A two-year-old male presented to the surgical outpatient department of the Armed Forces Hospital, Muscat, with penile shaft swelling, which had been present for 10 months. He had no history of trauma, but had undergone circumcision one year prior and the swelling had developed after the procedure. He was referred to a urologist for further management.
Clinical examination showed a soft swelling arising from the left lateral aspect of the penile shaft. Based on a presumptive diagnosis of soft tissue mass (fibroma), the swelling was excised and sent for histopathological assessment [Figure 1]. The specimen was a soft cystic nodule measuring 1cm.
Questions
1. What is the histological diagnosis?
2. What is the best treatment option?
Answers
1. Microscopy showed the cyst wall lined by histiocytes with giant cells and cholesterol clefts. The cavity contained lamellated keratin with desquamated squamous epithelium. A diagnosis of epidermal inclusion cyst of the penile shaft with granulomatous response to keratin was made.
2. Complete excision. This is a commonly diagnosed condition among the specimens submitted for histopathological examination.
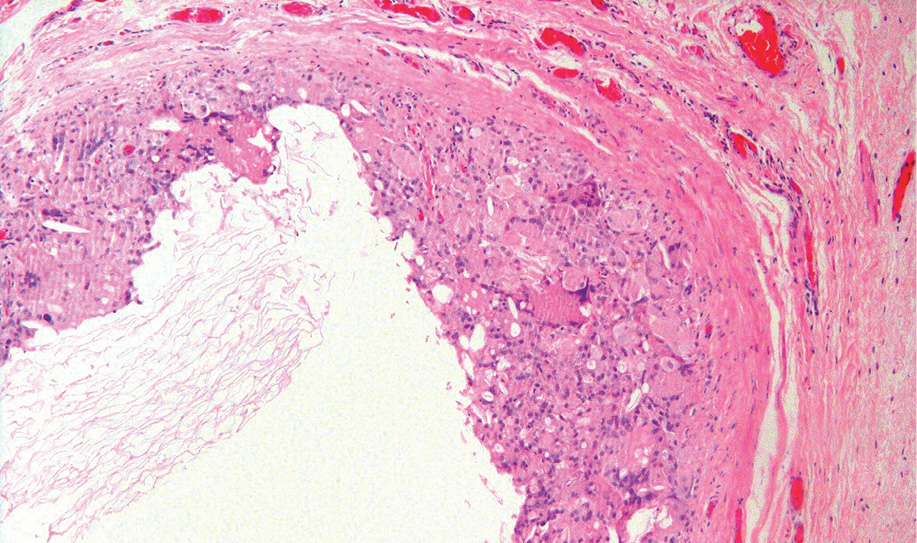
Figure 1: Hematoxylin and eosin staining showed cyst wall lined by histiocytes, cholesterol clefts, and giant cells with luminal keratin. Magnification=10×.
Discussion
Epidermal inclusion cyst is also known by other interchangeable terminologies like epidermal cyst and epidermoid cyst.1 The cyst arises from the infundibular part of the hair follicles.2 It is a benign condition that can develop in any part of the body. However, involvement of the penis is rare and is a late complication of neonatal circumcision.3
Complications of male circumcision are rare considering the number of procedures performed, and are classified as early or late. Bleeding, wound infection, retention of urine, and penile or urethral injury are early complications. Late complications include phimosis, shortage of preputial skin, penile curvature, lymphedema, and inclusion cysts. A recent meta-analysis has shown that the complication rate ranges from 0% to 16% with a median rate of 2%.4 A one year survey of neonatal circumcision in Israel, noted a complication rate of 0.3%. 5
The etiology of epidermal cysts is unknown and they can be either congenital or acquired.1 Abnormal embryologic closure of the median raphe is believed to be responsible for the congenital cases while acquired cases are the result of mechanical implantation and proliferation of the epidermal elements in the dermis.1,6 These cysts have been reported following repair of hypospadias, penile girth enhancement procedures, and circumcision due to the accidental sequestration of the epidermis into the dermis. They usually present as a painless swelling and treatment is mainly for cosmetic correction and other indications including secondary infection, difficulty during intercourse, or urinary obstruction. El-Shazly et al,6 reported a long-standing neglected case that resulted in stone formation and ureterocutaneous fistula, which was treated successfully with complete excision and repair of the fistula.
Differential diagnoses to be considered are urethral diverticula and keloids.4 A voiding cystourethrogram can eliminate the possibility of a diverticulum whereas a keloid can be determined through histopathology. Diagnosis requires careful physical examination and radiological evaluation. Treatment is simple, complete excision of the cyst. However, aspiration and drainage are not recommended as the cyst may recur, although recurrence can also be due to incomplete excision. Malignant transformation of the epithelium has been reported rarely in cysts occurring at other sites, but not in penile cysts.
Disclosure
The authors declared no conflict of interests.
references
- Aslan Y, Balci M, Atan A. Idiopathic penile epidermoid cyst in a young patient: three year follow-up. Eur J Surg Sci 2011;2(1):16-18.
- Kaviani A, Hosseini J, Vazirnia AR. A huge penile mass which turned out to be an epidermoid inclusion cyst. Urol J 2009;6(2):135-137.
- Saini P, Mansoor MN, Jalali S, Sharma A. Penile epidermal inclusion cyst. Indian J Pediatr 2010 Jul;77(7):815-816.
- Tuli S, Meinert E, Kelly M, Tuli S. Epidermal inclusion cyst after circumcision. Consultant for pediatricians 2012 April;11(4). Available at http://www.pediatricsconsultant360.com/content/epidermal-inclusion-cyst-after-circumcision#. Accessed 25 May 2015.
- Ben Chaim J, Livne PM, Binyamini J, Hardak B, Ben-Meir D, Mor Y. Complications of circumcision in Israel: a one year multicenter survey. Isr Med Assoc J 2005 Jun;7(6):368-370.
- El-Shazly M, Ghosbashy A, Allam A, Alenezy T, Alenezy N, Yordanov E, et al. Penile epidermal inclusion cyst. Case Rep Urol 2012;2012:191343.