Teratomas are neoplasms that arise from pluripotent cells and may have well-differentiated layers of ectoderm, endoderm, and mesoderm.1,2 The gonads are the most common sites of origin followed by the sacrococcygeal region.3 The kidney represents an exceedingly rare site for extragonadal teratomas.4 Our literature search revealed only four reported cases of primary immature renal teratoma, and none in a neonate, which makes the present case the fifth. This is also the first reported case of primary immature renal teratoma in a neonate.
Case Report
A two-week-old male neonate (born at term weighing 3.4 kg and good Apgar score) was brought to the hospital with poor oral intake, lethargy, and vomiting. He was found to have severe dehydration, hypotension, and a large abdominal mass. Blood report revealed pH of 6.8, HCO3 of 34 meq/L, and lactate level of 20 mmol/kg, indicating metabolic acidosis. The infant was resuscitated and intubated. Initial echocardiogram showed severe left ventricular dysfunction with an ejection fraction of 20% and severe mitral regurgitation. He was admitted for evaluation as a case of cardiogenic shock and abdominal mass.
The patient was given epinephrine and milrinone for two days. The high blood pressure which developed was regulated by hydralazine and amlodipine. A repeat echocardiogram showed normal cardiac function with no mitral regurgitation.
A computerd tomography (CT) scan of the abdomen revealed a 7.0 × 8.1 × 7.6 cm mass occupying most of the left abdomen. It displaced the surrounding organs and the main abdominal vasculature. Multiple enhancing blood vessels traversed the mass. The left kidney could not be seen separately. There was no sign of calcification or hemorrhage within the mass. The left renal artery was faintly visible as originating from the aorta and supplying the mass [Figure 1]. These findings were supported by magnetic resonance imaging which showed a solid mass on the left side of the abdomen with necrotic and cystic components. The mass appeared to arise from the left kidney, causing its superolateral displacement.
A provisional diagnosis of Wilms’ tumor was made. The patient underwent laparotomy where the left kidney along with the tumor was excised. The excised tumor was large (4.5 × 6 × 8 cm) with a solid cystic, soft, and friable gray-white cut surface, almost replacing the normal right kidney [Figure 2].
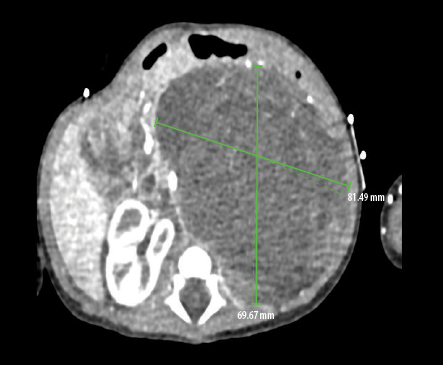 Figure 1: CT scan showing a large left abdominal mass. The right kidney appears normal.
Figure 1: CT scan showing a large left abdominal mass. The right kidney appears normal.
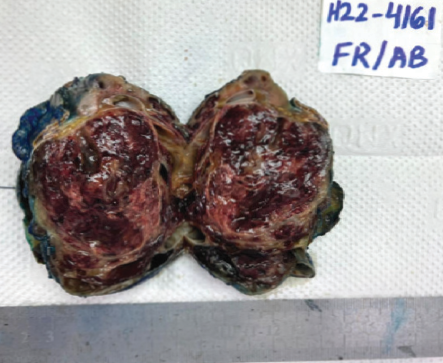 Figure 2: Gross specimen showing a solid, cystic, well-demarcated tumor compressing the normal renal parenchyma.
Figure 2: Gross specimen showing a solid, cystic, well-demarcated tumor compressing the normal renal parenchyma.
The specimen was sent for histopathology. Microscopically, a cyst lined by keratinizing stratified squamous epithelium with skin adnexal structures was seen, along with mucinous columnar epithelium, and retinal tissue [Figure 3]. Solid focus showed areas of brain tissue, cartilage, and bone [Figures 4 a and b]. Foci of immature neuroectodermal tissue with areas of rosette formation was also present [Figure 4c]. Based on these features, a diagnosis of intrarenal immature teratoma was made.
 Figure 3: (a) Teratomatous component of keratinizing stratified squamous epithelium with skin adnexa, magnification = 40 ×. (b) Teratomatous component of the mucinous columnar epithelium, magnification = 40 ×. (c) Teratomatous component of retinal tissue, magnification = 4 ×. Hematoxylin and eosin stain was used on all three slides.
Figure 3: (a) Teratomatous component of keratinizing stratified squamous epithelium with skin adnexa, magnification = 40 ×. (b) Teratomatous component of the mucinous columnar epithelium, magnification = 40 ×. (c) Teratomatous component of retinal tissue, magnification = 4 ×. Hematoxylin and eosin stain was used on all three slides.
 Figure 4: (a) Teratomatous component of bone, cartilage, and cysts, magnification = 4 ×. (b) Teratomatous component of bone tissue, magnification = 40 ×. (c) Immature neuroectodermal tissue, magnification = 40 ×. Hematoxylin and eosin stain was used on all three slides.
Figure 4: (a) Teratomatous component of bone, cartilage, and cysts, magnification = 4 ×. (b) Teratomatous component of bone tissue, magnification = 40 ×. (c) Immature neuroectodermal tissue, magnification = 40 ×. Hematoxylin and eosin stain was used on all three slides.
Postoperatively, the patient recovered well, and his blood pressure remained normal. He was discharged on the tenth postoperative day. When seen in the clinic after two weeks, his blood pressure was within normal range, and the echocardiogram showed normal function and structure of the heart.
Discussion
We have presented a rare case of primary immature renal teratoma in a two-week-old male neonate and its management. The kidney represents an exceedingly rare site for an extragonadal teratoma.4 In the literature, only four cases of immature renal teratoma have been reported—three children and one adult.3 To our knowledge, no neonate case has been reported, which should make the current case the first one reported in a neonate.
Intrarenal teratomas are often large but usually discovered incidentally.5,6 Patients with renal teratoma can present with abdominal swelling, abdominal pain, and hematuria.6 In the current case, the presentation was of cardiogenic shock and abdominal mass.
The differential diagnosis includes teratoid Wilms’ tumor, lymphoma, neuroblastoma, hydronephrosis, and infected renal cysts. For the tumor to be labeled as primary intrarenal teratoma, it should fulfill the Beckwith criteria which stipulate that the primary tumor should be unequivocal of renal origin and should exhibit heterotopic organogenesis.7 It is important to differentiate renal teratoma from teratoid Wilms’ tumor. The latter consists predominantly of heterogeneous tissue of extraordinary diversity, which may include the presence of cartilage, bone, muscle, neuroglial tissue, fat, and mature squamous epithelium.6 The presence of hair shafts is taken as evidence of terminal differentiation which is described in renal teratoma but not in Wilms’ tumor.8 In the present case, the tumor was unequivocal of intrarenal origin and mainly contained squamous epithelium with adnexal structures forming skin and immature components. As the characteristics were consistent with the criteria given by Beckwith, it was diagnosed as a renal immature teratoma.
The currently recommended therapy for pediatric immature teratoma is surgical excision alone.9 However, there is no unified standard treatment—two cases of immature renal teratoma in the literature were treated with surgical excision alone, and the other two with surgical excision
and chemotherapy.3
Conclusion
Though immature renal teratomas are extremely rare and preoperative diagnosis is difficult, it must be considered in the differential diagnosis of any renal mass in children and adults and should be distinguished from other entities to ensure the correct choice of treatment.
Disclosure
The authors declared no conflicts of interest. Informed consent was obtained from the patient.
references
- 1. Shumiye YG, Bushra FY, Sirak EH, Wondimagegnehu MB. Renal immature teratoma: a rare entity; a case report and literature review. Urol Case Rep 2021 Jan;34:101495.
- 2. Nirmal TJ, Krishnamoorthy S, Korula A. Primary intrarenal teratoma in an adult: a case report and review of literature. Indian J Urol 2009 Jul;25(3):404-406.
- 3. Zhang XL, Xu G, Li JL, Pan SH, Yan JJ. Renal immature teratoma in a male adult. A case report and literature review. Medicine 2018;97(35):e12143.
- 4. Adhikari RC, Sayami G. Immature teratoma of kidney in a 5-month-old child. Journal of Pathology of Nepal 2013;3(5):425-427.
- 5. Jacob S, Ghosh D, Rawat P, Bhatti W, Singh VP. Primary intra-renal teratoma associated with renal dysplasia: an unusual entity. Indian J Surg 2013 Jun;75(S1)(Suppl 1):77-79.
- 6. Dehner LP. Intrarenal teratoma occurring in infancy: report of a case with discussion of extragonadal germ cell tumors in infancy. J Pediatr Surg 1973 Jun;8(3):369-378.
- 7. Beckwith JB. Wilms’ tumor and other renal tumors of childhood: a selective review from the National Wilms’ tumor study pathology center. Hum Pathol 1983 Jun;14(6):481-492.
- 8. Govender D, Nteene LM, Chetty R, Hadley GP. Mature renal teratoma and a synchronous malignant neuroepithelial tumour of the ipsilateral adrenal gland. J Clin Pathol 2001 Mar;54(3):253-254.
- 9. Hamidi H, Foladi N. Intrarenal teratoma within a horseshoe kidney-a case report. Radiol Case Rep 2020 Aug;15(10):1743-1746.