| |
Abstract
Objective: The objective of the present study is to determine the incidence of delirium and the associated factors in patients undergoing open heart surgery.
Methods: This is an Analytic-descriptive study conducted on 404 patients undergoing elective open heart surgery in Fatemeh Zahra Heart Center, Sari, over the period of 6 months from July to December 2011. Sampling was achieved in a nonrandomized targeted manner and delirium was assessed using NeeCham questionnaire. A trained nurse evaluated the patients for delirium and completed the risk factor checklist on days 1 to 5 after surgery. Data analyses were accomplished using survival analysis (Kaplan-Meier and Cox regression) on SPSS software version 15.
Results: We found that variables, including ventilation time, increased drainage during the first 24 hours, the need for re-operation in the first 24 hours, dysrhythmias, use of inotropic agents, increased use of analgesics, increased arterial carbon dioxide, lack of visitors, and use of physical restrainers were associated with the development of delirium. In addition, we found a delirium incidence of 29%.
Conclusion: Diagnosis of cognitive disorders is of utmost value; therefore, further studies are required to clarify the risk factors because controlling them will help prevent delirium.
Keywords: Delirium; Heart surgery; NeeCham Confusion scale; Cognitive impairment.
Introduction
According to the Diagnostic and Statistical Manual of Mental Disorders-IV-Text Revision (DSM-IV-TR), delirium is a cognitive and consciousness disorder which develops over a short period and has certain features such as decreased level of consciousness, attention disorders (e.g. loss of concentration and memory), orientation disorder, rapid onset (a few hours to a few days), short duration, and prominent fluctuation.1 Delirium in admitted patients is associated with increased mortality,1-7 increased hospital stay,1,4,5,7-10 high hospital costs,1,2,4,6-8 compromise of patient rehabilitation,1,8 increased duration of intubation,5,9 very poor quality of life,6,10 and long-term care.11 Delirium leads to a threefold increase in the mortality risk,9 mostly are related to cardiac surgery (7%-34%, even as high as 90%), orthopedics (18%-50%), and intensive care unit (16%-83%).1 It is often manifested in three modes: hyperactive, hypoactive, and mixed. Hyperactive delirium, which is easily recognized, is accompanied by symptoms such as irritability in behavior, hallucination and delusion. On the other hand, hypoactive delirium is presented by withdrawal symptoms, decreased attention, and decreased motor activity. Symptoms of hallucination and delusion are less common and require more care. It is very difficult to diagnose and usually mistaken for depression, fatigue, and dementia.1,2,4,6-8 Symptoms of mixed delirium occur in both groups and are more common than the two others.1-7
Delirium most frequently occurs in the 2nd to 7th days after the surgery,12 and most related behavioral and mental changes arise during the first 3 days after the surgery. Cardiac surgery is increasing worldwide, and numerous cases of mental disorders have been reported to be associated with it. For example, although the etiology of post-surgical delirium is unknown, many risk factors have been distinguished that affect different patients differently.13 Since nurses are in close contact with the patients, they would able to observe and report the behavioral changes due to delirium fluctuations.14 Factors influencing the occurrence of post-surgical delirium include hematocrit levels of lower than 30%,12,15 reduced cardiac output,12,16-18 use of balloon pump, use of inotropic medication,16 intubation more than 24 hours, need for re-surgery, post-surgical dysrhythmias, infusion of more than 4 units of packed red cells, infusion of more than one unit of fresh frozen plasma, carbon dioxide level of more than 45 mmHg, more than 60 mmHg decrease in the arterial oxygen level, elevated blood sugar, reduced blood sugar, elevated temperature, and increased serum sodium, and urea levels.19
As few studies have been conducted in Iran concerning delirium and its associated factors in cardiac surgery; therefore, the present study was undertaken to determine the incidence of delirium after open heart surgery and the associated risk factors. It was started by determining the incidence of delirium using NeeCham questionnaire, and then followed by evaluating post-surgical risk factors.
Methods
This is an analytic-descriptive study conducted on 404 patients, whom underwent elective open heart surgery in Fatemeh Zahra Heart Center, Sari, over 6 months spanning from July to December 2011. We calculated the sample size with a confidence interval of 95% and a mean prevalence of 50% (10%-90%),1,12,19,20 that obtained 404. Sampling was performed in a nonrandomized targeted manner. The inclusion criteria were elective open heart surgery (due to the need for primary evaluation for delirium prior to surgery) and age of over 18 years. The exclusion criteria were delirium on entering into the study, deafness, blindness, and aphasia, which made the patients unable to complete the questionnaire.
Patients were assessed for delirium by NeeCham questionnaire, which is a screening instrument for nurses to evaluate the patient’s behavior rapidly at bed-side.21-23 This questionnaire is based on the criteria of DSM-III-R,21-23 and consists of three major subscales: information processing (attention, command, and processing orientation, scored 0-14), behavior (general appearance and posture, sensory motor performance, and verbal response, scored 0-10), and physiologic control (vital signs, oxygen saturation level, and urinary continence control, scored 0-6). It yields a total score of 30 points. The patient will be categorized under any of the following four groups according to the score he/she obtains: healthy (27-30 points); stupor (25-26 points); mild delirium (20-24 points); and severe delirium (0-19 points). In addition, the questionnaire displays high sensitivity and specificity. Completing the questionnaire takes 8-10 minutes, so it is not demanding on the nurse because it can be completed during the routine activities and observations of a nurse. Therefore, the questionnaire is a reliable tool for the assessment of delirium by nurses in the public wards. It has been recently used on non-intubated patients in intensive care units and the results of comparing the diagnostic power of the two questionnaires, namely, CAM-ICU and NeeCham, on 172 non-intubated patients admitted to a general intensive care unit revealed that NeeCham identified delirium better than CAM-ICU. The result of this study indicated 87% sensitivity and 95% specificity for NeeCham.23 The criteria in this study for tool selection were its high sensitivity and specificity, its appropriateness for critically ill and non-intubated patients, and its simple application by a nurse.
On the evening preceding the surgery day, all patients were evaluated by a psychiatrist to rule out primary delirium. Since the patients had to stay on intubation and receive sedative, the first 24 hours after the surgery was not considered. First day after the surgery, the patient who was rousable and non-intubated in the previous evening was assessed for delirium. A trained nurse evaluated the patients from day 1 to 5 after the surgery once a day. Due to the increased incidence of delirium in the afternoon and evening,1 the assessment was performed from 16:00 to 20:00. Selection of patients was done by nurses who were trained and informed about the inclusion and exclusion criteria. A checklist of post-surgical factors and demographic information was completed for each patient. Due to ethical considerations, any patient with symptoms of delirium would be reported to the head of the ward for treatment.
We used descriptive statistics (percentage, mean, median, and mode) to describe the variables related to the patients and the incidence of delirium, and survival analyses (Kaplan-Meier and Cox regression) were performed to determine the risk factors for delirium. All tests were performed on SPSS software version 15.
Results
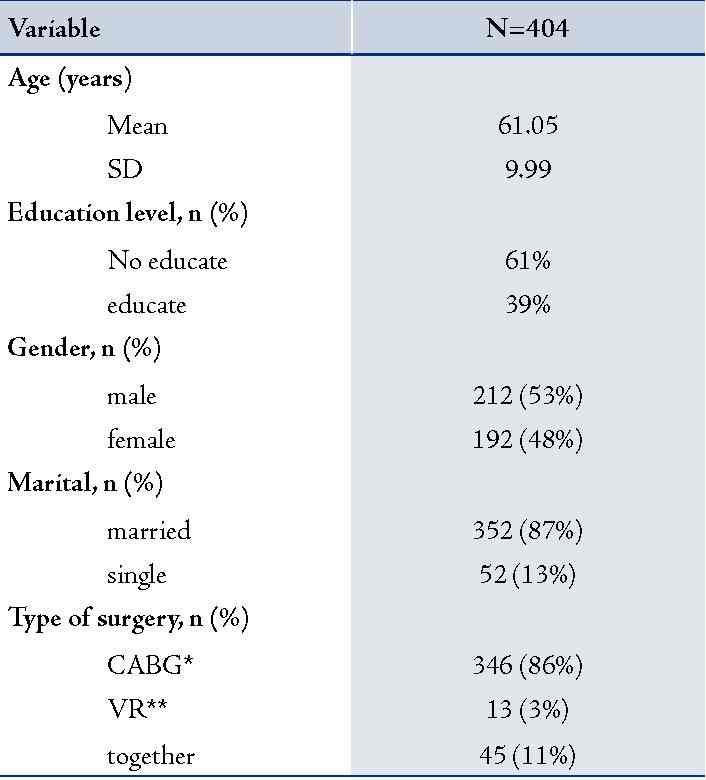
We found an incidence of 29% for post-surgical delirium. The patients’ age ranged from 35-85 years and most frequently belonged to the 56-60 year age group ([20%] 79 patients). Among the patients, 48% were women and 53% were men. Of these patients, 86% underwent CABG, 3% valve replacement, and 11% with both.
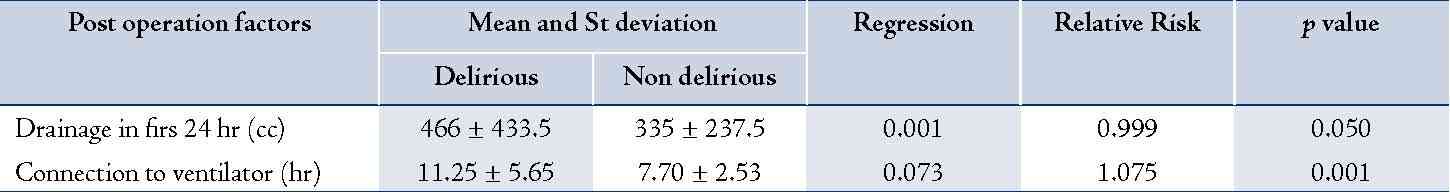
Table 1 represents demographic information of the variables, and Table 2 and 3 represent the post-surgical factors and their relationship with delirium.
Table 1: Information of Demographic.
In this study, a few things were taken into consideration such as ventilator time, need for re-surgery, drainage during the first 24 hours after the surgery, need for inotropes, increased arterial carbon dioxide, Arrhythmias that require intervention care, need for analgesic, using of restrainers (handcuffs and shackles) and visitors with post-surgical delirium (p-value <0.050).
Table 2: Post operation factors associated with delirium with using test of Kaplan Meier.
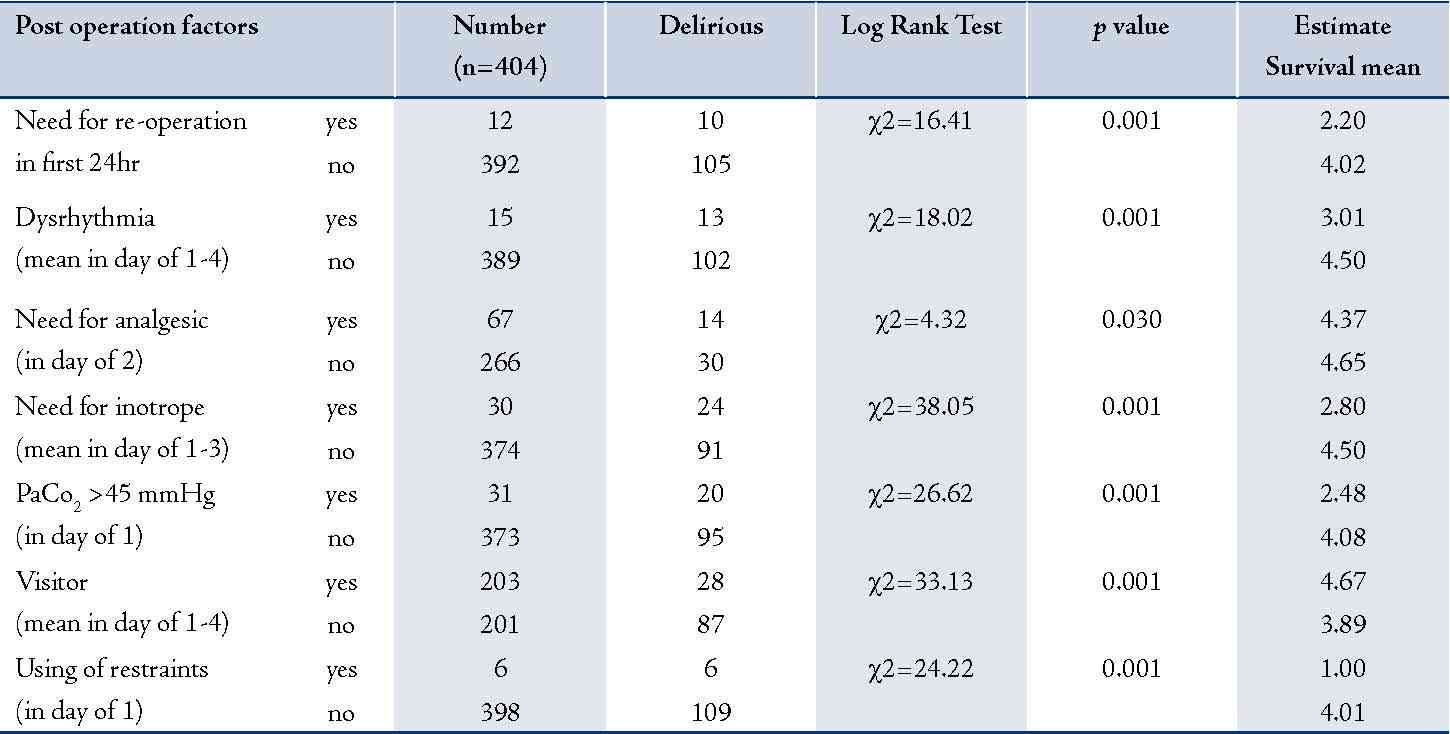
Table 3: Calculation of Relative Risk of post operation factors associated with delirium with using test of Cox Regression.
Discussion
According to these findings, delirium occurred most frequently in the first day after the surgery and no patient had delirium on the fifth day and most patients were afflicted with mild delirium. Different studies have reported the incidence of delirium to be 90%,1 47%,12 46%,24 32%,25 16%,19 and 10%.20 These discrepancies may reflect the difference in sample size, delirium assessment tools, study environments, and timing of evaluations.
In this study, we evaluated the post-surgical variables of ventilator time, need for re-surgery during the first 24 hours, drainage during the first 24 hours, blood pressure, temperature, biochemical variables (hemoglobin, serum urea, serum sodium, and serum glucose), drain secretions on the subsequent days, arterial blood gas analysis (pH, decreased arterial oxygen, increased arterial carbon dioxide), infusion of blood products, need for analgesics, need for inotropes, visitors and physical restrainers after surgery.
Our findings indicated that patients who developed delirium were on average intubated for a longer time compared to those who did not. Furthermore, the relationship between ventilator time and delirium was found statistically significant (p=0.001). We also found that the relative risk of delirium increased by 8% with each hour of ventilator time (Table 3). Long term intubation, which affects the cerebral function, may be the result of poor physical conditions, respiratory failure, or overuse of muscle relaxants and anesthetics. Hypoxia during surgery may be associated with cerebral ischemia and development of cognitive disorders.19 Findings of this study, in which the average intubation time was 11 hours and 25 minutes, corroborate those of previous studies. For example, a previous study suggests that intubation more than 24 hours is directly related to the development of delirium.19 Another study reports a relationship between delirium and mechanical ventilation of more than 6 hours.24
Most patients in this study followed a natural course after surgery and did not require re-surgery (97%). On the other hand, those who were indicated for re-surgery during the first 24 hours had higher incidences of delirium (80% vs. 27%), and the difference was statistically significant (p=0.001) (table 2). This is consistent with findings of a previous study on delirium after cardiac surgery.19
We found that the drainage of patients who developed delirium was more than the others during the first 24 hours after the surgery, and the difference was found to be statistically significant. Each cc increase in drainage raised the relative risk of delirium by 100% in a direct fashion (Table 3). Another study mentions that the drainage in the first 24 hours after surgery is directly related to the development of delirium.24 Our findings revealed that hemorrhage, during and after surgical procedures followed by infusion of sanguine products, was associated with increased risk of delirium, the mechanism of which is not clear. Nevertheless, a study on animal models suggests that hemorrhage initiates a stress response which activates the hypothalamus, leading to cortisol release. This chemical imbalance can have an influence on the incidence of cognitive impairment.26
Most studies report reduced cardiac output as a factor influencing delirium, which may be associated with increased use of inotropic agents, or other auxiliary instruments such as balloon pump.12,16-18 We measured the systolic and diastolic blood pressure of patients, and found no significant difference between patients who developed delirium and those who did not. This may be due to the fact that the use of inotropic medication keeps the blood pressure within normal range when the patients are evaluated. On the other hand, use of inotropes (mostly on days 1 to 3 after surgery) was significantly associated with increased risk of delirium (Table 2). This is in line with findings of most previous studies.12,16-18
There was no significant relationship found between delirium and body temperature. All patients had almost normal temperature readings during the few days after the surgery (36.86 ± 0.26, average of temperature in non-delirium patients vs. 36.90 ± 0.23, in delirium patients). Only one study refers to a relationship between delirium and increased body temperature over 38¼C.19 This may be because we administered prophylactic antibiotics to prevent the infection of the site of incision and drains, as well as oral acetaminophen (4 times a day) for pain relief and this may have reduced fever in our patients.
Other influential factors include hemoglobin level and infusion of packed red cells. The hemoglobin level of patients who developed delirium in this study was lower than the others; however, the difference was not statistically significant (9.45 ± 1.1, average of hemoglobin in non-delirium patients vs. 9.30 ± 0.83, in delirium patients). Patients were infused with packed red cells on different days based on their hemoglobin level, yet no relationship was found between infusion of blood products and delirium. In contrast, a previous study reports that infusion of more than 4 units of packed red cells per day is associated with increased risk of delirium.19 The discrepancy might be due to the fact that the patients received one unit of blood product per day and probably had less blood loss.
Increased (>300 mg/dl) and decreased (<50 mg/dl) serum glucose levels may both lead to post-surgical delirium.19 The glucose level of our patients was more or less in the normal range, and we found no significant relationship between glucose level and delirium. This may have been due to the fact that blood glucose levels of our patients all fell within the 134-193 mg/dl range (161.37 ± 57.33, average of serum glucose level in non-delirium patients vs. 161.93 ± 55.45, in delirium patients).
It has been found that increased serum urea level (>50 mg/dl) is associated with post-surgical delirium.19 Among the patients, those who developed delirium had higher levels of serum urea on all days of evaluation. The difference, however, was statistically insignificant which may have been due to the fact that serum urea levels in our study never fell out of the 18-37 mg/dl range (20.46 ± 5.82, average of serum urea level in non-delirium patients vs. 29.78 ± 10.95, in delirium patients).
During the evaluation period, patients who developed delirium yielded higher levels of serum sodium. Nonetheless, the sodium levels remained within normal ranges and no significant relationship was found between sodium level and delirium. One study reports that increased serum sodium (>150 mg/dl) is associated with increased risk of delirium,19 while we found that the sodium level ranged from 137 to 139 mg/dl, which was within normal range (136.99 ± 1.1, average of sodium level in non-delirium patients vs. 138.85 ± 3.67, in delirium patients).
Arterial blood gas analysis was conducted for all patients on the first few days after the surgery. The pH levels remained normal in all days and were not found to be significantly related to delirium. Only on the first day of evaluation, patients who developed delirium were found to have lower arterial oxygen and higher arterial carbon dioxide levels. Nevertheless, only the relationship between increased arterial carbon dioxide and delirium was significant and that of decreased arterial oxygen and delirium remained insignificant (Table 2). One study reports a significant relationship between delirium and pH level, that is, increased arterial carbon dioxide (>45 mmHg) and decreased arterial oxygen (<60 mmHg).19
Atrial fibrillation was the most common type of dysrhythmias among the patients, particularly those who developed delirium. No patient had dysrhythmias on the fifth day. We found a statistically significant relationship between dysrhythmias (Arrhythmias that require intervention care) and delirium (Table 2). Similarly, other studies have found that cardiac dysrhythmias, especially ventricular arrhythmias, are associated with increased risk of post-surgical mortality and delirium. Atrial fibrillation is the most frequent type of dysrhythmias following heart surgery,24 and atrial fibrillation may lead to delirium through cerebral embolism and compromised brain tissue perfusion.19
A significant relationship was revealed between delirium and analgesic use only on the second day (Table 2). The greatest and smallest amounts of analgesics used pertained to days one and five of the study, respectively. Although the patients used less analgesics on the second day compared to the first day, they experienced more delirium in the former. Normally, when an intubated patient is secluded from the surroundings and suffers from pain, he/she may show signs of agitation. Moreover, the elderly patients may have certain background conditions such as arthritis, discopathies, and knee problems, all of which add to the pain. On the other hand, persistent pain leads to increased catecholamine activity, myocardial ischemia, increased metabolism, sleep disorders, anxiety and delirium. Unless properly managed, pain will leave many nervous complications. Therefore, patients who undergo surgery experience pain from many sources, including incision site, catheters, tracheal tubes, repeated suctions, being bedbound, and muscular weakness.27 Although persistent pain control may reduce the severity of delirium, it does not have any impact on its incidence.28 Moreover, the adverse effects of analgesics and spasmolytics themselves may play a role in the development of delirium or aggravate it through respiratory suppression.29
In this study, restrainers (handcuffs and shackles) were used for agitated patients only on the first day, and it was associated with 100% delirium, which is statistically significant (Table 2). Most resources in the literature mention an increase in the risk of delirium with the use of physical restrainers.1,30,31 It has been found that an admitted patient encounters many stimuli which differ from what he/she is accustomed to, resulting in sensory changes such as increased sensory stimulation, and sensory and sleep deprivation. Increased sensory stimulation refers to the state of augmented stimulation when the brain fails to respond properly, and it depends on the patient’s personality, age, culture, and lifestyle. Sensory deprivation represents the state of reduced sensory stimulation or monotonous stimulation, which manifests as disorders of comprehension, cognition and memory.32
Patients who did not have any visitors during the first 4 days after the surgery were significantly more at risk of delirium (Table 2). On the fifth day, none of the patients without visitor experienced delirium. Other studies demonstrated that sensory deprivation occurs through lack of stimulation from the environment (loneliness, isolation, lack of visitors, complete bed rest), disorders of receiving stimuli from the environment (auditory or visual disorders, wound dressing which eliminates palpation, motion disorders, use of restrainers), or disorders of sensory transmission (spinal lesions, confusion, medication suppressing the central nervous system).33 This finding is in line with another study which mentioned lack of visitors as a risk factor for development of delirium.30
Prevention or early recognition of delirium is important since delirium correlates with a prolonged hospital stay, nursing home placement, reduced cognitive and functional recovery, and increased morbidity and mortality. In patients who undergo cardiac surgery, delirium is associated with more postoperative complications. In addition, patients with postoperative delirium are more prone to have postoperative respiratory insufficiency; they have a significantly higher prevalence of sternum instability and are more likely to require surgical revision of the sternal wound.34 The risk factors found in this study help identify the patients who are susceptible to postoperative delirium, as a result, appropriate action can be taken in the proper time. Regarding the early recognition and/or detection of delirium in hospitalized medically ill patients, nurses—who spend more time at the patients’ bedside—play a crucial role and knowing these risk factors can reduce the incidence of delirium.
Conclusion
In this study, intubation time, need for re-surgery during the first 24 hours, drainage during the first 24 hours, occurrence of dysrhythmias, use of inotropes, increased use of analgesics, elevated arterial carbon dioxide level, lack of visitors and use of physical restrainers (p<0.050) were significantly associated with post-surgical delirium. In patients with high risk of developing delirium, it may not be possible to prevent it, but its early recognition can be beneficial. Thus, risk factors found in this study can be considered by means of systematic observations of the patients’ behavior. This ensures that patients can be treated efficiently and the postoperative morbidity and mortality can thereby be reduced.34
Acknowledgements
The authors reported no conflict of interest and no funding was received on this work.
References
1. DeLeo FR, Otto M, Kreiswirth BN, Chambers HF. Community-associated meticillin-resistant Staphylococcus aureus. Lancet 2010 May;375(9725):1557-1568.
2. Howden BP, Davies JK, Johnson PD, Stinear TP, Grayson ML. Reduced vancomycin susceptibility in Staphylococcus aureus, including vancomycin-intermediate and heterogeneous vancomycin-intermediate strains: resistance mechanisms, laboratory detection, and clinical implications. Clin Microbiol Rev 2010 Jan;23(1):99-139.
3. Jevons MP. ‘‘Celbenin’’-resistant Staphylococci. BMJ 1961;1:124-125 .
4. Deresinski S. Methicillin-resistant Staphylococcus aureus: an evolutionary, epidemiologic, and therapeutic odyssey. Clin Infect Dis 2005 Feb;40(4):562-573.
5. Hiramatsu K, Hanaki H, Ino T, Yabuta K, Oguri T, Tenover FC. Methicillin-resistant Staphylococcus aureus clinical strain with reduced vancomycin susceptibility. J Antimicrob Chemother 1997 Jul;40(1):135-136.
6. Chang S, Sievert DM, Hageman JC, Boulton ML, Tenover FC, Downes FP, et al; Vancomycin-Resistant Staphylococcus aureus Investigative Team. Infection with vancomycin-resistant Staphylococcus aureus containing the vanA resistance gene. N Engl J Med 2003 Apr;348(14):1342-1347.
7. Askari E, Tabatabai SM, Arianpoor A, Naderi Nasab M. VanA-positive vancomycin–resistant Staphylococcus aureus: systematic search and review of reported cases. Infect Dis Clin Pract 2013;21:91-93 .
8. Aligholi M, Emaneini M, Jabalameli F, Shahsavan S, Dabiri H, Sedaght H. Emergence of high-level vancomycin-resistant Staphylococcus aureus in the Imam Khomeini Hospital in Tehran. Med Princ Pract 2008;17(5):432-434.
9. Dezfulian A, Aslani MM, Oskoui M, Farrokh P, Azimirad M, Dabiri H, et al. Identification and characterization of a high vancomycin-resistant Staphylococcus aureus harboring vanA gene cluster isolated from diabetic foot ulcer. Iran J Basic Med Sci 2012 Mar;15(2):803-806.
10. Azimian A, Havaei SA, Fazeli H, Naderi M, Ghazvini K, Samiee SM, et al. Genetic characterization of a vancomycin-resistant Staphylococcus aureus isolate from the respiratory tract of a patient in a university hospital in northeastern Iran. J Clin Microbiol 2012 Nov;50(11):3581-3585.
11. Bannerman TL. Staphylococcus, Micrococcus, and other catalase positive cocci that grow aerobically. In: Murray PR, Baron EJ, Jorgensen JH, Pfaller MA, Yolken RH, ed. Manual of clinical microbiology. ASM Press: Washington DC, 2003; 8: 384–404.
12. Brakstad OG, Aasbakk K, Maeland JA. Detection of Staphylococcus aureus by polymerase chain reaction amplification of the nuc gene. J Clin Microbiol 1992 Jul;30(7):1654-1660.
13. Clinical and Laboratory Standards Institute. 2011. Performance standards for antimicrobial susceptibility testing, 21st informational supplement. CLSI document M100-S21. Clinical and Laboratory Standards Institute, Wayne, PA.
14. Clinical and Laboratory Standards Institute. 2012. Performance standards for antimicrobial disk susceptibility tests. Approved standard, 11th ed. CLSI document M02-A11. Clinical and Laboratory Standards Institute, Wayne, PA.
15. Clark NC, Cooksey RC, Hill BC, Swenson JM, Tenover FC. Characterization of glycopeptide-resistant enterococci from U.S. hospitals. Antimicrob Agents Chemother 1993 Nov;37(11):2311-2317.
16. Willems RJ, Top J, van Schaik W, Leavis H, Bonten M, Sirén J, et al. Restricted gene flow among hospital subpopulations of Enterococcus faecium. MBio 2012;3(4):e00151-e12.
17. Périchon B, Courvalin P. Glycopeptide resistance, In: Dougherty TJ, Pucci MJ, editors. Antibiotic discovery and development. New York, US: Springer; 2012. p. 515-542.
18. Melo-Cristino J, Resina C, Manuel V, Lito L, Ramirez M. First case of infection with vancomycin-resistant Staphylococcus aureus in Europe. Lancet 2013 Jul;382(9888):205. .
19. ProMED-mail. Staphylococcus aureus, MRSA - Brazil: (SP) vancomycin resistant (VRSA). ProMED-mail 2013; 30 Jun: 20130630.1800166. Available at: http://www.promedmail.org/direct.php?id=20130630.1800166. Accessed July 26 2013.
20. Banerjee T, Anupurba S. Colonization with vancomycin-intermediate Staphylococcus aureus strains containing the vanA resistance gene in a tertiary-care center in north India. J Clin Microbiol 2012 May;50(5):1730-1732.
21. Chakraborty SP. KarMahapatra S, Bal M, Roy S. Isolation and identification of vancomycin resistant Staphylococcus aureus from post operative pus sample. Am J Med Sci 2011;4:152-168.
22. Saravolatz LD, Pawlak J, Johnson L, Bonilla H, Saravolatz LD II, Fakih MG, et al. In vitro activities of LTX-109, a synthetic antimicrobial peptide, against methicillin-resistant, vancomycin-intermediate, vancomycin-resistant, daptomycin-nonsusceptible, and linezolid-nonsusceptible Staphylococcus aureus. Antimicrob Agents Chemother 2012 Aug;56(8):4478-4482.
23. Gould IM. Clinical activity of anti-Gram-positive agents against methicillin-resistant Staphylococcus aureus. J Antimicrob Chemother 2011 May;66(Suppl 4):iv17-iv21.
24. Saha B, Singh AK, Ghosh A, Bal M. Identification and characterization of a vancomycin-resistant Staphylococcus aureus isolated from Kolkata (South Asia). J Med Microbiol 2008 Jan;57(Pt 1):72-79.
25. Alzolibani AA, Al Robaee AA, Al Shobaili HA, Bilal JA, Issa Ahmad M, Bin Saif G. Documentation of vancomycin-resistant Staphylococcus aureus (VRSA) among children with atopic dermatitis in the Qassim region, Saudi Arabia. Acta Dermatovenerol Alp Pannonica Adriat 2012 Sep;21(3):51-53.
26. Al-Yaqoubi M, Elhag K. Susceptibilities of common bacterial isolates from oman to old and new antibiotics. Oman Med J 2008 Jul;23(3):173-178.
27. Hamid ME, Mustafa FY, Alwaily A, Abdelrahman S, Al Azragi T. Prevalence of bacterial pathogens in Aseer region, Kingdom of Saudi Arabia: emphasis on antimicrobial susceptibility of Staphylococcus aureus. Oman Med J 2011 Sep;26(5):368-370.
|