|
Introduction
Scrotal dermatitis is characterized by severe itching, erythema, scaling and lichenification of the scrotal skin. Several factors are responsible for the condition, the most important being psychological stress and contact dermatitis either allergic or irritant. The condition has been easily overlooked as fungal infection of the scrotal area. Due to wide spread use of antiseptics and over the counter topical agents, this condition is very common nowadays. Though common, very limited literature has been published on scrotal dermatitis, as such either because of under reporting by the practitioners or because of the fact that it is not yet considered a separate entity by dermatologists. The condition has not yet received adequate clinical description. Though the condition can be treated easily, it causes significant physical and psychological morbidity to the patient in the form of persistent or recurrent symptoms and social embarrassment.
Etiopathogenesis
The penis and scrotum are physiologically in a dependent position and the skin covering them is extra-ordinarily elastic. As the underlying connective tissue is areolar, severe edema can develop rapidly. Allergic reactions of the male genitalia are most often acute. They are influenced by the dependent position, rich vascularity and looseness of the connective tissue in this area. The approximation of the cutaneous surfaces and the increased moisture are important factors in the production of contact dermatitis.
Scrotal dermatitis may be considered as an end result of various insults to the skin either patient induced or as a result of the pathological process. The symptoms vary depending on the etiological factors. The main pathology, like elsewhere is the persistent inflammation of the scrotal skin leading to the release of the various inflammatory mediators or proteolytic agents which leads to pruritus and this evokes continuous scratching of the scrotal skin leading to further aggravation of the inflammation and thus begins a vicious cycle which finally culminates in an erythematous or lichenified scrotum, which has been typically described as "wash leather scrotum". The pruritus in scrotal dermatitis often has a particular 'burning quality'. Since the inflamed skin has a higher permeability, the various over the counter products applied on the lesions further aggravate the condition. The etiopathogenesis of the scrotal dermatitis is schematically described in Fig. 1.
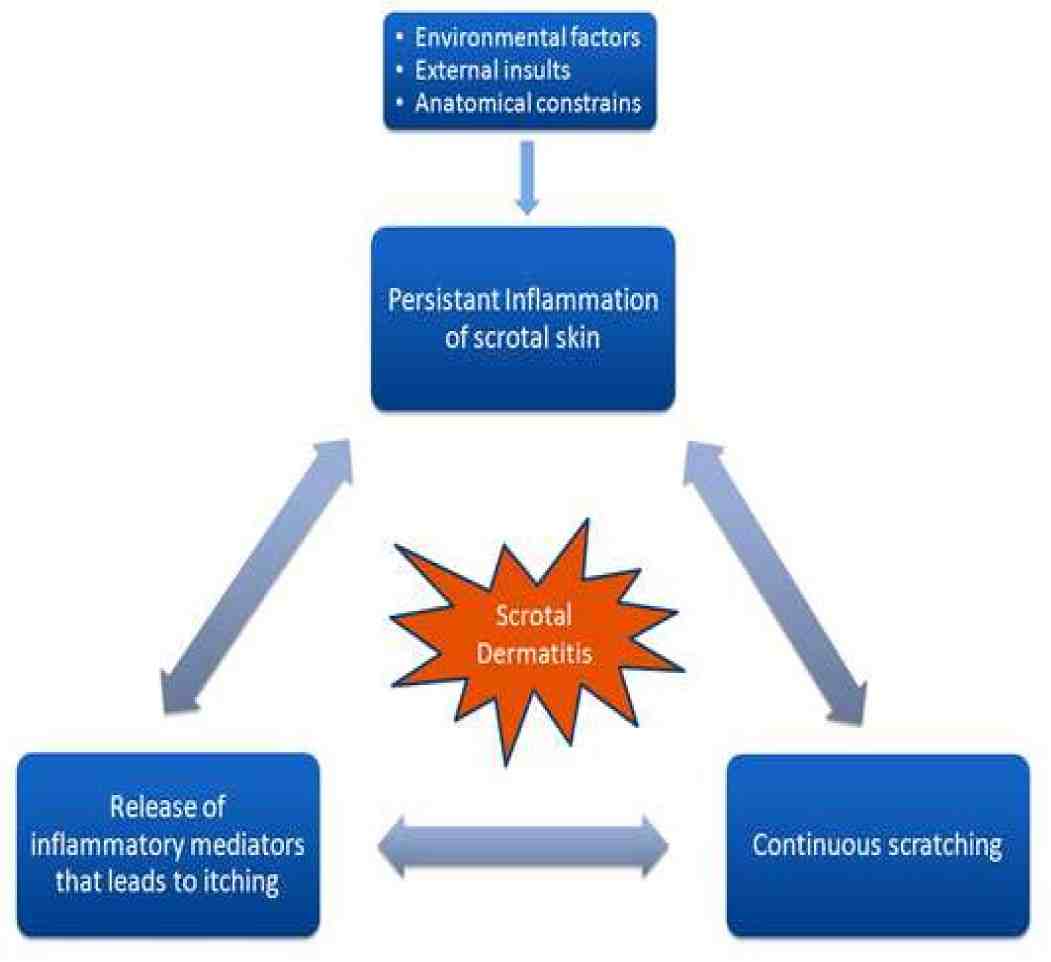
Figure 1: Schematic presentation of the etiopathogenesis of scrotal dermatitis.
Table 1: Important agents causing scrotal dermatitis.
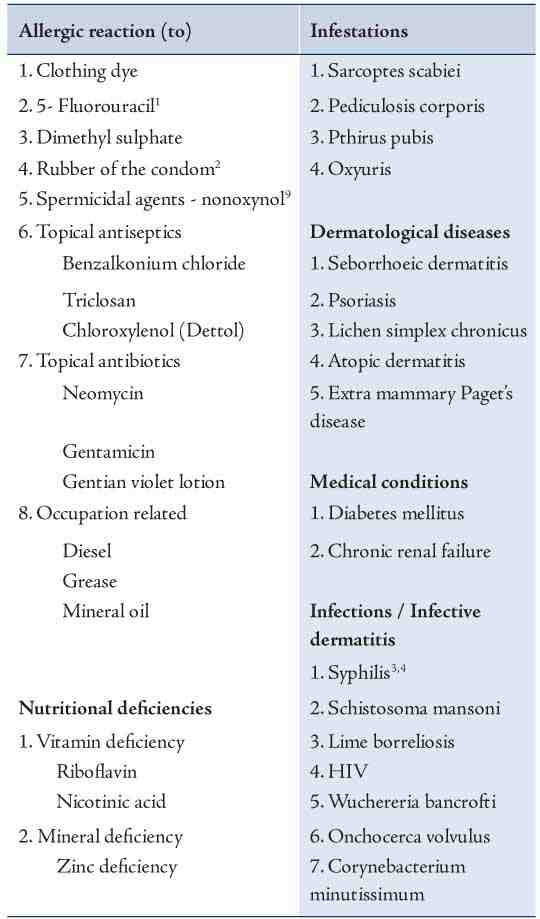
Scrotal dermatitis is usually multifactorial in origin. The various etiological agents evoking the condition are summarized in Table 1. Psychological stress is considered an important cause and it results in a sensation of itch on the scrotum.6 Itching then leads to psychological relief and further tendency to evoke the same response again. Finally, an itch scratch cycle develops resulting in the lichenification of the skin. Furthermore, self-medication with various agents leads to the development of dermatitis.
Occlusion of the area under hot and humid conditions is another predisposing factor and especially reported in soldiers who were posted in the tropics. Occupation related exposure to various agents is also a leading cause of scrotal dermatitis. Various precipitating factors like increased temperature, sweating and occlusive clothing of industrial workers facilitate the percutaneous absorption of irritant agents and leads towards an increased chance of allergic and irritant dermatitis. The important agents include various mineral oils used as cooling agents, diesel, coal tar and grease.7,8 There is also an increased chance of malignancy in longstanding cases of this dermatitis.
The scrotum is an area with remarkable permeability.9 It provides a unique percutaneous doorway for the entrance of drugs into the circulation and is thus uniquely susceptible to toxic and irritant agents. Hence, a few topical agents readily produce irritant dermatitis and even ulceration when applied onto the scrotal skin. Dermatitis medicamentosa thus appears to be another important etiological factor for this condition.
Contact dermatitis to various topical agents like over the counter anti-fungal medications can lead to scrotal dermatitis. It is very difficult to differentiate clinically whether the skin changes are that of the allergic or irritant dermatitis or a manifestation of the scrotal dermatitis because in both conditions, there are apparent inflammatory changes over the skin. A patch test can be performed to determine the nature of the allergens.
Dermatitis in response to the spermicidal agents used in contraceptive creams like nonoxynol 9 and also to the rubber in condoms have also been reported.3,10 Chloroxylenol or 4-chloro-3,5-dimethylphenol present in various commonly used antiseptic preparations and soaps is also an important cause of dermatitis of the scrotum.11 It also causes the removal of normal microbial flora of the skin and facilitates colonization by pathogenic groups. It has been reported that chloroxylenol is the second most common antibacterial agent causing dermatitis on human skin. The common misconception brought about by the advertising agencies for various antibacterial agents have lead to the wide spread use of this agent and increased incidence of various dermatitis including scrotal dermatitis.
Benzalkonium chloride and triclosan used in bath emollients have also been reported to cause scrotal dermatitis and gangrene simulating Fournier’s gangrene.12 Gentian violet solution or pyoctanin is widely used in dermatological practice and can also lead to allergic contact dermatitis, as well as necrosis of the intertriginous areas and scrotum.13
Oro-oculo-genital syndrome due to riboflavin and/or zinc deficiency is also characterized by significant scrotal changes. The term deficiency scrotal dermatitis has been used to indicate this condition.14 It can also be due to nicotinic acid deficiency. It is characterized by angular stomatitis, chelitis and glossitis in addition to scrotal involvement. Eye involvement in the form of retrobulbar neuritis and photophobia are also present.
Attempts to isolate micro-organisms from this condition mainly yielded candida and Staphylococcus species as the most common agents.15 These are superinfections of the involved scrotal skin and generally not primary etiological agents. Infective conditions involving the scrotal skin can also lead to infective dermatitis of the scrotum. Human immunodeficiency virus (HIV) infected patients also present with severe dermatitis and ulcerations of the scrotum.16 The exact etiological agents have not been isolated but various factors like immunosuppression and abnormal skin physiology have been postulated as possible reasons. Gummatous syphilis of scrotum can also present with thickened scrotal skin and can cause scrotal dermatitis. Erythrasma presenting as scrotal dermatitis have also been reported.
Fungal infection of the genital region is an important differential diagnosis for this condition. Fungal infections in general are easily identifiable by the clear cut margins of papular lesions and the presence of peripheral scales and central clearing. But most of the times, the diagnostic challenge arises when the patient treats the area with a topical steroid preparation, in such cases a skin scrapping using a blunt scalpel from the edge of the lesions results in a positive KOH mount (using 10% potassium hydroxide) of the fungus.
Lichen simplex chronicus of the scrotal skin is also frequently encountered in clinical practice.17 The scrotal skin shows thickening, hypo or hyperpigmentation, sparse hair, and clearly defined margin. Patients will give a history of chronicity and will be psychologically stressed. There may also be associated lichen simplex lesions elsewhere like the nape of the neck.
Extramammary Paget's disease (EMPD) is a rare skin disease and amongst which the EMPD of the scrotum is the commonest. It can also mimic scrotal dermatitis.18 Scrotal exfoliative dermatitis with ulcers have also been reported with the therapy of acute promyelocytic leukemia with all-trans retinoic acid.19,20 Idiopathic thrombocytopenia can sometimes present with purpuric spots on the scrotum which may mimic dermatitis, but associated purpuric spots can be found elsewhere in the lower limb and body.21
Distinctive exudative discoid and lichenoid chronic dermatosis described by Sulzberger and Garbe (oid-oid disease) is considered as a severe form of nummular eczema. Scaling plaques may persist in the genital region, even after satisfactory remission elsewhere in the body.
Classification
An endeavor to classify scrotal dermatitis based on the various types of clinical features have earlier been attempted by a few authors, though this classification is old and was used for the dermatitis resulting from vitamin and mineral deficiency, it also seems to hold well for scrotal dermatitis arising from other conditions. In routine clinical practice, there are various manifestations of scrotal dermatitis that were generally encountered.14 Scrotal dermatitis can be classified into the following four categories:
Type 1 ~ Mild acute dry type: This is characterized by erythematous scrotal skin with a clear cut demarcation between the normal and the involved skin. This is less conspicuous in colored skin and may become apparent on stretching the skin. It is characterized by severe itching and burning sensation in the involved area. This stage may persist for a few days or weeks and may resolve by itself with mild desquamation if no further insult occurs.
Type 2 ~ Severe chronic dry: In this stage, the involved scrotum looks bright red or hypopigmented and scaly. There may also be involvement of the adjacent thighs and under surface of the penis. Itching and burning sensation is marked. (Fig. 2)
Type 3 ~ Chronic wet: The whole of the scrotum and the inner side of the thighs become macerated and oozing is present. Sometimes telangiectasia may also be seen. There also tends to be fetid odour and painful lesions. (Fig. 3)

Figure 2: Type 2 scrotal dermatitis.

Figure 3: Type 3 scrotal dermatitis.
Type 4 ~ Ulcerated and edematous: The scrotal skin is swollen, with fluid and pus oozing from the fetid area, presenting with extreme pain from ulceration. In worst cases, spreading of gangrene from the scrotum to the legs and lower abdominal wall occurs.
Management
The main stay of management is to remove the precipitating factors. Loose clothing should is advised to remove the occlusive elements. Any over the counter agent used should be immediately stopped and an absorbing powder can be given for routine use. Psychiatric counseling should also be offered to relieve stress and if needed psychotropic drugs like tricyclic antidepressants can be administered.
For mild and acute dry type, a mild potency steroid prescribed once daily for a week in addition to removal of the precipitating factor is usually enough. Oral antihistamines may also be given. In cases of older patients, a sedative antihistaminic is preferred to the non-sedating forms so as to prevent the patient from continuously scratching the affected area. Like atopic dermatitis patients, the most important aspect in terms of therapy is to break the itch-scratch cycle.
Severe chronic dry type should be treated with mild potency steroids and oral antihistamines. An emollient can be supplemented during the day time. In addition, narrow band UV-B radiation has been found to be useful in treating the dermatitis of scrotal skin. Though genital areas are covered during regular treatment with narrow band UVB for other dermatological conditions, it has been found that dermatitis of the scrotal skin improves with narrow band therapy. At the author’s institution, narrow band is administered at 300 nm for a period of three to five consecutive days. The results of this therapy have been found to be astonishing both in decreasing the severity and better patient satisfaction. Narrow band has routinely been used for dermatological conditions for nearly a decade, and so far there has been no report of increased incidence of malignancy of the genital skin; however, this notion should be kept in mind and there should be more follow-up of cases.22 Narrow band phototherapy exerts its action through various mechanisms, like reduction of Langerhans cells, induction of immunomodulatory cytokines, and promoting apoptosis of infiltrating T-lymphocytes.23
The authors would like to recommend initiating therapy in recalcitrant cases using narrow band and then follow-up with mild potency topical corticosteroids and antihistamines. For chronic wet and ulcerated stages, frequent wet compresses with potassium permanganate 1 in 1000 to 10000 dilution can be used. Antibiotics can be given for infected lesions, and surgical opinion should be obtained in cases of severe involvement resulting in pus discharge and gangrene. In cases of longstanding and persistent forms of the condition, an attempt should be made to rule out EMPD. Finally, oral supplements should be given for cases occurring as a result of nutritional deficiency.
Conclusion
To summarize, scrotal dermatitis has long been overlooked as a separate disease entity, thus recognition as a separate condition, as well as further investigation into the etiopathogenesis is necessary for better formulation of treatment protocols.
Acknowledgements
The author reported no conflict of interest and no funding was received for this work.
References
1. Shelley WB, Shelley ED. Scrotal dermatitis caused by 5-fluorouracil (Efudex). J Am Acad Dermatol 1988 Nov;19(5 Pt 2):929-931.
2. Fisher AA. Condom dermatitis in either partner. Cutis 1987 Apr;39(4):281, 284-285.
3. Fisher AA. Dermatitis from rubber, adhesives and gums. Chapter 10. In: Fisher AA, editor. Contact Dermatitis, 2nd ed. Philadelphia: Lea and Febiger; 1973, p. 448.
4. Jeong E, Oh ST, Lee JY, Cho BK. Secondary syphilis presenting as scrotal eczema. J Am Acad Dermatol 2007 Dec;57(6):1099-1101.
5. Kang SH, Lee D, Park JH, Kang MS, Cho SH, Park SW. Scrotal eczema-like lesion of secondary syphilis in an HIV-positive patient. Acta Derm Venereol 2005;85(6):536-537.
6. Bhatia MS, Gautam RK, Bedi GK. Psychiatric profile of patients with neurodermatitis. J Indian Med Assoc 1996 Dec;94(12):445-446, 454.
7. Karube H, Aizawa Y, Nakamura K, Maeda A, Hashimoto K, Takata T. [Oil mist exposure in industrial health–a review]. Sangyo Eiseigaku Zasshi 1995 Mar;37(2):113-122.
8. Cusano F, Capozzi M, Errico G. Allergic contact dermatitis from coal tar. Contact Dermatitis 1992 Jul;27(1):51-52.
9. Fisher AA. Unique reactions of scrotal skin to topical agents. Cutis 1989 Dec;44(6):445-447.
10. Banerjee R, Banerjee K, Datta A. Condom leukoderma. Indian J Dermatol Venereol Leprol 2006 Nov-Dec;72(6):452-453.
11. Calnan CD. Contact dermatitis from drugs. Proc R Soc Med 1962 Jan;55:39-42.
12. Saw NK, Hindmarsh JR. Acute irritant reaction to an antiseptic bath emollient. Postgrad Med J 2005 Feb;81(952):131-132.
13. Schoppelrey HP, Mily H, Agathos M, Breit R. Allergic contact dermatitis from pyoctanin. Contact Dermatitis 1997 Apr;36(4):221-224.
14. Frankland AW. Deficiency scrotal dermatis in P.O.Ws in the Far East. Br Med J 1948 May;1(4560):1023-1026.
15. Woskoff A, Carabelli S, Hoffman M. [Dermatitis of the scrotum]. Med Cutan Ibero Lat Am 1982;10(1):37-40.
16. Hillman RJ, Goldmeier D, Taylor-Robinson D. Scrotal ulceration in HIV-positive patients. Genitourin Med 1990 Apr;66(2):93-94.
17. Rajashekhar N, Thippeswamy C, Babu PN. Lichen simplex chronicus of scrotum. Indian J Dermatol Venereol Leprol 1999 Mar-Apr;65(2):91-92.
18. Png JC, Tung KH, Wong YE, Mokal N, Rajagopalan R, Chong PY. Extramammary Paget’s disease: a report of three cases and review of the literature. Ann Acad Med Singapore 1995 Jul;24(4):636-639.
19. Tajima K, Sagae M, Yahagi A, Akiba J, Suzuki K, Hayashi T, et al. [Scrotum exfoliative dermatitis with ulcers associated with treatment of acute promyelocytic leukemia with all-trans retinoic acid]. Rinsho Ketsueki 1998 Jan;39(1):48-52.
20. Al Huneini M, Wasim F, Al Farsi K, Al-Khabori M, Al Kindi S. Genital ulcer development in patients with acute promyelocytic leukaemia treated with all-trans retinoic Acid: a case series. Oman Med J 2013 May;28(3):207-209.
21. Madhusudhanan M, Yusuff AM. Unusual presentation of chronic idiopathic thrombocytopenic purpura. Oman Med J 2008 Jan;23(1):48-49.
22. Weischer M, Blum A, Eberhard F, Röcken M, Berneburg M. No evidence for increased skin cancer risk in psoriasis patients treated with broadband or narrowband UVB phototherapy: a first retrospective study. Acta Derm Venereol 2004;84(5):370-374.
23. Majoie IM, Oldhoff JM, van Weelden H, Laaper-Ertmann M, Bousema MT, Sigurdsson V, et al. Narrowband ultraviolet B and medium-dose ultraviolet A1 are equally effective in the treatment of moderate to severe atopic dermatitis. J Am Acad Dermatol 2009 Jan;60(1):77-84.
|