynamically stabilized and vitals were closely monitored. X-Ray of the nasal bones did not add to the clinical assessment. A reconstructive surgery was planned under general anesthesia on the next day theater list. Ideally, the child should have been operated on the same night.
The surgical technique was conducted under general anesthesia for cleaning and exploration of the wound, which was observed to be a deep lacerated wound extending from the base of the collumella externally deep toward the nasal angle superiorly above the quadrilateral cartilage leaving it intact. (Fig. 1)
Suturing of the wound was done in layers with vicryl 4-0 starting by approximation of the deep soft tissue near the septal angle and gradually extending inferiorly until the collumella was reached. Varieties of techniques are used when closing lacerating nasal injuries. In the presented case, the following precautions were taken: a) Tension-free closure to minimize scarring, b) averting the superficial layers during suturing, c) symmetric and precise placement of sutures with attention to the anatomic layers, d) care while suturing the Collumella, and e) the use of V-nasal stent to minimize the risk of postoperative synechea and vestibular stenosis.

Figure 1: The wound caused by the injury.
Nasal stents are routinely used after nasal surgery to keep raw surfaces apart, prevent contractions and closing of the nasal airway by granulations; since postoperative scar contractions and adhesions are inherent characteristics of the nasal mucosa. The traditional way to place readymade stents is to place it in the saggital plane (Fig. 2) sheet, anchored to the collumella to prevent slippage into the nasopharynx. We have modified this by inserting thin 0.50 mm silicone sheeting. A rectangular piece 2 cm by 1.0 cm was cut and inserted bilaterally in the nasal cavities like an inverted V shape; this was fixed by a silk 4-0 bilaterally in the nasal cavity to the nasal septum and secured well to avoid slippage of the stent, (Fig. 2). Because of the inherent spring affect, a gentle pressure was applied to the lateral nasal wall and septum, thus creating a tunnel in between. Following the stent placement and fixation, size 4 merocel nasal packs were introduced for two days between the two flaps of the stent to secure hemostasis.
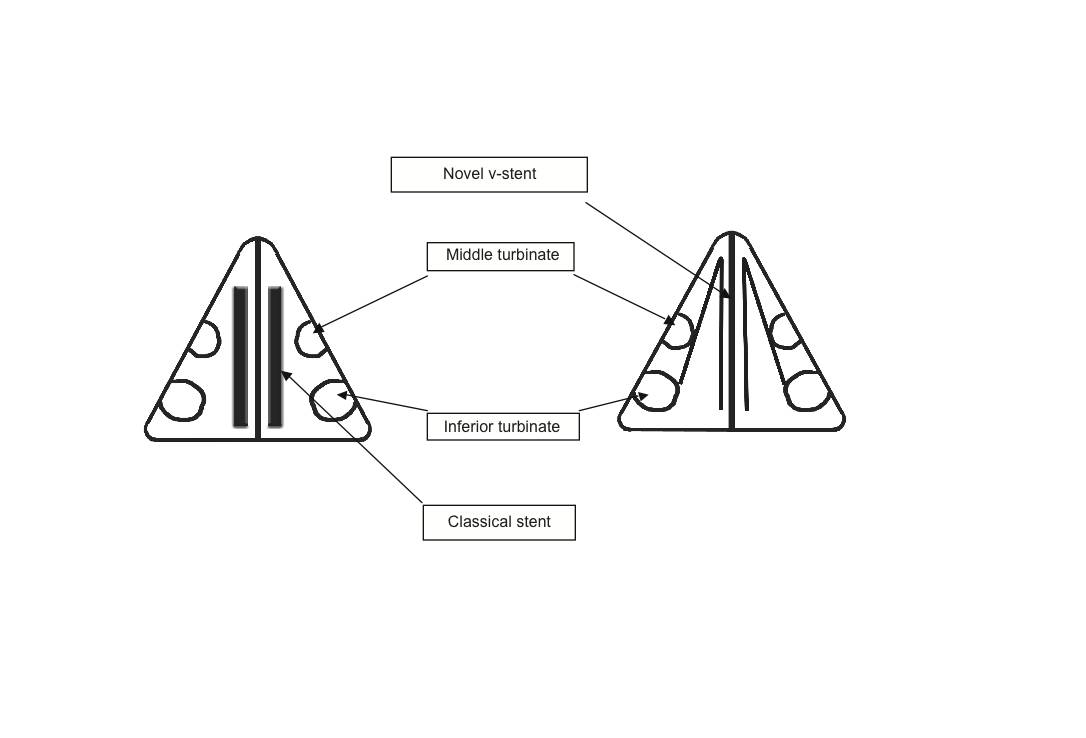
Figure 2: Diagrammatic representation of saggital section of traditional stents in the nose and the inverted V-Stent.

Figure 3: Postoperative results 4 months later.
The patient was discharged the morning after the removal of the nasal packs. Three weeks later, the patient was reassessed and the nasal splint was removed. The child tolerated the soft stents very well and made a remarkable recovery with no aesthetic of functional sequelae of the trauma and surgery, (Fig. 3). Following this case, we have used this stent in other patients with nasal trauma and extensive nasal surgery with good cosmetic and functional results.
Discussion
Vestibular stenosis can be a result of infection, foreign body reaction, or trauma, which could be iatrogenic or accidental. Iatrogenic vestibular stenosis is a complication of supportive care, with minimal literature describing this entity.6 Stents are traditionally used to avoid vestibular stenosis; these have been fashioned from a variety of resources, including nasal airway tubes, endotracheal tubes and suction catheters.1 Bilateral, circular stents have been described to avoid contact of raw surfaces,5 to decrease the risk of vestibular stenosis leading to functional and aesthetic problems.7,8
Small children are more prone to vestibular stenoses due to small area to work on, complex three dimensional surface of the nose, and the varying thickness of the skin. Healing in the vestibular region is usually by secondary intention due to the limited amount of vestibular skin; also, the nasal mucosa has an inherent characteristic of developing synechia, because whenever the nasal mucosa is breached, fibroblast activity attempts to heal the breach and if two mucosal surfaces are in contact, a synechia between the two surfaces develops. Ultimately, there is a possibility of contracture and various degrees of stenosis.
Various techniques have been reported in the literature for the repair of nasal vestibular stenosis. Karen et al. reported excellent results by using composite aural graft without any nasal stent.7 Jablon and Hoffman reported a case of nasal vestibular stenosis caused by obstetric forceps they treated by mucosal graft from the hard palate.2 Other suggested reconstructive options include the use of modified Z-plasty skin grafts, local myocutaneous flaps, and septal cartilage flaps, as well as mucosal flaps from the palate and composite cartilage grafts. These all require general or prolonged monitored anesthesia.2,7 Salvado and Wang have reported the use of mitomycin C for the correction of vestibular stenosis by the inhibition of fibroblast proliferation and collagen synthesis as preventive measures.7 While Smith and Roy reported endoscopic lyses of the scar tissue with application of mitomycin C and nasal stent placement.6
In summary, previous strategies as mentioned above focus on correction with local flaps or skin grafts.1,3,5 However, recent literature supports management by endoscopic lysis, mitomycin application and stenting by different tubing, usually modified endotracheal tubes.7,8 The advantages of using V-stent include: a) sparing the patient from prolonged anesthesia, and b) major surgery with a better surgical outcome. Additionally, the stent placement is technically simpler and it provides support to the external and internal nasal valves, and also helps achieve maximal aesthetic and functional results. Because of the inherent spring effect of the V-stent; a gentle pressure is applied to the lateral nasal wall and the septum, thus exerting hemostasis. Placing merocel in the tunnel decreased the risk of septal hematoma by keeping the mucopericondrium in place, and decreasing the dead space.
In our experience, the soft consistency of the stent caused less discomfort to the patient, hence the compliance was better, as children are known to pull out stents if they feel irritated by them. The stents are custom made so the fitting is perfect for the nose, on which it is placed. The cost of such stents is low as many stents can be cut from a single silicone sheet.
Conclusion
In patients with nasal trauma involving the nasal vestibule, and internal and external nasal valves, stent placement avoids sequels; adhesions, contractures, synechia, vestibular stenosis and fibrosis involving these anatomical structures. The advantages of the described V-stents over the traditional readymade ridged nasal stents, tubing’s and composite aural graft are: a) simplicity of use, b) safety, c) less morbidity, d) they tend to be more comfortable, and e) economical. Finally, the initial management of proper referral to a specialist after nasal trauma for suturing of the wound and nasal stenting are very important to get satisfactory cosmetic and functional results, and also to decrease the risk of complications such as vestibular stenosis.
Acknowledgements
To Dr Abdul Aziz Al Azri and M.S Aditi Bhargava for helping with the diagrams. No conflicts of interest declared.
References
1. Corey CL, Most SP. Treatment of nasal obstruction in the posttraumatic nose. Otolaryngol Clin North Am 2009 Jun;42(3):567-578.
2. Jablon JH, Hoffman JF. Birth trauma causing nasal vestibular stenosis. Arch Otolaryngol Head Neck Surg 1997 Sep;123(9):1004-1006.
3. Jatana KR, Oplatek A, Elmaraghy CA. Bilateral vestibular stenosis from nasal continuous positive airway pressure/cannula oxygen administration. Otolaryngol Head Neck Surg 2008 May;138(5):690-691.
4. William E. Walsh, Robert C. Kern Sinonasal Anatomy, Function, and Evaluation. Head & Neck Surgery - Otolaryngology, 4th Edition; Volume One > II - Rhinology and Allergy.
5. Karen M, Chang E, Keen MS. Auricular composite grafting to repair nasal vestibular stenosis. Otolaryngol Head Neck Surg 2000 Apr;122(4):529-532.
6. Smith LP, Roy S. Treatment strategy for iatrogenic nasal vestibular stenosis in young children. Int J Pediatr Otorhinolaryngol 2006 Aug;70(8):1369-1373.
7. Salvado AR, Wang MB. Treatment of complete nasal vestibule stenosis with vestibular stents and mitomycin C. Otolaryngol Head Neck Surg 2008 Jun;138(6):795-796.
8. Menger DJ, Lohuis PJ, Kerssemakers S, Nolst Trenité GJ. Postoperative management of nasal vestibular stenosis: the custom-made vestibular device. Arch Facial Plast Surg 2005 Nov-Dec;7(6):381-386.
|