|
Abstract
Multivessel coronary spasm resulting to cardiogenic shock and malignant ventricular arrhythmias though rare has been reported in the literature. The disease seems to be more prevalent in Asians. There have been isolated reports of coronary spasm in patients with reactive airway disease. We report the first case of spontaneous multivessel spasm in a male patient with bronchial asthma of Arab ethnicity resulting in acute myocardial infarction complicated by cardiogenic shock, recurrent ventricular arrhythmias, and transient complete heart block. Literature review of similar cases suggests a strong association with bronchial asthma and a more malignant course in patients with reactive airway disease. The role of intracoronary nitroglycerin in proving the diagnosis even in patients in shock on maximal inotropic supports and intra-aortic balloon pump is highlighted and the importance of considering multivessel coronary spasm as a cause for acute coronary syndrome even in patients with conventional risk factors for atherosclerotic coronary artery disease is reinforced in the discussion of this case.
Keywords: Acute coronary syndrome; Cardiac arrest; Asthma.
Introduction
Multivessel coronary spasm presenting with acute myocardial infarction complicated by complete heart block or recurrent ventricular fibrillation and cardiogenic shock though rare has been reported previously.1-4 Racial heterogeneity has been suggested in the frequency and presentation of patients with coronary spasm.5,6 Bronchial asthma may be a concomitant co-morbidity, which portends a more malignant course in such cases.3,4 Acute myocardial infarction complicated with cardiogenic shock has high mortality.3,7 We report the first case involving an Arab with spontaneous malignant multivessel coronary spasm.
Case Report
A 54-year-old male with previous history of inferior wall myocardial infarction and recurrent chest pain was referred to our institute for an elective angiogram. Other co-morbidities included diabetes mellitus and long standing bronchial asthma on treatment with long acting bronchodilator and steroid inhalers. He had undergone angiogram and angioplasty elsewhere in the past, the details of which were not available at the time of catheterization.
He developed acute onset chest pain with bradycardia and an electrocardiogram (ECG) (Fig. 1A) revealed an acute inferior + right ventricular wall myocardial infarction with complete heart block and junctional escape rate of 40 beats per minute. His blood pressure was 100/60 mmHg. He was transferred to the catheterization laboratory for primary percutaneous coronary intervention within 45 minutes of onset of his symptoms since the patient was already admitted in the cardiac ward. Transvenous right ventricular pacing was instituted at demand rate of 70 per minute, since the complete heart block persisted despite intravenous atropine. The left coronary angiogram revealed severe narrowing of the distal left anterior descending artery (LAD) and multiple tandem lesions of 80-90% in a large circumflex artery (LCX). Right coronary angiogram revealed dominant right coronary artery (RCA) with moderate narrowing’s in the proximal and mid segment with severe stenosis distally before the crux. The posterior descending branch (PDA) and postero-lateral branch (PLB) of the RCA had TIMI 1 flow. (Fig. 2: Panel A, B, C)
During the procedure his systolic blood pressure dropped to 80 mm of Hg, which failed to improve despite aggressive fluid loading. Intra-aortic balloon pump was inserted with 1:1 frequency and maximum augmentation. He developed recurrent ventricular fibrillation followed by transient asystole requiring multiple defibrillation attempts, loading dose of antiarrhythmic medications and cardiopulmonary resuscitation. He was intubated and started on inotropic support with Adrenaline and Dopamine to maintain a mean arterial pressure of about 65-70 mmHg. Once his rhythm stabilized it was decided to do multivessel angioplasty of the right coronary artery followed by the circumflex and LAD as per the recommendation for intervention in patients with cardiogenic shock.
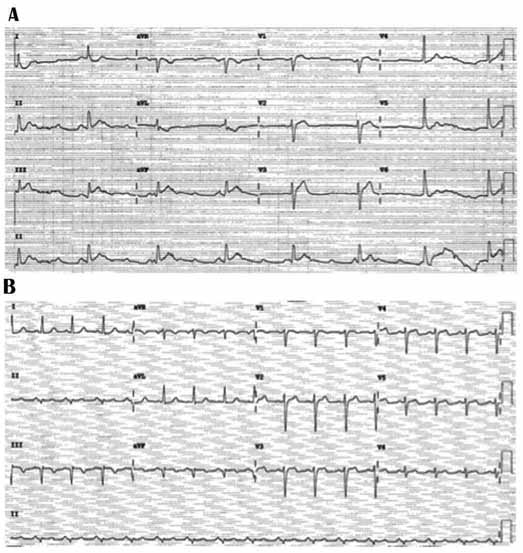
Figure 1: (A) ECG of Acute inferior wall and right ventricular myocardial infarction with complete heart block; (B) ECG of Evolved inferior wall myocardial infarction and normal sinus rhythm.
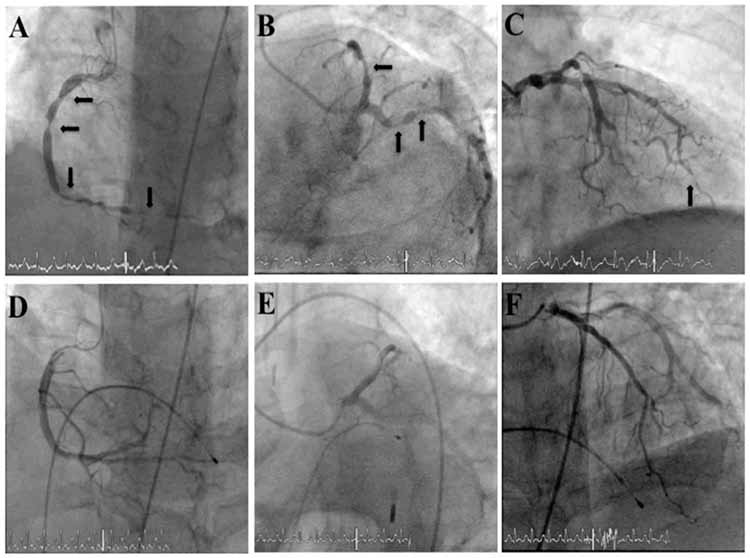
Figure 2: Panels A, B, C: Baseline angiogram showing spasm of LCA and RCA. Black block arrows in all panels represent sites of coronary spasm. Panels D, E, F: Final angiographic pictures after intracoronary administration of nitroglycerin in the corresponding arteries.
The right coronary artery was wired and an attempt was made to aspirate possible thrombus from the distal RCA using an Export catheter. No thrombus was retrieved and hence balloon dilatation of the PDA, PLB and distal RCA was carried out using a semi-compliant balloon 2 × 12 mm at 6-8 atm. During this time spontaneous improvement of moderate stenosis in the proximal RCA was noted suggesting dynamic obstruction. It was decided to administer intracoronary nitroglycerin despite a low blood pressure (80/50 mmHg) at near maximal dosages of both Adrenaline (1 mcg/kg/min) and Dopamine (18 mcg/kg/min). Following 100 mcg of intracoronary Nitroglycerin into the respective coronary arteries, there was abrupt relief of spasm in all three coronary arteries (Fig. 2: Panel D, E, and F).
The intra-aortic balloon pump was removed after 24 hours, weaned off inotropes and successfully extubated on the fifth post procedure day. On the fourth post-procedure day he was noted to have paucity of movement of his left hand and leg, along with an up going left plantar response. An urgent CT scan revealed right anterior cerebral artery territory ischemic infarct. The neurologist was consulted and it was decided to manage him conservatively with dual antiplatelet therapy and intravenous heparin. He was started on physiotherapy and his symptoms improved over the ensuing five days with grade 4 - power of the left upper and lower limb. He was started on high doses of Diltiazem along with long acting oral nitrates, aspirin, clopidogrel and statins. Serial ECG’s confirmed an evolved inferior wall myocardial infarction (Fig. 1B). The peak Troponin twelve hours following the procedure was 70.02 mcg/L (Reference for lab <0.04 mcg/L). Echocardiogram was consistent with inferior wall myocardial infarction as evidenced by mildly hypokinetic inferior wall with preserved systolic function. He was discharged after ambulation in the ward 10 days into his present admission with no recurrence of angina or arrhythmias.
Discussion
Spontaneous multivessel coronary artery spasm can present with a myriad of presentations varying from variant angina to complicated acute myocardial infarction.4,8 The difference in the prognosis of patients who present with coronary spasm with and without fixed stenosis has been previously described.9 Following the angiogram, the patient was re-interviewed to elicit any history cocaine abuse or use of herbal remedies but the patient denied and form of drug abuse. From review of literature of cases with similar presentation, it was apparent that three out of six cases had a history of bronchial asthma (Table 1).1-4,10 Airway hyper-responsiveness and coronary spasm share many pathophysiologic processes including inflammation, disturbances in the parasympathetic system, and elevated levels of circulating endothelin, thromboxane A2 and serotonin.11 The association between bronchial asthma and coronary spasm has been suggested but the exact mechanism has remained elusive, however it is clear that when coronary spasm occurs in patients with bronchial asthma they tend to follow a more malignant course.
Despite being on high doses of intravenous infusions of Adrenaline and Dopamine, coronary spasm in all three coronary vessels was relieved with 100 mcg of intracoronary nitroglycerin suggesting that local release of nitric oxide in the epicardial vessels can negate the effects of systemically administered vasoconstricting agents.
In view of past documentation of non-sustained ventricular tachycardia on Holter and recurrent ventricular fibrillation during the present episode he is advised close follow up for consideration of automatic implantable cardioverter defibrillator (AICD) despite the recent question on efficacy of AICD in patients with coronary spasm and frequent life threatening arrhythmias.12
Conclusion
Multivessel spasm should be considered even in patients with multiple coronary risk factors, irrespective of gender. Intra-coronary nitroglycerin should be administered after optimizing blood pressure even in hemodynamcially unstable patients with acute myocardial infarction to exclude coronary spasm and inadvertent percutaneous coronary intervention. Patients with bronchial asthma presenting with multivessel spasm may constitute a high-risk subset with a complicated in hospital course.
Acknowledgements
The author reported no conflict of interest and no funding was received for this work.
References
1. Saito H, Itoh T, Itoh M, Kanaya Y, Suzuki T, Hiramori K. Simultaneous multivessel coronary spasm causing acute myocardial infarction: a case report. Angiology 2007 Feb-Mar;58(1):112-117.
2. Lilli A, Vecchio S, Vittori G, Consoli L, Chechi T, Margheri M. Severe diffuse coronary artery spasm in the early phase of cardiogenic shock. Int J Cardiol 2009 May;134(3):e103-e104.
3. Richardson JD, Nelson AJ, Worthley SG, Teo KS, Baillie T, Worthley MI. Multivessel coronary artery spasm. Heart Lung Circ 2012 Feb;21(2):113-116.
4. Tacoy G, Kocaman SA, Balcioğlu S, Tanindi A, Ozdemir M, Cemri M, et al. Coronary vasospastic crisis leading to cardiogenic shock and recurrent ventricular fibrillation in a patient with long-standing asthma. J Cardiol 2008 Dec;52(3):300-304.
5. Beltrame JF, Sasayama S, Maseri A. Racial heterogeneity in coronary artery vasomotor reactivity: differences between Japanese and Caucasian patients. J Am Coll Cardiol 1999 May;33(6):1442-1452.
6. Pristipino C, Beltrame JF, Finocchiaro ML, Hattori R, Fujita M, Mongiardo R, et al. Major racial differences in coronary constrictor response between japanese and caucasians with recent myocardial infarction. Circulation 2000 Mar;101(10):1102-1108.
7. Prashanth P, Mukhaini M, Riyami AA, Sulaiman K, Shahrabani R, Riyami AM. Immediate and Six-month Clinical Outcome of Percutaneous Coronary Intervention in a Tertiary Hospital in the Sultanate of Oman. Oman Med J 2008 Oct;23(4):247-252.
8. Prinzmetal M, Kennamer R, Merliss R, Wada T, Bor N. Angina pectoris. I. A variant form of angina pectoris; preliminary report. Am J Med 1959 Sep;27:375-388.
9. Ong P, Athanasiadis A, Borgulya G, Voehringer M, Sechtem U. 3-year follow-up of patients with coronary artery spasm as cause of acute coronary syndrome: the CASPAR (coronary artery spasm in patients with acute coronary syndrome) study follow-up. J Am Coll Cardiol 2011 Jan;57(2):147-152.
10. Chuang YT, Ueng KC. Spontaneous and simultaneous multivessel coronary spasm causing multisite myocardial infarction, cardiogenic shock, atrioventricular block, and ventricular fibrillation. Circulation journal: official journal of the Japanese Circulation Society. 2009; 73:1961-4.
11. Haruta S, Okayama M, Uchida T, Hirosawa K, Kasanuki H. Airway hyperresponsiveness in patients with coronary spastic angina: relationship between coronary spasticity and airway responsiveness. Circulation journal: official journal of the Japanese Circulation Society. 2007; 71:234-41.
12. Letsas KP, Filippatos GS, Efremidis M, Sideris A, Kardaras F. Secondary prevention of sudden cardiac death in coronary artery spasm: is implantable cardioverter defibrillator always efficient? Int J Cardiol 2007 Apr;117(1):141-143.
|