Traumatic pulmonary pseudocysts (TPPs) (or pulmonary pneumatoceles) are rare parenchymal lung lesions with a cavitary structure, but no epithelial walls. TPPs form as a result of blunt thoracic trauma and are reported to occur in 0.1% of all chest traumas.1 They are usually associated with high-energy injuries sustained in traffic accidents and falls. A typical cyst structure is formed by the accumulation of air or fluid in the cavity formed by the rupture of the lung parenchyma as a result of blunt thoracic trauma. In adults, blunt thoracic trauma can cause chest wall injuries, bone fractures, or lung injuries.2 The greater elasticity of the thoracic wall in children and adolescents renders them more vulnerable to injury to the lung parenchyma. Thus, pediatric and adolescent parenchymal lung injuries are more likely to occur without rib fractures, with more likelihood of TPP formation in thoracic trauma. Furthermore, since pathologies such as pneumothorax and pneumomediastinum may occur simultaneously in the same chest injury, TPPs may be confused with those. In contrast to these pathologies, TPPs are generally benign and do not require intervention. This highlights the importance of recognizing TPPs to avoid incorrect interventions including surgery.3 We report a rare case of TPP with simple pneumothorax and scapula fracture caused by blunt thoracic trauma in a seven-year-old patient.
Case Report
A seven-year-old boy presented to the emergency department after being hit by a vehicle while riding a bicycle. He took the impact on the left side of his chest, causing him to fall to his right side. The Glasgow Coma Scale of the patient was 15, arterial blood pressure was 123/73 mmHg, pulse was 89 beats/minute, and oxygen saturation was 96%. Physical examination revealed multiple abrasion sites sized 2–5 cm on the right parietal scalp, right shoulder, right elbow, and right hip. It was observed that breath sounds decreased in the left hemithorax, and the right shoulder had limited movement and was painful on palpation. There were no pathological signs in his neurological, abdominal, or vertebral examinations. A fracture of the right scapula was detected in the X-ray [Figure1], which also gave the suspicion of a cavitary structure in the left lung. Accordingly, the patient underwent thorax computed tomography (CT) which detected a pulmonary pseudocyst, contusions in the upper lobe of the left lung, and simple pneumothorax [Figure 2]. No pathology was detected using CT in the brain, abdomen, or vertebra. The injury severity score of the patient was estimated at 13.
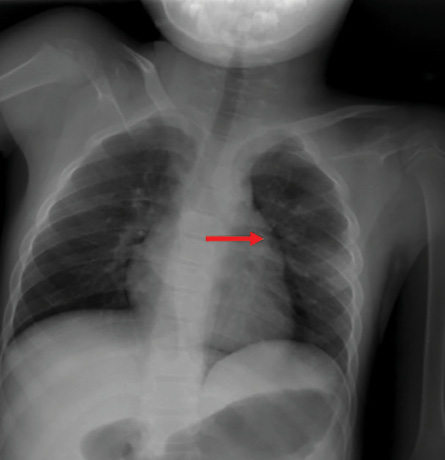 Figure 1: A cavitary lesion (red arrow) is seen in the upper lobe of the left lung on the chest X-ray taken at the time of admission.
Figure 1: A cavitary lesion (red arrow) is seen in the upper lobe of the left lung on the chest X-ray taken at the time of admission.
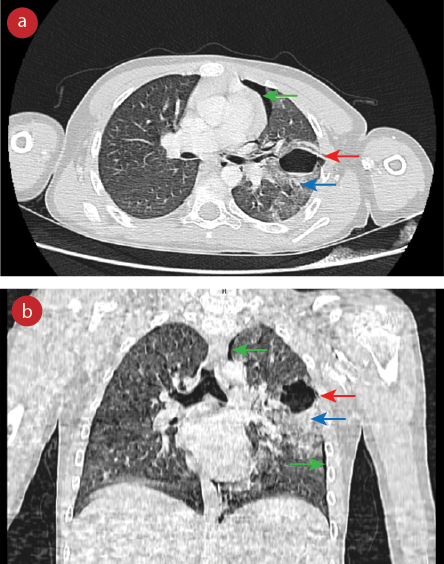 Figure 2: (a) Axial and (b) coronal thorax CT sections show a 3 × 3 cm traumatic pulmonary pseudocyst (red arrows) in the upper lobe of the left lung, without a clear wall, containing an air-fluid level surrounded by a contusion (blue arrows), and a simple pneumothorax (green arrows).
Figure 2: (a) Axial and (b) coronal thorax CT sections show a 3 × 3 cm traumatic pulmonary pseudocyst (red arrows) in the upper lobe of the left lung, without a clear wall, containing an air-fluid level surrounded by a contusion (blue arrows), and a simple pneumothorax (green arrows).
In view of the pseudocyst and simple pneumothorax, it was decided to hospitalize the child and follow-up with daily chest X-rays. The scapula fracture was treated by applying a Velpeau bandage. The patient’s C-reactive protein value, which was 0.1 mg/dL (normal range = 0.0–0.5 mg/dL) at admission, rose to 2.8 mg/dL on the second day. He was started on a prophylactic antibiotic (ampicillin sulbactam, 1 g intravenously, twice a day for four days). After five days of follow-up, the patient was discharged due to the absence of complications on the chest X-ray [Figure 3].
 Figure 3: Chest X-ray taken on the fifth day shows that the pseudocyst has not enlarged and the absence of complications.
Figure 3: Chest X-ray taken on the fifth day shows that the pseudocyst has not enlarged and the absence of complications.
Discussion
Since the ossification of the ribs is not complete in children and adolescents, the compliance of the chest wall is high. The elasticity of the chest wall causes traumatic energy to be transmitted to the underlying parenchymal structures without causing rib fractures, unlike in adults. This poses a particular risk in pediatric patients for parenchymal damage in blunt chest trauma.4 As for the mechanism of formation of TPPs, it is accepted that the energy transmitted from the chest wall causes parenchymal tears. The tears enlarge and form cavities; increasing the intrathoracic pressure.5 This also explains why some authors found the incidence of TPP higher. For example, Armstrong et al,6 found the incidence of TPP to be 12% among a sample of 204 children, all of whom had a pulmonary contusion. Thus, it can be said that all of these patients had severe chest trauma, and this ratio does not represent the incidence of TPP among all chest injuries. In our patient, TPP was similarly formed as a result of blunt chest injury without a rib fracture.
TPPs are classified as subpleural or intraparenchymal according to their location. Intraparenchymal TPPs are associated with younger ages, higher trauma severity, and more concomitant injuries. Intraparenchymal TPPs risk being confused with bullae, congenital cysts, abscesses, or pneumothorax, as in the current case. We could not clearly differentiate the cavitary lesion on the first chest X-ray on the presentation from the above-mentioned pathologies. This led us to opt for a thorax CT, which was confirmatory. It has been reported that half or fewer of TPPs can be recognized in chest X-rays in the early post-traumatic period.7 Although CT devices are now ubiquitous, they cannot be performed on all thoracic traumas in children. Hence, the importance of being able to recognize TPPs.
Various lung injuries and extra-thoracic injuries may accompany TPPs.8 There are two major risks arising from this: TPPs can be confused with other pathologies such as pneumothorax, and TPPs may be treated similarly to other pathologies. Incorrect interventional procedures such as tube thoracostomy may cause increased morbidity and mortality. TPPs usually resolve spontaneously within 3–6 months.9 In our patient, we monitored the TPP and other lung pathologies for five days without any intervention. In addition to analgesics, prophylactic antibiotics were started because of the increased C-reactive protein level on the second day. After five days of follow-up, the patient was discharged without complications.
Conclusion
TPPs can occur with blunt thoracic trauma and risk being confused with other traumatic pathologies. In particular, pediatric patients are at risk. To prevent misinterpretation and mistreatment, emergency physicians should develop knowledge and skills to recognize and manage TTPs.
Disclosure
The authors declared no conflicts of interest. Informed consent was obtained from the patient’s parents for the use of all information and images.
references
- 1. Athanassiadi K, Gerazounis M, Kalantzi N, Kazakidis P, Fakou A, Kourousis D. Primary traumatic pulmonary pseudocysts: a rare entity. Eur J Cardiothorac Surg 2003 Jan;23(1):43-45.
- 2. Albulushi A, Kadir S, Barton D, Chatzizisis YS, O’Leary E. Blunt chest trauma presenting with acute coronary event. Oman Med J 2021 May;36(3):e275.
- 3. Cho HJ, Jeon YB, Ma DS, Lee JN, Chung M. Traumatic pulmonary pseudocysts after blunt chest trauma: prevalence, mechanisms of injury, and computed tomography findings. J Trauma Acute Care Surg 2015 Sep;79(3):425-430.
- 4. Sartorelli KH, Vane DW. The diagnosis and management of children with blunt injury of the chest. Semin Pediatr Surg 2004 May;13(2):98-105.
- 5. Phillips B, Shaw J, Turco L, McDonald D, Carey J, Balters M, et al. Traumatic pulmonary pseudocyst: an underreported entity. Injury 2017 Feb;48(2):214-220.
- 6. Armstrong LB, Mooney DP. Pneumatoceles in pediatric blunt trauma: common and benign. J Pediatr Surg 2018 Jul;53(7):1310-1312.
- 7. Ozsoy IE, Tezcan MA. Unusual cavitary lesions of the lung: analysis of patients with traumatic pulmonary pseudocyst. North Clin Istanb 2020 Aug;8(1):82-87.
- 8. Luo L, Yin L, Liu Z, Xiang Z. Posttraumatic pulmonary pseudocyst: computed tomography findings and management in 33 patients. J Trauma Acute Care Surg 2012 Nov;73(5):1225-1228.
- 9. Melloni G, Cremona G, Ciriaco P, Pansera M, Carretta A, Negri G, et al. Diagnosis and treatment of traumatic pulmonary pseudocysts. J Trauma 2003 Apr;54(4):737-743.