|
Abstract
Persistent hiccup is a rare but potentially severe condition that can be symptomatic of a variety of diseases or idiopathic. Most episodes last only a few minutes and are self-limited, but hiccup can get persistent and become a real problem for physician and patient alike. The center of hiccup may be activated by a great variety of stimuli travelling along different nerve pathways and bring different effecter responses. We report a case of persistent hiccup as a presentation of impending thyroid storm of Graves’ disease. Though the condition is rare, clinicians should remain alert to the possibility of this diagnosis.
Introduction
Chronic hiccup is defined as an attack lasting longer than 48 hours and, sometimes it can be serious, intractable and exhausting. Persistent Hiccup (PH) is rare and it can be idiopathic or a symptom of a variety of diseases. The hiccup center may be activated by a great variety of stimuli travelling along different nerve pathways and a reflex arc has been proposed, with the phrenic nerves, vagi, and T6-12 sympathetic fibers as the afferent limb.1 The "hiccup centre" is thought to be located in either the brainstem respiratory centre or the cervical cord between segments C3 and C5.2 The efferent limb is the phrenic nerve.3 It has been suggested that hiccups could be a form of myoclonus, caused by repeated and abnormal activity of the solitary inspiratory nucleus.4 We present a case of Graves’ disease which had defaulted with drug treatment and presented with PH. The patient had impending thyroid storm and its treatment resulted in remission of hiccup. We hypothesize that hyperthyroxinemia caused the irritation of the hiccup centre that resolved after taking care of hyperthyroxinemia. This case highlights a rare presentation of severe thyrotoxicosis.
Case Report
A 55 years-old male, chronic smoker, shopkeeper by occupation diagnosed case of Graves’ disease with moderate ophthalmopathy was on our follow-up for the last 12 months. He was stabilized on carbimazole 20 mg a day for two months before the current admission, when he defaulted with the medication. He started with persistent and non responding hiccup for 10 days (i.e. two months after drug withdrawal).
The frequency and intensity of hiccups worsened with time and were almost present throughout the day and night at the time of admission to the emergency room of the hospital. There was no history of drug intake known to cause hiccups, abdominal pain, and chest pain, as well as symptoms pointing to a mass or sepsis in the chest or abdomen.
On examination, the patient was ill looking, confused, disoriented, diaphoretic and moderately emaciated with a BMI of 19.4 Kg/m2. Vitals in ER revealed moderate fever (103.5°F), severe tachycardia (pulse of 122 bpm), and a wide pulse pressure (BP 130/60 mm Hg). He had diffuse, soft to firm thyromegaly with bruit over it. Eye examination revealed that both were hyperadrenergic and mechanical (bilateral proptosis) components of ophthalmopathy were indicative of activity. The rest of the systemic examination was unremarkable.
Investigations revealed normal blood counts, urinalysis, electrocardiography, liver and kidney functions. Electrogastr- odudenoscopy, chest roentgenography, Ultrasonography (USG) of the abdomen, Contrast Enhanced Computed Tomography (CECT) of the brain were normal. USG of the thyroid showed diffuse enlargement with no nodules. Thyroid functions tests revealed very high tri-iodothyronine and L thyroxine levels with undetectable TSH. (Table 1)
Table 1: Serial thyroid function tests
| Investigation |
Zero week |
1st week |
3rd week |
10th week |
Normal range |
| T3 |
4.04 |
1.82 |
1.41 |
0.03 |
00.70-02.50 ng/ml |
| T4 |
12.71 |
12.13 |
11.25 |
9.28 |
05.50-13.50 ug/dl |
| TSH |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
00.50-06.50 UIu/ml |
The patient was treated for impending thyroid storm with external cooling, intravenous fluids, and carbimazole 60 mg/day in divided doses, 100 mg of IV hydrocortisone eight hourly and beta blockers. The clinical condition improved and the hiccups decreased in frequency and intensity, until they stopped on the third day of admission. On enquiry, the patient gave similar history of mild hiccup at the first diagnosis of Graves’ disease which had resolved after anti-thyroid treatment. He was discharged on carbimazole after two weeks of inpatient care and is currently euthyroid and under consideration for radioiodine ablation as definitive therapy. (Fig. 1)
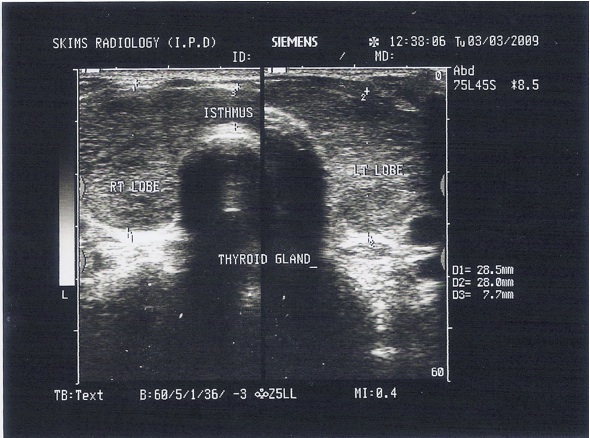
Figure 1: USD Thyroid showing diffuse enlargement of the thyroid.
Discussion
Hiccups are an involuntary spasmodic and coordinated contractions of the inspiratory muscles associated with a delayed and sudden closure of the glottis which is responsible for the characteristic noise.1Hiccups are a common benign disorder, which are usually transient. Occasionally, hiccups fail to resolve spontaneously, resulting in patient fatigue, incapacitation and the need for the affected individual to seek medical care in order to resolve the problem.
The approach to the management of these patients consists of the identification and treatment of serious underlying causes of the episode as well as therapeutic interventions to achieve hiccup resolution. Chronic Persistent hiccup is defined as one lasting more than 48 hours, which is uncommon, and Graves’ disease presenting with hiccup is rare.5 It can be serious, intractable, and exhausting, and its cause often obscure. It may indicate multiple neurologic and extra neurologic disorders such as brain tumor, strokes, myocardial infarction, renal failure, prostate cancer, or abdominal surgery.
Psychogenic causes (excitement, stress) may also elicit hiccups. Detailed medical history and physical examinations will often guide diagnostic investigations (abdominal ultrasound, chest or brain CT scan). Gastric and duodenal ulcers, gastritis, esophageal reflux and esophagitis are commonly observed in chronic hiccup patients and upper gastrointestinal investigations such as; endoscopy, pH monitoring and manometry should be included in the diagnostic evaluation systematically.
Most episodes of hiccup are associated with acute gastric distention and alcohol ingestion, but these are short lived and resolve spontaneously.6 Etiological treatment is not always available and chronic hiccup treatment has classically relied on metoclopramide and chlorpromazine. Recently, baclofen has emerged as a safe and often effective treatment.5 To the best of our knowledge; this is the first case which highlights hiccup as one of the rare presentations of thyrotoxicosis.
In this report, we attempted to rule out most of the usual causes of hiccup and most of the evaluation was negative. We assume that irritation of the hiccup centre by high levels of thyroxine resulted in persistent hiccup since it was the treatment of thyrotoxicosis, which resulted in its resolution. It was not the steroid effect as he continued with hiccups even on steroids, and by day three, the hiccups stopped completely, which also corresponds to the normalization of serum T3 levels. Also, the fact that the patient had no recurrence of the symptoms in the euthyroid state and no other cause was evident after a long follow up of 18 months further confirmed our hypothesis.
Conclusion
We report this case to highlight this rare presentation of thyroid storm/severe thyrotoxicosis. It emphasizes to practitioners that it is important to thoroughly investigate a case of hiccup to identify any underlying pathological cause with due consideration to hyperthyroxinemia/thyroid storm as in this case.
Acknowledgements
The authors reported no conflict of interest and no funding was received on this work.
|