|
Abstract
Various causes of common peroneal palsy have been described in the English language medical literature in the past. Authors report a case of foot drop in a post cesarean section patient, due to osteochondroma of the proximal fibula, which recovered completely after excision of the offending mass.
Keywords: Osteochondroma; Fibular head; Common peroneal nerve; Entrapment neuropathy; Cesarean section.
Introduction
Incidence of neurological complications in peri and post partum period has been reported to be around 1%.1 Compressive neuropathy of the common peroneal nerve (CPN) has been described to be due to cysts from the tibiofibular joint,2 lateral meniscal cysts,3 fibular head osteophytes,4 and osteochondroma of the fibular head.4-7 Traumatic causes have been reported due to fractures of the proximal fibula, traction of the nerve, compression by tight bandages or direct injury to the nerve.8 Osteochondroma of the fibular head as a cause of CPN palsy presenting soon after normal or cesarean delivery is very rare.
Case Report
A 21-year-old primigravida was taken up for emergency cesarean section, due to non-progression of labor. Lower segment cesarean section (LSCS) was done under spinal anesthesia with a 25G needle in the L3-4 space and 3 mL of 0.5% bupivacaine with patient in the right lateral position. After the spinal anesthesia, a wedge was kept under the buttocks of the patient to avoid post spinal hypotension. Cesarean section was completed in 43 minutes. In the immediate postoperative period, she noticed inability to dorsiflex the right ankle, (Fig. 1). There was no sensory loss in the extremity. She had grade 2/5 power of the ankle dorsiflexors and evertors. Pain in the right leg from the level of the fibular head to the foot started after a few days with burning sensation in the leg. She was aware of painless masses around the right knee especially over the medial side but was not aware of the small masses over the proximal fibula. Her burning pain subsided in a few days’ time.

Figure 1: Figure showing absent dorsiflexion of the right foot.
Physical examination revealed presence of multiple bony hard, nontender masses on the side of the proximal tibia and lateral aspect of the fibula, and over the lateral aspect of the distal femur. Plain radiographs showed multiple osteochondromas around the proximal tibia and fibula and the distal femur. (Fig. 2)

Figure 2: Plain films showing multiple osteochondroma over the medial aspect of the proximal tibia, over the medial and posterior aspect of the proximal fibula. A small osteophyte is seen over the proximal fibula (white arrow).
A computerized tomography (CT) scan further confirmed the multiple osteochondromas, and in addition showed a small mass from the lateral aspect of the fibular neck. (Fig. 3)

Figure 3: CT scan showing the osteophyte over the fibula neck (white arrow).
A magnetic resonance imaging (MRI) was done to identify the relation of the CPN to the fibular neck masses. MRI showed multiple osteochondromas around the lateral aspect of the distal femur; medial and lateral aspect of the proximal tibia; and medial, lateral, and posterolateral aspect of the proximal fibula. Two small osteochondromas of 3 and 4 mm were noted in the lateral aspect of the proximal fibula. The masses were found indenting the common peroneal nerve at the site where it winds round the proximal fibula. (Fig. 4)
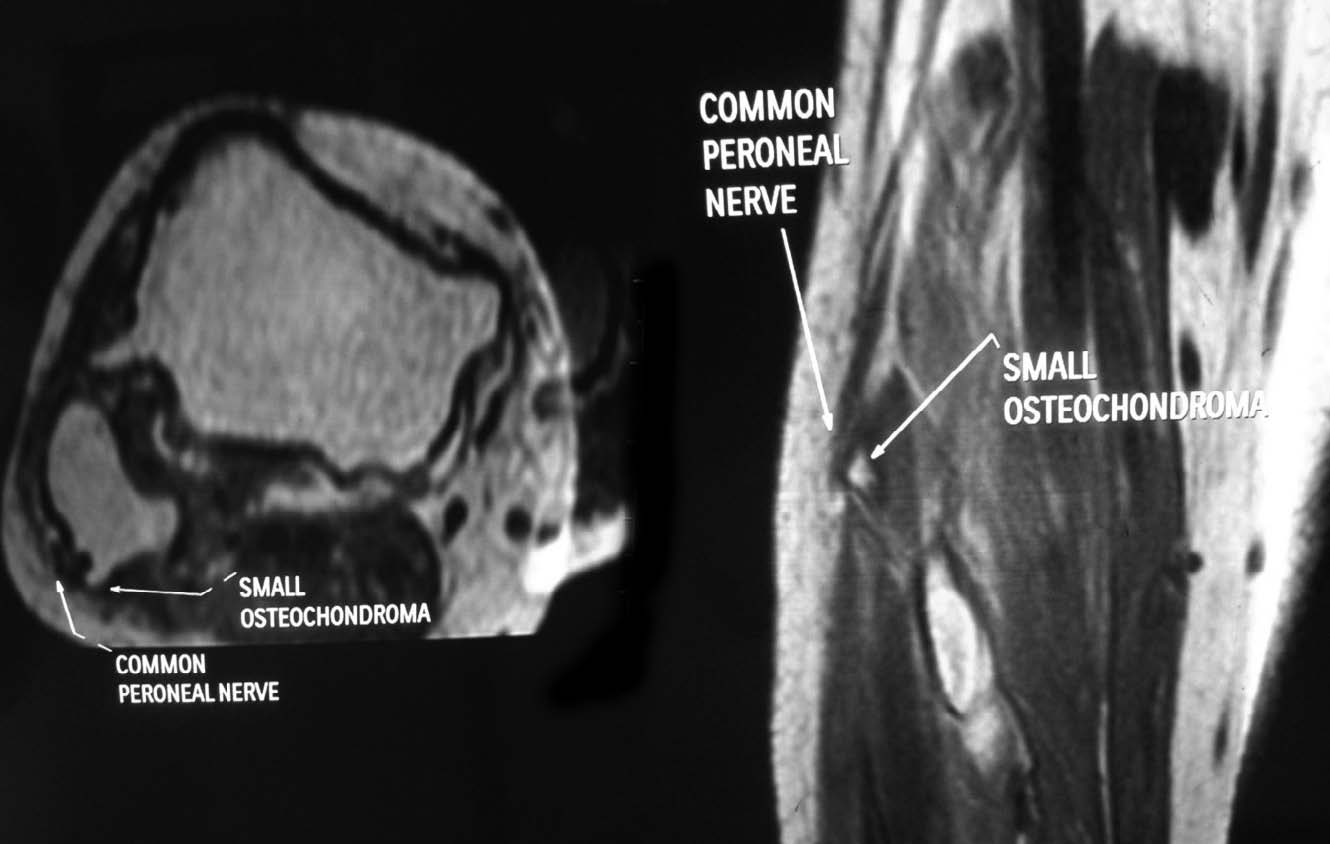
Figure 4: MRI showing the compression of the CPN by the osteochondroma.
Electrophysiological studies revealed a nonstimulatible right common peroneal nerve. Electrophysiological studies of the posterior tibial nerve were normal. The patient underwent surgical decompression of the right CPN and excision of the offending osteochondroma. The osteochondroma was found displacing the CPN, (Fig. 5). A neurolysis of the CPN was also done. Recovery from paralysis started in 4 weeks’ time. She recovered completely with grade 5/5 power of the dorsiflexors and evertors of the ankle at 6-month follow-up.
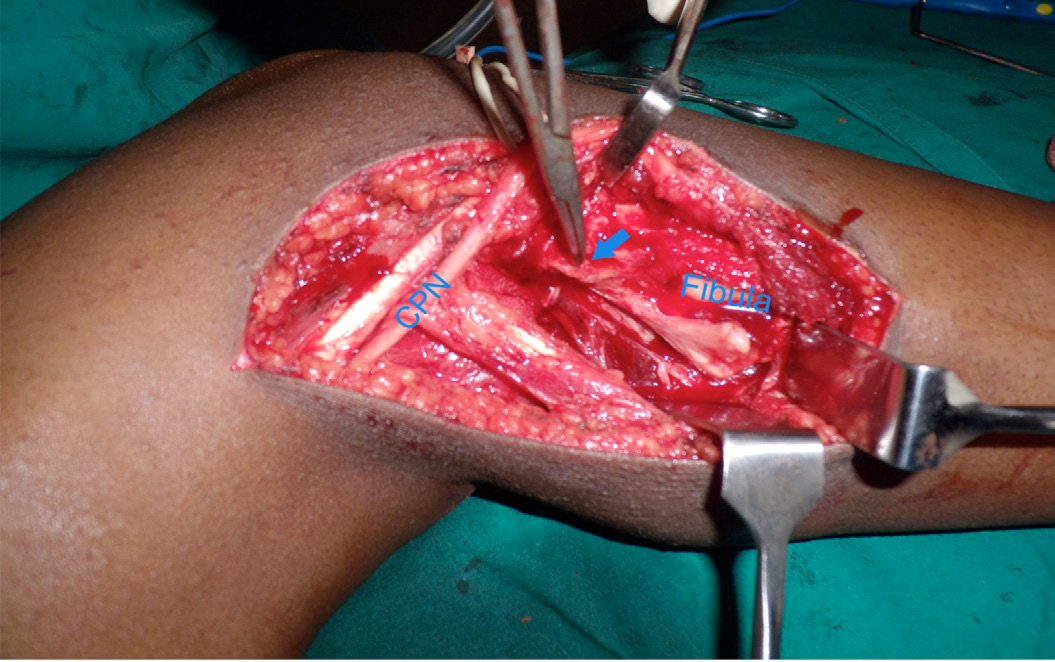
Figure 5: Operative picture showing the common peroneal nerve and the osteochondroma. Histopathology confirmed the diagnosis of osteochondroma.
Discussion
The peroneal nerve is vulnerable to injury while it winds around the neck of the fibula. At this particular location, the nerve is superficial and covered only by subcutaneous tissue and fat. Various causes of CPN palsy had been reported in literature before. Extraneural compression by cysts of the lateral meniscus,3 synovial cysts from the proximal tibiofibular joint,2 ganglion cysts,7 osteophytosis,4 and benign bone tumors around the proximal fibula causing CPN palsy had been reported before.4-7 Osteochondromas are benign tumors of the bone located mainly in the metaphysic of long bones with more than 35% of cases affecting the bones around the knee.
Our case was diagnosed to be multiple exostosis syndrome, which is characterized by formation of multiple bone masses which developed from the epiphysis. Osteochondroma are usually asymptomatic but may become painful with fracture of the bony stalk, nerve impingement syndromes, malignant transformation, and mass effects. Clinical manifestations depend on the size and location of the mass. Prolonged compression can occur with hip abduction, leg external rotation and knee flexion, as done in gynecological procedures,8 resulting in CPN palsy. External rotation of the limb with knee flexion as it happens in prolonged bed rest may result in compression of the peroneal nerve at the proximal fibula due to bony prominence of the fibular head. This, in addition to the presence of osteochondroma, triggered the common peroneal nerve palsy in our patient. Moreover, by keeping the patient on the right lateral position for the spinal anesthesia, the knee was kept in slight varus further stretching the CPN.
Our patient received spinal anesthesia for cesarean section and initially it was thought that this could be the reason for her neurological deficit; however, plain films and advanced imaging techniques identified osteochondroma of the proximal fibula as the cause of her foot drop. Foot drop during spinal anesthesia has been reported before which is thought to be due to needle trauma or inadvertent drug placement.1,9 Postpartum neurologic deficit is usually bilateral and could be due to spinal cord ischemia, direct trauma to the spinal nerve or the spinal cord, chemical toxicity of the local anesthetic agent or formation of a hematoma.10 Epidural catheter placement may cause direct neural trauma.11 Peters and Hinds reported a case of postpartum foot drop in a postpartum patient caused by segmental demyelination as a result of fetal head compression on the lumbosacral plexus. Their patient was subsequently diagnosed to have hereditary sensory neuropathy.1
Conclusion
Postpartum foot drop is a rare complication, in this case, due to the presence of an osteochondroma over the fibular head. This complication should have been anticipated and a lateral position on the affected side should have been avoided.
Acknowledgements
Authors declare that they have no conflict of interest
References
1. Peters G, Hinds NP. Inherited neuropathy can cause postpartum foot drop. Anesth Analg 2005 Feb;100(2):547-548.
2. Hersekli MA, Akpinar S, Demirors H, Ozkoc G, Ozalay M, Cesur N, et al. Synovial cysts of proximal tibiofibular joint causing peroneal nerve palsy: report of three cases and review of the literature. Arch Orthop Trauma Surg 2004 Dec;124(10):711-714.
3. Jowett AJ, Johnston JF, Gaillard F, Anderson SE. Lateral meniscal cyst causing common peroneal palsy. Skeletal Radiol 2008 Apr;37(4):351-355.
4. Flores LP, Koerbel A, Tatagiba M. Peroneal nerve compression resulting from fibular head osteophyte-like lesions. Surg Neurol 2005 Sep;64(3):249-252, discussion 252.
5. Gallagher-Oxner K, Bagley L, Dalinka MK, Kneeland JB. Case report 822: Osteochondroma causing peroneal palsy-imaging evaluation. Skeletal Radiol 1994 Jan;23(1):71-72.
6. Yoo JH, Min KD, Kim CK, Cha JG. A case of extension loss of great toe due to peroneal nerve compression by an osteochondroma of the proximal fibula. Arch Orthop Trauma Surg 2010 Sep;130(9):1071-1075.
7. Mnif H, Koubaa M, Zrig M, Zammel N, Abid A. Peroneal nerve palsy resulting from fibular head osteochondroma. Orthopedics 2009 Jul;32(7):528.
8. Baima J, Krivickas L. Evaluation and treatment of peroneal neuropathy. Curr Rev Musculoskelet Med 2008 Jun;1(2):147-153.
9. Nirmala BC, Kumari G. Foot drop after spinal anaesthesia: A rare complication. Indian J Anaesth 2011 Jan;55(1):78-79.
10. Pham LH, Bulich LA, Datta S. Bilateral postpartum femoral neuropathy. Anesth Analg 1995 May;80(5):1036-1037.
11. Omeroglu H, Ozçelik A, Turgut A. Bilateral peroneal nerve palsy after simultaneous bilateral total knee arthroplasty. Report of a case with rheumatoid arthritis. Knee Surg Sports Traumatol Arthrosc 2001 Jul;9(4):225-227.
|