Cardiac arrest is one of the leading causes of death worldwide and is therefore an important public health issue.1 Advanced cardiac life support (ACLS) is paramount in the management of cardiac arrest. Cardiopulmonary resuscitation (CPR) is a basic life-saving technique involving chest compression and artificial ventilation. Knowledge and training of CPR skills allow for bystanders and health personnel to respond immediately and adequately to a cardiac arrest event.2 In 1974, the American Heart Association (AHA) published its first ACLS guidelines, followed by other organizations such as the International Liaison Committee on Resuscitation and European Resuscitation Council.3 Collaboration between these entities resulted in further updates and revisions to these guidelines to create an effective and easy approach to the provision of ACLS.4
Nevertheless, knowledge and guidelines alone are not sufficient to ensure optimal CPR skills and practices. This is crucial as cardiac arrest outcomes have been linked to the quality of CPR practices.5,6 As such, significant resources have been allocated towards ACLS training to ensure high-quality CPR practices.2,3 According to the AHA guidelines, high-quality CPR is defined as: (1) a chest compression rate of at least 100 compressions per minute, (2) a compression depth of at least 5 cm in adults, (3) complete chest recoil after each compression, (4) minimizing chest compression interruptions, and (5) avoiding excessive ventilation.2 High-quality CPR ensures adequate coronary perfusion pressure, myocardial blood flow, and myocardial oxygen delivery during a cardiac arrest event, thereby improving patient survival and outcome.2,7
Various efforts have been undertaken to translate CPR knowledge and guidelines into practice, such as CPR-recording devices, large cardiac arrest event registries, and high-fidelity basic life support (BLS) and ACLS simulations.7 Nevertheless, CPR remains a complex skill that is often performed inefficiently or incorrectly during a cardiac arrest event, meaning that “the quality of care provided during resuscitation attempts frequently does not meet quality of care standards”.8 To achieve high quality CPR, it is necessary to use and integrate cognitive, behavioral, and psychomotor skills. In 2010, many resuscitation guidelines addressed the importance of continuous education and improvement, emphasizing the necessity of delivering high-quality CPR and maintaining CPR skills over time.3,9,10
As with most other skills, CPR needs to be practiced regularly to achieve proficiency.4,8 BLS certification courses aim to consolidate the five components of high-quality CPR, with research showing a significant retention in CPR skills following completion of a BLS course.9 However, traditional BLS training highlights the importance of recertification every two years, an interval which organizations such as the AHA consider to be too lengthy to ensure optimal skill retention.4 Indeed, CPR skills and knowledge have been found to deteriorate within 6–12 months of the initial BLS training, with some research showing that this deterioration may occur in as little as three months.10–12 Others indicate that BLS and ACLS certification may not translate to adequate performance during actual arrest events, particularly for providers who do not encounter many cardiac arrest events.2,9,10 As of yet, there is no consensus in the existing literature to support a standardized timing and format for refresher CPR training. Therefore, this study aimed to assess the effectiveness of a short BLS refresher training course, after six months from the initial training, on the retention of CPR-related psychomotor skills.
Methods
This prospective, non-blinded, randomized clinical trial was conducted from February 2018 to August 2020 at the Emergency Department of the Sultan Qaboos University Hospital (SQUH), Muscat, Oman. The enrolled participants consisted of healthcare workers (including nurses, doctors, and paramedics) who had prior exposure to CPR training. Those with medical illnesses or conditions that might interfere with chest compressions (such as back, wrist, or knee pain), pregnant women, and providers scheduled for recertification training during the study period were excluded.
In view of the different backgrounds of participants, in terms of experience and practice, block randomization was used to allocate participants. Candidates were divided to the intervention or control groups based on years of experience (< 10 and > 10 years). Sealed envelopes opened by third parties were used to allocate participants in each group.
At the start of the trial, all participants were assessed to determine their baseline CPR skills. They were asked to perform two minutes of CPR on a manikin using a QCPR monitoring device (Laerdal Corp., Stavanger, Norway). Subsequently, all participants received feedback based on their performance and were asked to practice their CPR skills until they had achieved 100%. This assured that all participants had similar performance at the beginning of the study. Six months later, the participants were once again asked to perform two minutes of CPR. At this point, the intervention group received feedback on their performance and underwent a brief CPR refresher training course until they achieved 100% performance. In contrast, no training or feedback was given to the control group. Finally, 12 months after the initial baseline assessment, all participants underwent a final assessment. At each stage, Little Anne® QCPR manikins (Laerdal Corp., Stavanger, Norway) with QCPR monitors were used to measure chest compression rate, depth, chest recoil, interruption, and ventilation to assess overall CPR performance [Figure 1].
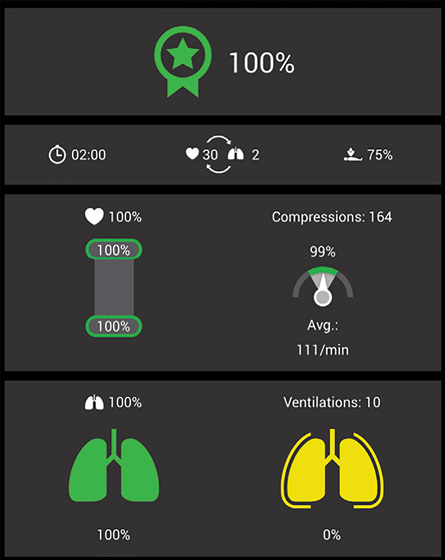 Figure 1: QCPR monitor screen.
Figure 1: QCPR monitor screen.
The primary outcome of the trial was to assess the effectiveness of CPR refresher training at six months on the retention of CPR-related psychomotor skills. Participants were assessed based on the five components of high-quality CPR, including compression rate (compressions/minute) depth (percentage), recoil (percentage), ventilation (percentage), and interruption time (seconds). These variables were assessed at the time of enrolment (i.e., at baseline) and then again at six and 12 months from the time of enrolment. Knowledge of high-quality CPR was assessed before the skills assessment using a short questionnaire involving four multiple-choice questions.
Data were analyzed for all cases using SPSS (SPSS Inc. Released 2007. SPSS for Windows, Version 13.0. Chicago, SPSS Inc.). Categorical data were summarized using frequency and percentage, whereas continuous data were summarized as means and SDs. Comparisons of CPR performance between the two groups were performed using an independent samples t-test and Fisher’s exact test. A p-value of < 0.05 was regarded as statistically significant.
The protocol for this study was approved by the local research ethics committee of SQUH. The study was funded by a research grant from the College of Medicine and Health Sciences at Sultan Qaboos University (#SQU-EC/023/18). All participants provided informed verbal consent prior to enrolment in the trial.
Results
A total of 59 participants were randomized and 38 were included in the study (retention rate: 64.4%). Of those remaining, 19 were assigned to the intervention group and 19 to the control group [Figure 2]. The demographic data of the participants are summarized in Table 1. Overall, there were 10 (26.3%) BLS instructors, with four (21.1%) assigned to the intervention group and six (31.6%) to the control group. All participants, regardless of group allocation, actively participated in resuscitations during their work. Baseline knowledge of CPR was comparable in both groups.
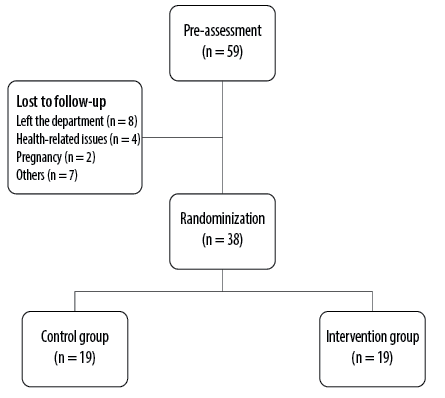 Figure 2: Overview of the study design and flow of participants through the study.
Figure 2: Overview of the study design and flow of participants through the study.
Table 1: Baseline characteristics of the participants.
|
Age, mean ± SD, years
|
36.7 ± 6.0
|
33.4 ± 5.7
|
|
|
Sex
|
|
|
1.000
|
|
Male
|
9 (47.4)
|
10 (52.6)
|
|
|
Female
|
10 (52.6)
|
9 (47.4)
|
|
|
Profession
|
|
|
0.195
|
|
Nurse
|
9 (47.4)
|
12 (63.2)
|
|
|
Physician
|
8 (42.1)
|
7 (36.8)
|
|
|
Paramedic
|
2 (10.5)
|
0 (0.0)
|
|
|
Experience, years
|
|
|
1.000
|
|
< 10
|
10 (52.6)
|
10 (52.6)
|
|
|
≥ 10
|
9 (47.4)
|
9 (47.4)
|
|
|
BLS status
|
|
|
0.714
|
|
Instructor
|
4 (21.1)
|
6 (31.6)
|
|
|
Provider
|
15 (78.9)
|
13 (68.4)
|
|
|
Involvement in active resuscitations
|
|
Yes
|
19 (100)
|
19 (100)
|
|
|
No
|
0 (0.0)
|
0 (0.0)
|
|
|
Knowledge of CPR
|
|
CVR in single-rescuer adult CPR
|
|
Correct
|
18 (94.7)
|
18 (94.7)
|
|
|
Incorrect
|
1 (5.3)
|
1 (5.3)
|
|
|
CC depth
|
|
|
|
|
Correct
|
17 (89.5)
|
19 (100)
|
|
|
Incorrect
|
2 (10.5)
|
0 (0.0)
|
|
|
Maximal interval for pausing CC
|
|
Correct
|
19 (100)
|
19 (100)
|
|
|
Incorrect
|
0 (0.0)
|
0 (0.0)
|
|
|
Target ventilation rate during CPR
|
|
Correct
|
14 (73.7)
|
14 (73.7)
|
|
BLS: basic life support; CVR: compression-to-ventilation ratio;
CC: chest compressions.
At baseline, both groups demonstrated similar CPR skills, with a mean overall performance of 72.7±12.9% in the intervention group versus 75.8±25.2% in the control group (p = 0.638). At six months, both groups showed an improvement in their overall performance compared to baseline, with a mean of 87.2±7.2% in the intervention group and 88.5±11.1% in the control group (p = 0.682). However, at 12 months, there was a significant difference in the mean overall performance of the intervention group compared to the control group (93.8±5.9% vs. 79.4±21.3%; p = 0.010). There were significant differences between the two groups in terms of ventilation (p = 0.028) and interruption time (p = 0.020) [Table 2].
Table 2: Performance assessment.
|
At baseline
|
|
|
|
|
CC rate, compressions/minute
|
127.2 ± 11.3
|
122.1 ± 13.7
|
0.220
|
|
CC depth, %
|
91.6 ± 16.3
|
95.9 ± 7.8
|
0.315
|
|
Chest recoil, %
|
89.1 ± 25.2
|
81.5 ± 31.0
|
0.415
|
|
Ventilation, %
|
73.7 ± 26.3
|
80.3 ± 18.5
|
0.383
|
|
Interruption time, sec, n (%)
|
|
|
|
≤ 10
|
17 (89.5)
|
15 (78.9)
|
0.660
|
|
> 10
|
2 (10.5)
|
4 (21.1)
|
|
|
Overall performance, %
|
72.7 ± 12.9
|
75.8 ± 25.2
|
0.638
|
|
At six months
|
|
|
|
|
CC rate, compressions/minute
|
113.9 ± 11.8
|
114. ± 11.6
|
0.845
|
|
CC depth, %
|
94.7 ± 12.4
|
96.8 ± 10.8
|
0.591
|
|
Chest recoil, %
|
88.8 ± 25.3
|
96.8 ± 5.9
|
0.195
|
|
Ventilation, %
|
85.1 ± 22.2
|
79.0 ± 34.2
|
0.518
|
|
Interruption time, sec, n (%)
|
|
|
|
≤ 10
|
15 (78.9)
|
18 (94.7)
|
0.340
|
|
> 10
|
4 (21.1)
|
1 (5.3)
|
|
|
Overall performance, %
|
87.2 ± 7.2
|
88.5 ± 11.1
|
0.682
|
|
At one year
|
|
|
|
|
CC rate, compressions/minute
|
115.8 ± 15.1
|
112.1 ± 13.7
|
0.425
|
|
CC depth, %
|
99.5 ± 0.8
|
92.6 ± 14.4
|
0.050
|
|
Chest recoil, %
|
97.7 ± 6.0
|
89.8 ± 17.4
|
0.075
|
|
Ventilation, %
|
93.1 ± 9.8
|
76.3 ± 29.4
|
0.028*
|
|
Interruption time, sec, n (%)
|
|
|
|
≤ 10
|
13 (68.4)
|
19 (100)
|
0.020*
|
|
> 10
|
6 (31.6)
|
0 (0.0)
|
|
CC: chest compressions. *Statistically significant using an independent samples t-test and Fisher’s exact test.
Discussion
This study showed that a short refresher BLS training course, six months after initial training, resulted in a higher retention of high-quality CPR, mainly ventilation (p = 0.028) and interruption time (p = 0.020). Overall CPR performance was superior in the intervention group compared to the control group. In contrast, the control group demonstrated a decline in performance at 12 months, likely because of the deterioration of skills over the one-year interval from the initial training. The study showed that both groups demonstrated comparable knowledge of CPR at baseline, with a noticeable knowledge gap in terms of target ventilation rate.
The findings of this study are consistent with those of previous research showing a decline in CPR quality and performance at 12 months.10,11 Alarmingly, some researchers have shown that the loss of CPR-related skills may occur as early as three to six months after initial BLS training.10 However, no decline in psychomotor skills was found at six months in our study. This could be explained by the initial baseline training; in addition, all participants were emergency staff who were actively involved in resuscitations. No difference was observed in overall performance between participants with < 10 or ≥ 10 years experience. Further studies are needed to support these findings regarding the retention of CPR skills over time; such studies should involve larger sample sizes and staff employed in different hospital departments other than the emergency department.
Although the AHA emphasizes the necessity of frequent training for BLS providers to maintain relevant skills, no specific recommendation is given in terms of the frequency or modality of refresher CPR training.2 Various studies have suggested that a short refresher training course two to six months from the initial training may be a practical solution to overcome the problem of deterioration in CPR skills.13–16 Most researchers conclude that refresher courses should not be delayed beyond seven months.17 Niles et al,13 recommended refresher training focusing on chest compressions alone in which participants underwent brief in situ ῾rolling refresher’ training using audio-visual feedback every 2–3 months; the training was found to significantly improve the quality of chest compressions among nurses. Another study similarly found that 15-minute refresher BLS training at six months significantly increased chest compression rate (p = 0.009) and significantly reduced time without compressions (p < 0.001) during a two-minute case-based scenario 12 months after the initial training.14 Other researchers have recommended alternative approaches to refresher BLS training, such as six-minute monthly practice sessions using a voice advisory manikin and frequent ῾rolling refresher’ sessions using a portable manikin/defibrillator system with automated feedback.15,16
In this study, the modality adopted was a short, simplified, monitored, hands-on refresher training course in which participants underwent a two-minute cycle with a feedback device until they achieved 100% performance. Most participants required 2–3 cycles to achieve this target. Hence, this approach was found to be a feasible and cost-effective method of CPR refresher training. In addition, we found comparable results with previously conducted studies despite differences in population and refresher training modality. Considering the critical importance of high-quality CPR to cardiac arrest outcomes, and because there is no direct monitoring of CPR quality and performance apart from during refresher training, healthcare facilities must ensure that BLS providers retain and master these skills throughout their practice. In addition, providers who encounter fewer cardiac arrest events during their practice may demonstrate a more rapid loss of CPR skills after training and thus may benefit from more frequent refresher training.2,4
This study is not without limitations. It was a single-center study with a small sample size. The small sample size was mainly due to the loss of participants to follow-up at the six-month assessment. This was due to the development of exclusion criteria in certain participants (e.g., pregnancy and musculoskeletal pain), staff leaving the department and disruptions to the study protocol as a result of the ongoing COVID-19 pandemic. Therefore, the study might be underpowered due to the small sample size.
Conclusion
A short BLS refresher training course involving a two-minute CPR cycle with a feedback device six months after initial training was found to significantly improve the retention of CPR-related psychomotor skills at 12 months. This study underlines the importance of regular refresher training before the traditional two-year recertification period. A brief, simple, and cost-effective refresher course is crucial to achieve high-quality CPR practices, the ultimate objective of advanced life support procedures.
Disclosure
The authors declared no conflicts of interest. The study was funded by the College of Medicine and Health Sciences at Sultan Qaboos University (research grant #SQU-EC/023/18).
references
- 1. Paratz ED, Rowsell L, Zentner D, Parsons S, Morgan N, Thompson T, et al; Australian UCDP Registry. Cardiac arrest and sudden cardiac death registries: a systematic review of global coverage. Open Heart 2020 Jan;7(1):e001195.
- 2. Meaney PA, Bobrow BJ, Mancini ME, Christenson J, de Caen AR, Bhanji F, et al; CPR Quality Summit Investigators, the American Heart Association Emergency Cardiovascular Care Committee, and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American heart association. Circulation 2013 Jul;128(4):417-435.
- 3. Hermreck AS. The history of cardiopulmonary resuscitation. Am J Surg 1988 Dec;156(6):430-436.
- 4. Bhanji F, Donoghue AJ, Wolff MS, Flores GE, Halamek LP, Berman JM, et al. Part 14: education: 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015 Nov;132(18)(Suppl 2):S561-S573.
- 5. Stiell IG, Brown SP, Christenson J, Cheskes S, Nichol G, Powell J, et al; Resuscitation Outcomes Consortium (ROC) Investigators. What is the role of chest compression depth during out-of-hospital cardiac arrest resuscitation? Crit Care Med 2012 Apr;40(4):1192-1198.
- 6. Kaplow R, Cosper P, Snider R, Boudreau M, Kim JD, Riescher E, et al. Impact of CPR quality and adherence to advanced cardiac life support guidelines on patient outcomes in in-hospital cardiac arrest. AACN Adv Crit Care 2020 Dec;31(4):401-409.
- 7. Abella BS. High-quality cardiopulmonary resuscitation: current and future directions. Curr Opin Crit Care 2016 Jun;22(3):218-224.
- 8. Sutton RM, Nadkarni V, Abella BS. “Putting it all together” to improve resuscitation quality. Emerg Med Clin North Am 2012 Feb;30(1):105-122.
- 9. Yang CW, Yen ZS, McGowan JE, Chen HC, Chiang WC, Mancini ME, et al. A systematic review of retention of adult advanced life support knowledge and skills in healthcare providers. Resuscitation 2012 Sep;83(9):1055-1060.
- 10. Soar J, Monsieurs KG, Ballance JH, Barelli A, Biarent D, Greif R, et al. European resuscitation council guidelines for resuscitation 2010 section 9. Principles of education in resuscitation. Resuscitation 2010 Oct;81(10):
1434-1444.
- 11. Avisar L, Shiyovich A, Aharonson-Daniel L, Nesher L. Cardiopulmonary resuscitation skills retention and self-confidence of preclinical medical students. Isr Med Assoc J 2013 Oct;15(10):622-627.
- 12. Rajeswaran L, Cox M, Moeng S, Tsima BM. Assessment of nurses’ cardiopulmonary resuscitation knowledge and skills within three district hospitals in Botswana. Afr J Prm Health Care Fam Med 2018;10(1):1-6.
- 13. Niles DE, Nishisaki A, Sutton RM, Elci OU, Meaney PA, O-Connor KA, et al. Improved retention of chest compression psychomotor skills with brief “rolling refresher” training. Simul Healthc 2017 Aug;12(4):213-219.
- 14. Nishiyama C, Iwami T, Murakami Y, Kitamura T, Okamoto Y, Marukawa S, et al. Effectiveness of simplified 15-min refresher BLS training program: a randomized controlled trial. Resuscitation 2015 May;90:56-60.
- 15. Oermann MH, Kardong-Edgren SE, Odom-Maryon T. Effects of monthly practice on nursing students’ CPR psychomotor skill performance. Resuscitation 2011 Apr;82(4):447-453.
- 16. Niles D, Sutton RM, Donoghue A, Kalsi MS, Roberts K, Boyle L, et al. “Rolling Refreshers”: a novel approach to maintain CPR psychomotor skill competence. Resuscitation 2009 Aug;80(8):909-912.
- 17. Broomfield R. A quasi-experimental research to investigate the retention of basic cardiopulmonary resuscitation skills and knowledge by qualified nurses following a course in professional development. J Adv Nurs 1996 May;23(5):1016-1023.