Introduction
Primary malignant melanoma of the esophagus is a very rare neoplasm accounting for less than 0.2% of all esophageal tumors. Due to its rarity, the treatment protocols are not well defined. In a good surgical risk patient with non-metastatic disease, a radical esophagectomy is the preferred treatment option. We herein report a patient with malignant melanoma of the esophagus who was managed by thoracolaparoscopic esophagectomy.
Case Report
A 62 yr old female presented with painless progressive dysphagia of 1 month duration. At the time of presentation, she was able to swallow semisolids with difficulty. There was no history of cough, hoarseness of voice, anorexia or weight loss. The patient was evaluated with an esophagoscopy that revealed a polypoidal mass in the lower esophagus, 32 cm from incisors, with black pigmentation at the base (Fig. 1a). A biopsy was taken which suggested malignant melanoma. Further staging with a contrast enhanced CT scan of the thorax and abdomen showed an intra luminal polypoidal mass in the lower esophagus with no mediastinal, abdominal or periesophageal lymphadenopathy (Fig 1b). There were no other cutaneous, ocular or mucosal melanotic lesions and a diagnosis of primary esophageal malignant melanoma was made. A total thoraco-laparoscopic esophagectomy with regional lymphadenectomy and a cervical esophagogastric anastomosis was done (Fig 2). The patient recovered well and the final histopathology confirmed a malignant melanoma of the esophagus confined to the esophageal wall (pT2N0M0) (Figs. 3a & b)
Discussion
A primary malignant melanoma of the esophagus is rare, accounting for less than 0.1-0.2% of all esophageal tumors.1,2 It arises from the scattered mucosal melanocytes and is most commonly located in the mid and the lower third of the esophagus. The tumor tends to grow in the mucosal and submucosal layer; however, deeper infiltration into the muscular layers of the esophagus can occur. Macroscopically, the tumor usually presents as a polypoid mass, which is focally ulcerated but mostly covered by intact squamous mucosa. It is considered to be primarily arising from the esophagus when the mass has a characteristic structure of a melanoma that contains melanin, the adjacent epithelium contains melanocytes, the tumor is polypoidal, and arises from the area of junctional changes in the squamous epithelium.3 Recently, immunohistochemical (IHC) staining, which utilizes antibodies that are specific to HMB-45 and/or S-100 cytoplasmic protein, have been used to identify malignant melanoma within the esophagus.4,5 In a good surgical risk patient, an esophagectomy with regional lymphadenectomy with or without adjuvant chemotherapy is the preferred treatment option.

Figure 1a: Esophagoscopy showing a polypoidal mass lesion arising at 32 cm from incisors. Black pigmentation is visible at the base.

Figure 1b: Contrast enhanced CT scan showing a polypoidal mass in the esophagus with no regional lymphadenopathy and maintained planes with adjacent structures.

Figure 2: The resected specimen of esophagus with a pedunculated fleshy pigmented tumors at the lower end
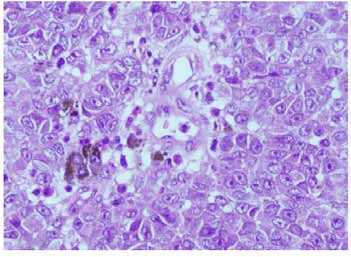
Figure 3a: Large cells with prominent nucleoli with black pigment in the cytoplasm (HE, 40x)
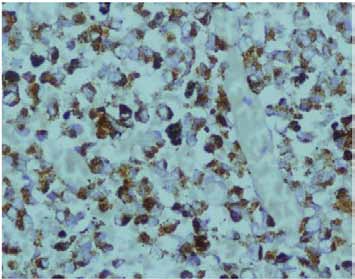
Figure 3b: Immunohistochemical staining with HMB-45, 20x, highlighting the melanoma cells.
Acknowledgements
The author reported no conflict of interest and no funding was received in this work.
References
1. Chang F, Deere H. Esophageal melanocytosis morphologic features and review of the literature. Arch Pathol Lab Med 2006 Apr;130(4):552-557.
2. Sabanathan S, Eng J, Pradhan GN. Primary malignant melanoma of the esophagus. Am J Gastroenterol 1989 Dec;84(12):1475-1481.
3. Allen AC, Spitz S. Malignant melanoma; a clinicopathological analysis of the criteria for diagnosis and prognosis. Cancer 1953 Jan;6(1):1-45.
4. Stranks GJ, Mathai JT, Rowe-Jones DC. Primary malignant melanoma of the oesophagus: case report and review of surgical pathology. Gut 1991 Jul;32(7):828-830.
5. Gao N, Li L-J, Li Y, Wang L. Primary amelanotic malignant melanoma of the parotid gland: a case report. J Int Med Res 2008 Nov-Dec;36(6):1435-1439.
|