|
Introduction
We present a case of a 49 year-old woman having no significant past medical history with severe chest pain since 4 hours, global ST elevation in all ECG leads and raised troponin T. A diagnosis of acute STEMI was made and the patient was subsequently thrombolysed with intravenous tenecteplase. Her echocardiogram revealed septal akinesia and left apical ballooning. The coronary angiogram did not reveal significant stenosis in any artery.
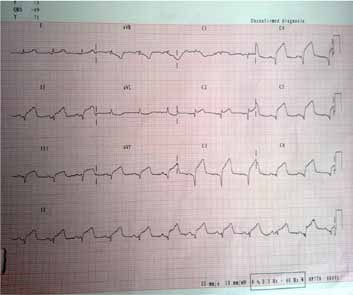
Figure 1: ECG with ST elevation in all the chest and limb leads.
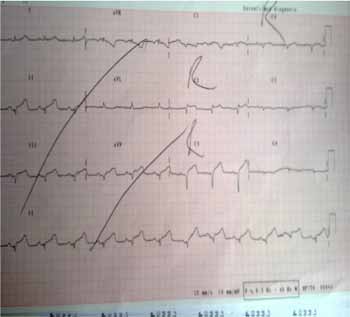
Figure 2: ST elevation on right side chest leads.
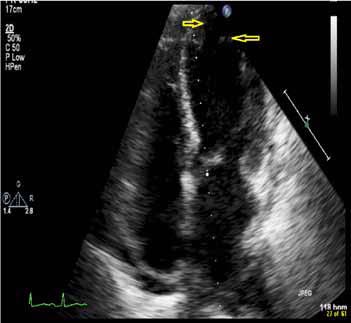
Figure 3: Echocardiogram showing left ventricle apical balloning.
Question
What is the diagnosis?
Answer
The patient was diagnosed with a condition called Takatsubo cardiomyopathy or stress cardiomyopathy.
Discussion
This phenomenon was first described in 1991 by Dote et al. who named the syndrome "takatsubo like cardiomyopathy" because the appearance of the left ventricle resembles a pot historically used in Japan to catch octopus (tako meaning octopus and tsubo means pot in Japanese).1 The cardiac dysfunction is transient and the left ventricle returns to normal within days to weeks. There are many theories to explain it; the most popular one is catecholamine excess due to the activation of sympathetic tone. Other causes could be multi-vessel coronary spasm or a transient atherosclerotic plaque.2
Patients typically present with acute chest pain, dyspnea, ST segment elevation in the precordial leads, and elevated levels of cardiac biomarkers.2 In 85% of cases, an emotional or physical stressor usually triggers the onset of clinical features e.g., emotional stressors include grief (death of a loved one), fear (armed robbery, public speaking), anger, relationship conflicts and financial problems. Depression is one of the most commonly encountered emotional distresses in both the general public and in various types of clinical populations.3 Physical stressors like acute asthma, surgery, chemotherapy and stroke may also lead to the condition. However, in 15% of cases, no cause can be identified.1
Takatsubo cardiomyopathy has important implications as its clinical presentation mimics that of an acute coronary syndrome.4 Even an experienced physician can find it hard to distinguish between the two. Diagnosis is generally established by an echocardiogram showing left apical ballooning resembling the Japanese octopus pot and a normal coronary angiogram.1 An echocardiogram must be obtained within days or weeks after the acute phase to confirm whether the abnormalities have reversed.2
The initial ICU management includes administration of aspirin, glycoprotein 2b/ 3a receptor inhibitors, nitrates, beta-blockers and diuretics. Once takatsubo cardiomyopathy is diagnosed, treatment is primarily supportive. Aspirin can be discontinued unless there is preexisting coronary artery disease. Beta-blockers may be continued long term to protect against catecholamine sensitivity.2 Long-term outlook in nearly all the patients after the acute phase is good. In approximately 5% of patients, recurrence may occur.1 Late complications include heart failure and pulmonary edema in 3% to 46% of patients and mortality rates are 1 to 3%. Recommendations for follow-up include echocardiography at 4 to 6 weeks post event to document normalization of function of the left ventricle.2
Prospective studies are needed to accurately determine its incidence and long-term outcomes. Studies are also required to elucidate the pathophysiology of this cardiomyopathy.4
References
1. Sharkey SW, Lesser JR, Maron BJ. Cardiology Patient Page. Takotsubo (stress) cardiomyopathy. Circulation 2011 Nov;124(18):e460-e462.
2. Derrick D. The "broken heart syndrome": understanding Takotsubo cardiomyopathy. Crit Care Nurse 2009 Feb;29(1):49-57, quiz 58.
3. Al-Busaidi Z, Bhargava K, Al-Ismaily A, Al-Lawati H, Al-Kindi R, Al-Shafaee M, et al. Prevalence of Depressive Symptoms among University Students in Oman. Oman Med J 2011 Jul;26(4):235-239.
4. Virani SS, Khan AN, Mendoza CE, Ferreira AC, de Marchena E. Takotsubo cardiomyopathy, or broken-heart syndrome. Tex Heart Inst J 2007;34(1):76-79.
|