Malaria is a global health concern with 241 million malaria cases reported worldwide in 2020, and 627 000 fatalities.1 In 2015, the World Health Organization (WHO) launched the Global Technical Strategy for Malaria 2016–2030.2,3 They also supported 21 malaria-free countries launch a unique program known as the ῾E-2020’ in 2017. Of these, eight ῾E-2020’ member countries recorded zero indigenous (autochthonous) malaria cases.4 The Eastern Mediterranean Region (EMR) developed the tailored Action Plan on Malaria Control and Elimination 2016–2020 to implement this strategy at the regional level.5
Omani national malaria program: milestones
Malaria has historically been a key public health concern in Oman. The occurrence of malaria was first documented in the early 19th century by Major Clifford Gill.6 In his written records of troops stationed in Muscat, he noted for every 1000 soldiers admitted to the hospital each month, 100–400 soldiers were admitted with fever from infection with Plasmodium falciparum. Similarly, a review of malaria morbidity data among civilians from the Agency Hospital in Muscat between 1900–1915 revealed that cases of fever increased in 1905 compared to previous years, coinciding with an increase in annual rainfall in 1905.6
In December 1915, a survey to estimate the rate of spleen enlargement in children < 10 years of age in villages near Muscat found the prevalence of malaria was higher in Muscat and Muttrah.6 From the mid-1970s to the late 1980s, malaria remained a serious public health problem in Oman with clinical malaria cases accounting for 50% of all communicable diseases identified during these years.7
Program development
In 1973, malariometric surveys found that most of Oman’s northern regions were mesoendemic. The highest reported infection rates in the Al Batinah governorate (province) and southern regions were malaria-free or hypoendemic.8–10 With the data from this survey, the Ministry launched the Malaria Control Programme in January 1975.11 In 1978, 17 malaria control units were established; and two years later, the malaria training center began operations to train health staff, providing required knowledge and skills at this state-of-the-art facility. In 1979, > 90% of infections were attributed to P. falciparum, P. vivax, and P. malariae with only one case of P. ovale reported.6
The first phase of the control program focused on biological control of larvae. Consequently, the program switched to larviciding with temephos following a pilot project along the coastal strip and extended into other areas from 1977 to 1979.
A key feature of the vector control program since 1975 is the detailed mapping of risk areas using aerial photographs to inform larval control.8 Mapping activities were followed by a comprehensive control approach that included source reduction, biological control with native larvivorous fish, and DDT residue spraying. These tools were initially introduced in small village-scale trials to assess their individual or combined effects on vector population densities.9
In 1976, residual DDT spraying extended to Shinas, Al Batinah governorate, the Dhank region, and the Buraimi governorate border with the UAE.4 Unfortunately, the indoor residual spraying (IRS) campaign never achieved full coverage. In Al Batinah governorate, annual rounds of DDT spraying in houses decreased from 90% in 1976 to < 50% in 1981.5
The IRS program ended in Muscat in 1980 and Salalah City in 1981. In 1982, prophylaxis was discontinued in areas protected by DDT due to the fear of emerging resistance and was reserved for the use of pregnant women and young children5 as resistance was detected in larvae of Anopheles culicifacies in 1980.8
The use of DDT was replaced by fenitrothion in 1993 due to technical difficulties in maintaining high coverage, as well as increasing DDT resistance. Fenitrothion remained the insecticide of choice until 1992 when the program began systematic replacement with pyrethroid through 1999. Permethrin 2.5% emulsifiable concentrate (EC) was utilized from 1992 until 1996 when it was replaced with lamda-cyhalothrin 10% wettable powder (WP).1
Oman is in the African-Arab epidemiological zone of the natural distribution of malaria vectors, where the malaria vectors: An. culicifacies, An. fluviatilis, An. Stephensi, and An. sergenti are of low vectorial capacity.11,12 Cemented water reservoirs, wells, and water collections in rainy creeks, known locally as wadis have been important breeding grounds for malaria vectors and the main tool of malaria vector control was larviciding beginning in 1975 with temephos.7
The National Malaria Eradication Programme (NMEP) in Oman was launched in 1991 as a pilot project in A’Sharqiya governorate and was extended to the rest of the country in phases. The objective of the NMEP was to reach to an annual parasite incidence (API) of 0.1/1000 population by the year 2000 through vector control, early case detection, and prompt, radical cure of cases. Weekly larviciding was the major vector control method, mainly chemical control, but larvivorous fish were used where feasible. Larviciding was based on geographical reconnaissance with detailed maps of breeding sites. Other vector control methods, namely IRS, space spraying, and environmental management were complementary to larviciding.
The program used an early case detection strategy consisting of passive case detection (PCD), active case detection (ACD), and quality control. All strategies informed the surveillance system, PCD involved case reporting by public (government) and private health institutions, and ACD included epidemiological contact surveys (ECS), mass surveys, school surveys, and screening passengers arriving from malaria-endemic countries. Quality control of malaria diagnostic services used malaria microscopy as the gold standard and ensured all parasitological positive malaria cases across the country were checked.
Socioeconomic development factors that contribute to reducing autochthonous (endogenous) cases
In Oman, socioeconomic growth played a significant role in reducing local cases. The rise in the standard of living, with better housing and availability of electricity, reduced vector-human interaction. Also, improved water supply to homes and advancements in agriculture irrigation technologies have reduced vector habitats.
Oman is a malaria-free country, meeting WHO requirements with no indigenous malaria cases documented since 2010.12 To retain this position, all efforts are focused on preventing malaria re-establishment. There are few published malaria reports in Oman13–19 describing the malaria elimination initiative in Oman.19 The principal objective of this paper is to provide a retrospective analysis of the epidemiological characteristics and trends of malaria cases detected between 1976 and 2020. This epidemiological profile will assist in the assessment of malaria risk in Oman and in local public health areas, thus improving prevention, diagnosis, and treatment.
Methods
Oman is one of 22 countries within the EMR, located in the southeastern corner of the Arabian Peninsula. The country has a population of nearly five million, of which 39% are non-citizens.20 This national review utilized secondary data available from 1994 to 2020.21
The data was collected from a national database published between 1976 and 2020. Variables were extracted for the total number of malaria cases per year, the number of indigenous, introduced, and imported malaria cases, and their geographical distribution. Case detection activities performed between 1988 and 2020 were evaluated. We reviewed reports from WHO consultants together with global malaria reports that provided information for assessing the malaria situation in Oman.
Patient characteristics were described using frequency and percentage for categorical variables, mean and SD for continuous variables. We used Microsoft Excel for Mac Version 16.52 for data analytics.
We used publicly disclosed and anonymized data; and therefore, the ethical approval was not required as it was based on secondary data extracted from the national malaria surveillance system published in an official domain. This study does not violate the Internal Review Committee and endorses the Helsinki Declaration.
Results
The total number of confirmed malaria case notifications reported from 1976 to 2020 was 298 070 [Figure 1]. During this period, cases declined from 1.6 (3286) to 0.1 (273) per 1000 population.
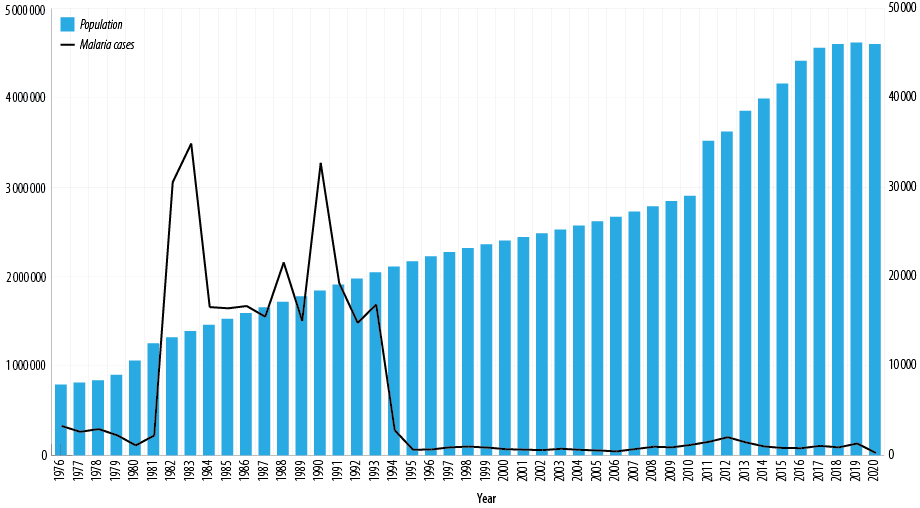 Figure 1: Trend of malaria cases, Oman, 1976–2020.2
Figure 1: Trend of malaria cases, Oman, 1976–2020.2
In 1991, the malaria control program was revitalized and in a 12-year period (1994–2006), there was a 93.0% (7215 to 443) reduction in cases and case rates decreased from 3.6 to 0.2/1000 population. In 1994, the epidemiologic classification of cases was initiated [Table1]. Since 1994, 98.0% of cases have been imported, and the rest were autochthonous malaria cases. In the 20-year period from 2000 until 2020, there have been no deaths due to indigenous malaria cases.
Over a 10-year period, autochthonous cases went from a higher cases in 1994 of 4415 (2.4 per 1000 population) to zero in 2004. This shifted when four autochthonous cases were reported from Al Dakhliya governorate.
In 2007, the total number of malaria notifications rose from 0.3/1000 (705) to 0.8 per 1000 population (2051) in 2012. Thereafter, confirmed cases began to decline until 2020, reaching 0.6 per 1000 population (273 cases). Since 2007, small pockets of local transmission have been detected on an annual basis in various governorates [Table 1].
Table 1: The year, slide positivity rate (SPR), SPR percentage, annual blood examination rate (ABER) percentage of the total population, and annual parasite incedence (API) per 1000 population.
|
1994
|
2 095 770
|
295 194
|
7215
|
2800
|
4415
|
2.4
|
14.6
|
2.188
|
|
1995
|
2 091 420
|
464 091
|
1801
|
617
|
1184
|
0.4
|
21.8
|
0.566
|
|
1996
|
2 135 900
|
527 182
|
1265
|
662
|
603
|
0.2
|
23.8
|
0.282
|
|
1997
|
2 255 630
|
485 184
|
1026
|
897
|
129
|
0.2
|
21.5
|
0.057
|
|
1998
|
2 287 640
|
438 166
|
1091
|
977
|
114
|
0.3
|
19.2
|
0.050
|
|
1999
|
2 325 460
|
496 067
|
901
|
872
|
29
|
0.2
|
21.3
|
0.012
|
|
2000
|
2 401 257
|
494 884
|
694
|
688
|
6
|
0.1
|
20.6
|
0.002
|
|
2001
|
2 477 687
|
521 552
|
635
|
633
|
2
|
0.1
|
21.0
|
0.001
|
|
2002
|
2 537 742
|
495 826
|
590
|
584
|
6
|
0.1
|
19.5
|
0.002
|
|
2003
|
2 340 815
|
409 559
|
740
|
734
|
6
|
0.2
|
17.5
|
0.003
|
|
2004
|
2 415 576
|
326 124
|
615
|
615
|
0
|
0.2
|
13.5
|
0.000
|
|
2005
|
2 508 837
|
258 981
|
544
|
544
|
0
|
0.2
|
10.3
|
0.000
|
|
2006
|
2 577 062
|
223 075
|
443
|
443
|
0
|
0.2
|
9.4
|
0.000
|
|
2007
|
2 743 499
|
244 346
|
705
|
701
|
4
|
0.3
|
8.9
|
0.001
|
|
2008
|
2 867 428
|
245 113
|
965
|
957
|
8
|
0.4
|
8.5
|
0.003
|
|
2009
|
3 173 917
|
234 803
|
898
|
898
|
0
|
0.4
|
7.4
|
0.000
|
|
2010
|
3 237 412
|
226 009
|
1193
|
1169
|
24
|
0.5
|
7.0
|
0.007
|
|
2011
|
3 518 818
|
267 353
|
1531
|
1519
|
13
|
0.6
|
7.6
|
0.004
|
|
2012
|
3 623 001
|
269 990
|
2051
|
2029
|
22
|
0.8
|
7.5
|
0.006
|
|
2013
|
3 855 206
|
230 041
|
1451
|
1440
|
11
|
0.6
|
6.0
|
0.003
|
|
2014
|
3 992 893
|
168 043
|
1001
|
986
|
15
|
0.6
|
4.2
|
0.004
|
|
2015
|
4 159 102
|
198 589
|
822
|
818
|
4
|
0.4
|
4.8
|
0.001
|
|
2016
|
4 414 031
|
203 409
|
807
|
804
|
3
|
0.4
|
4.6
|
0.001
|
|
2017
|
4 559 963
|
162 628
|
1078
|
1059
|
19
|
0.7
|
3.6
|
0.002
|
|
2018
|
4 601 706
|
159 535
|
921
|
891
|
30
|
0.6
|
3.5
|
0.006
|
|
2019
|
4 617 927
|
126 680
|
1338
|
1323
|
15
|
1.0
|
2.7
|
0.003
|
A total of 11 747 cases reported between 2009 and 2019, with 10 228 cases in men and only 1519 cases identified in women. Nearly two-thirds (73.0%) of reported cases 9423 were in adults, aged 20 to 34 years old [Figure 2].
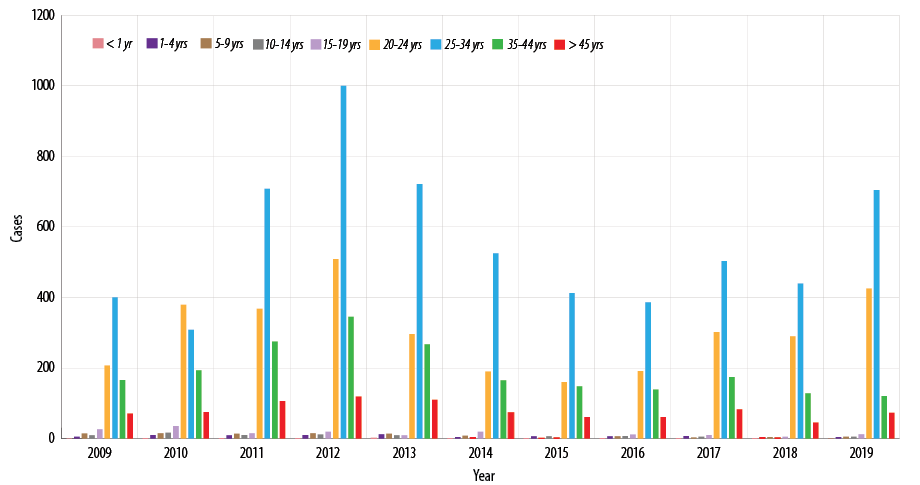 Figure 2: Malaria cases by age group, Oman, 2009–2019.
Figure 2: Malaria cases by age group, Oman, 2009–2019.
In 1997, 897 cases were classified as imported with 448 (49.9%) from Africa and 327 (36.5%) from India with an additional 122 (13.6%) cases coming from other countries. By 2009, there were only 19 cases from Africa representing 2.1% of cases imported while cases imported from India were rising with 828 reported. By 2012, imported cases from India peaked at 1950 (96.0%). There was a marked decrease in cases imported from India between 2012 and 2018 and then cases imported from Africa and India begin to rise again from 2014, this shifted from 2010 to 2018, as there was a dramatic increase from 23 (2.0%) to 546 (63.0%) cases in 2018 [Figure 3]. Subsequently, there was a dramatic decline to 308 cases in 2018, representing 36% of total imported cases [Figure 3].
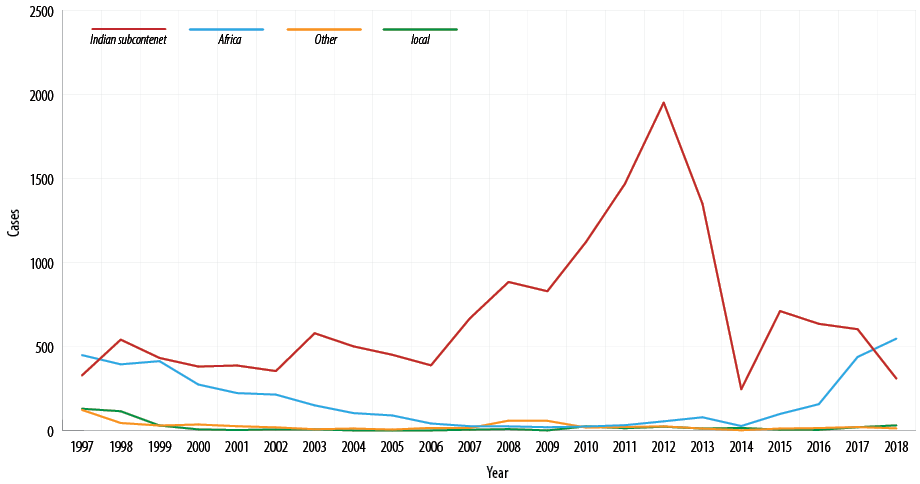 Figure 3: Geographical sources of imported malaria cases in Oman, 1997–2018.
Figure 3: Geographical sources of imported malaria cases in Oman, 1997–2018.
In 1988, P. falciparum was the malaria-predominant species accounting for 91.8% (19 812) of confirmed malaria cases. Cases of P. falciparum declined in subsequent years reaching 4.0% (87) of confirmed cases in 2012 then increased to 86.0% (237) in 2020. Interestingly in 1988, P. vivax represented only 8.0% of confirmed cases; between 1994 and 2012 this rose to 96.0% of all cases in 2012. Subsequently, confirmed P. vivax cases declined from 2013 to 2020, reaching 9% of all malaria notifications in 2020 [Figure 4].
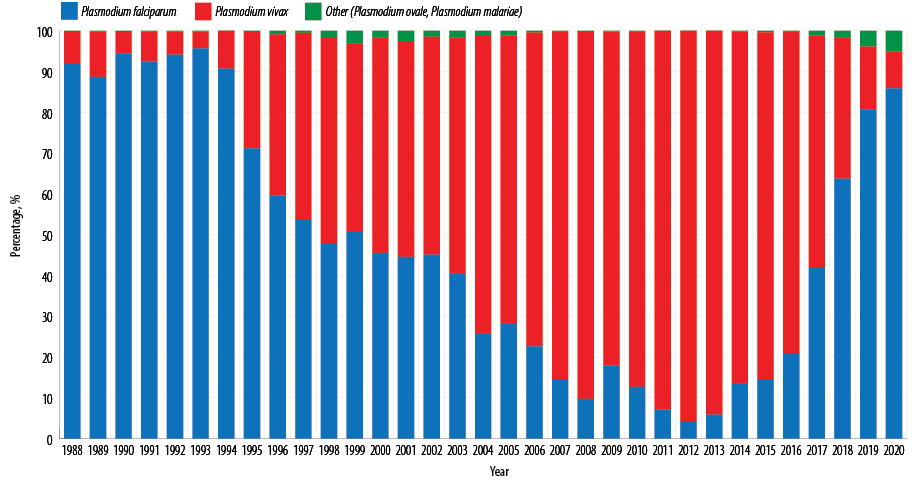 Figure 4: Malaria parasite diagnosis in Oman, 1988–2020.
Figure 4: Malaria parasite diagnosis in Oman, 1988–2020.
Screening for malaria involves both ACD and PCD and in Oman blood slides are collected and then tested from various sources. ACD includes general investigations, contact investigations, airport screening, and medical examinations for non-citizens who apply for a new, or renewal of, their residence card. Passive screening includes reporting and collection of blood slides from public and private healthcare institutions.
Between 1988 and 2020, 9 705 492 blood slides were examined and of these, 6 473 040 (66.7%) were obtained through PCD and 3 232 452 (33.3%) came from ACD. In 1988, the total number of blood slides examined was 252 300. This decreased to 250 020 in 1993 the peaked in 1996 with 527 182 blood slides examined. Since, the number of malaria slides evaluated and the number of positive cases has decreased steadily to 43 284 in 2020, with a 92.0% reduction rate [Figure 5].
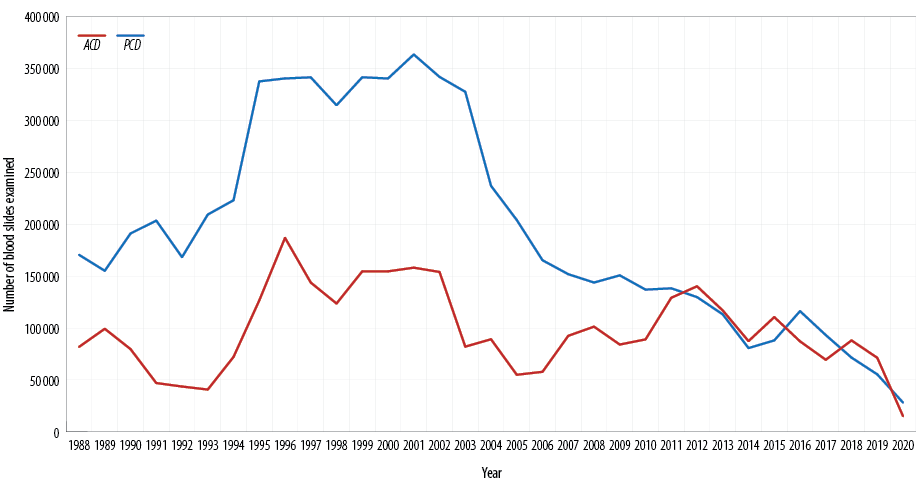 Figure 5: Malaria blood slides examined active case detection (ACD) and passive case
Figure 5: Malaria blood slides examined active case detection (ACD) and passive case
detection (PCD), 1988–2020.
API decreased sharply from 2.188 per 1000 population in 1994 to 0.566 per 1000 population in 1995 and then decreased to zero in 2004. It remained zero for the following two years, then fluctuated in the following years between zero and 0.007 to 0.001 per 1000 population.
The annual blood examination rate increased from 14.6% in 1994 to 23.8% in 1996, decreasing gradually to reach 2.7% in 2019. The positivity rate (SPR) fell from 0.4% to 0.2% between 1995 and 2006. The SPR fluctuated from 2007-2018 reaching an SPR of 1.% in 2019 [Table 1].
Discussion
Oman is a low-incidence country and the number of confirmed malaria cases has steadily declined since 1991.22,23 The malaria mortality rate from indigenous malaria has been zero since 2000 and the last indigenous malaria cases were reported in 2010. With the current decline in annual reporting and mortality, Oman has achieved the WHO goal of malaria elimination defined as the interruption of local transmission of specific malaria parasites within a geographical area resulting from focused malaria elimination and control activities.1
This decrease was primarily attributable to a well-established national malaria eradication program with sufficient resources, human resources trained in the health centers and hospitals, treatment available nationwide, appropriate laboratory capacity, and an extensive surveillance system that includes monitoring, case finding, contact tracing, screening, and program evaluation. The national malaria eradication program is well-funded and has integrated malaria activities with primary, secondary, and tertiary health care services. The malaria notification and registry have been mandated and incorporated into the National Communicable Disease Surveillance System.22 Malaria care, control and prevention services were provided free of charge to everyone regardless of citizenship. In addition, enhanced active case detection particularly among contacts has made a great impact.
The decline in malaria cases in Oman from 1995 is attributed to the efforts and investments in the NMEP. The key programmatic strategies include vector control, mainly larviciding utilizing mapping, screening to support early case detection, and prompt (radical) treatment. Interruption of malaria transmission was achieved in 2004 and maintained till September 2007 when a focus of local transmission was detected in Ad Dakhiliya governorate and then in 2008 transmission occurred in North Al Batinah governorate. In 2009, no local transmission occurred, but due to the high receptivity and increased vulnerability of the country, the increased number of imported cases, local transmission was detected in the following years as it controlled immediately.
In 2013, foci of local transmission were detected in Ad Dakhilya, North Al Batinah, and South A’Sharqiyah governorates.20
The predominant malaria species in 1994 was P. falciparum [Figure 4]. This was attributed to the importation of malaria cases from East Africa. The shift in predominant species to P. vivax occurred due to heavy importation of malaria cases from the Indian subcontinent where much of the labor force was from. However, in 2014 there was an increase in P. falciparum cases due to undocumented immigrants from Somalia in the Dhofar governorate. The number of the undocumented immigrants from Somalia is unknown but it was estimated to be in the hundreds. The sharp increase in the number of malaria blood slides examined from 1994 to 1996 is attributed to the expansion of NMEP to new governorates to cover the entire country [Table 1]. As part of this program, 10% of all fever cases attending outpatient department are required to be screened for malaria. In addition, there is an increase in the number of non-Omanis coming from malaria-endemic countries over the years. However, the reduction in the number of malaria blood slides examined during the period from 2002 to 2010 could be linked to the reduction in the number of imported malaria cases from malaria- endemic countries. To accelerate progress towards elimination, WHO has urged affected countries to maximize the impact of existing life-saving tools and strategies. This strategy is built on three pillars with two supporting elements that guide global efforts towards malaria elimination.1,2 Oman had the lead in the EMR region in implementing many of the substantive components of the three pillars of the WHO’s framework for malaria elimination described below.1,2
Pillar 1: Ensure universal access to malaria prevention, diagnosis, and treatment.
Oman has demonstrated its political commitment through strong governance to ensure universal access to malaria prevention, diagnosis, treatment, and national vector control under the stewardship of the malaria program within the Ministry of Health (MoH). To facilitate this process, a single administrative structure has been established to lead the Malaria Prevention of Re-establishment Strategy at the national and governorate units with focal points across the country with adequate human resources and essential data analysis tools.
Since the beginning of the malaria eradication program in the early 1990s, the ultimate objective was to attain zero vector reproduction around the human population and emphasis has been placed on the examination of maximum breeding sites and the rectification of positive sites. These targets were met in most operating areas and, as a result, malaria transmission was halted, and this status was maintained in subsequent years (two years only). With the decline of malaria cases, larviciding coverage has been cautiously phased out since 1999. However, larviciding continues in malaria-prone areas with larval control and treatment of positive sites continuing today. With the cessation of malaria transmission, entomological malaria surveillance will focus on fine-tuning and maintaining a system capable of mapping malaria susceptibility.
Chemoprevention
Protect all non-immune travelers and migrants. Oman has established a chemoprophylaxis policy used for people at high risk for malaria, including non-immune travelers, who are most likely to die if infected. This policy is also recommended for travelers in malaria-free areas to areas at high risk of malaria. These policies have been implemented to reduce the spread of infection among travelers.
Diagnostic testing and treatment. Oman recognized early case detection, prompt treatment, and proper management of malaria cases through intensified surveillance are of great importance.24 A system has been established to identify vulnerable populations and ensure that health staff are knowledgeable as most cases are likely to present in clinical care settings. Provision of quality diagnostics was made available in all primary healthcare institutions. Since malaria may be a ῾forgotten disease’, raising awareness and motivation among doctors to order a blood smear examination for fever cases is done through a continuous professional development program. To ensure a timely diagnosis and effective treatment, a quality diagnostic service has been established. Microscopy services were strengthened in all areas and an accreditation system was established with international agencies. Vigilance and outbreak response have been the key to prevention of re-establishment.
Monitor safety and efficacy of antimalarial medicines and manage antimalarial drug resistance. Pharmacovigilance and monitoring for antimalarial resistance are routinely monitored through the existing system.
Contain antimalarial drug resistance. The Oman National Malaria Treatment Guidelines were revised based on the recent WHO recommendations.
Pillar 2: Accelerate efforts towards elimination and attained of malaria-free refocus programmes.
In the past, malaria was one of the major public health problems in Oman. Learning from the achievements in the past, Oman refocused on case investigation and epidemiological classification of all cases. Data analysis provided evidence on the source of malaria in Oman (East Africa and the Indian subcontinent) and three key strategies were implemented: 1) distribution of the prophylactic drugs for travelers to malaria endemic countries; 2)screening of arriving passengers from Africa at the airport; 3) involvement of private health institutes in early case detection. Private health institutes are a key strategy in detecting and treating cases coming from the Indian subcontinent.
Interruption of malaria transmission was achieved in 2004 and maintained until September 2007. The program refocused again on increasing preparedness and response to outbreaks through enhanced surveillance and increasing staff competency for malaria diagnostics and case management skills.
Enact legislation. Through previous legislative and public health efforts, malaria management is currently available free of charge to patients. This policy encouraged individuals with suspected malaria to seek medical attention, which assisted in early case detection and prevention of local transmission in the community. This will continue and is reflected in the public health national law currently being prepared for 2022.
Renew political commitment and deepen regional collaboration. Oman has demonstrated its political commitment and the National Malaria Prevention of Re-establishment Strategy agenda has been reaffirmed through national public health legislation. In addition, Oman was collaborating with neighboring countries through the WHO and Gulf Cooperates Council MoH regarding malaria elimination. In addition, one of the strategies used was to provide aid to neighboring countries in the fight against malaria. The National Malaria Laboratory in Oman is considered a center of excellence for the EMR countries and international training programs are conducted there to help countries in the region achieve malaria elimination.
Reduce the number of undetected infections. Oman has adopted the radical treatment of cases with primaquine to prevent the relapse of P. vivax, eliminate gametocytes of P. falciparum, and block the chain of transmission of malaria in the areas at risk, as recommended.
Prevent re-establishment of local malaria transmission. In October 2016, the preliminary draft of the strategy was developed by the Department of Malaria, based on discussions during a regional workshop. Then, extended meetings were conducted with other stakeholders within and outside the MoH.
Malaria notification as part of an e-notification system was established and a standard electronic form was developed for notification of all malaria cases. It is accessible to everyone responsible for the detection, diagnosis, and treatment of malaria.
When a local malaria case has been identified, the concerned departments conduct an epidemiological investigation of both the case and the malaria focus. This investigation includes stratification and identification of high-risk areas and high-risk groups which will guide the different public health activities. The effective use of a geographic information system will help in mapping the receptivity and vulnerability of each area. High-risk groups will be identified and screened through ACD. This is a cost-effective intervention for early case detection and prevention of local transmission.
Use of medicines to reduce the parasite pool. Prompt treatment of all confirmed malaria cases is an important pillar in any malaria program. Physicians are trained annually to meet the program standards in their practice. Malaria was incorporated in the general practitioner’s training program conducted in the governorates. The national malaria management guidelines include primaquine to get rid of gametocytes of P. falciparum, and hypnozoites in the liver to prevent relapses of P. vivax and P. ovale. This is done after conducting tests of the glucose-6-phosphate dehydrogenase status for the patient and prescribing the correct regimen to avoid hemolysis in glucose-6-phosphate dehydrogenase deficient patients.
Detect all infections to attain elimination and prevent re-establishment. After becoming a malaria-free country, many healthcare workers in Oman were less likely to suspect malaria in individuals presenting with fever. This resulted in a delay in diagnosis and treatment of malaria, which if continued would negatively impact both malaria mortality and potential spread of the disease in the community. To prevent this and increase the index of suspicion, and sensitization of healthcare workers to malaria, its diagnosis and management have been and continues to be conducted. In addition, early and mandatory reporting of all confirmed malaria cases identified by public and private healthcare facilities is required.
Devise P. vivax-specific strategies. The use of primaquine to prevent relapse is discussed.
Use surveillance as an intervention in elimination programs. Oman has a well-established surveillance program. Malaria notification is part of the e-notification system established. All malaria cases must be reported within 24 hours. The main objective is to monitor the malaria situation in the country and provide this information to mainstream health services. In addition, this national surveillance system is responsible for monitoring and assessing the effectiveness of preventive action and curative measures taken by general and specialized health services in the country.
Pillar 3: Transform malaria surveillance into a core intervention
Surveillance in areas of high and low transmission. In Oman, malaria surveillance is currently a component of the National Integrated Disease Surveillance system with a stringent notification system.
Surveillance in areas targeted for elimination of malaria. The WHO defines a malaria-free nation as “an area in which there is no ongoing local mosquito-borne malaria transmission, and the risk of contracting malaria is restricted to infection from introduced cases” and in the status of prevention of re-establishment of malaria.23,24 According to this criterion, Oman is a malaria-free country. A strong and vigilant surveillance system must be maintained to sustain the malaria-free status.
Invest in routine information systems. Malaria surveillance is currently a key component of the national integrated disease surveillance system. Investments in training, the reporting system, and quality assurance continue to be made.
Collect necessary data for understanding disease trends and overall program performance. The surveillance is undergoing regular monitoring internally and externally. National reports and governorate reports are provided for program review and modification.
Develop national strategic plans that consider the epidemiology and heterogeneity of malaria in a country. The National Strategic Plans for Prevention of Re-establishment of Local Malaria Transmission in Malaria-Free countries was adopted in 2016 with modifications as new policies and the epidemiological situation demand.
Monitor the implementation of the national malaria strategic plan at regular intervals. The National Strategy for Prevention of Re-establishment of Malaria Transmission strategic plans are regularly monitored.
Ensure the surveillance system is monitored. The national and subnational surveillance system is continuously monitored regularly through the quality assurance system. This includes monitoring the diagnosis through crosschecking blood smears at different levels (regional and national) and revising the data collected from the electronic surveillance system when required.
Challenges and the way forward
The foremost challenges encountered in the malaria elimination initiative in Oman is to ensure a critical review of both the progress and challenges, focusing on key issues that may support programmatic improvements and prevent the achievement of the 2030 elimination targets. Key actions include the maintenance of trained personnel for the malaria program at all levels, securing government, and other program funding to maintain the vigilance of malaria surveillance and continued high-quality vector surveillance.
Limitations
Additional data is required that reflects the actual clinical practice. For example, were the patients that were malaria positive on given chemoprophylaxis? Were they given the correct chemoprophylaxis? We are limited in our ability to monitor the rate of policy implementation. It is no longer acceptable to state there is a policy. We need to start to think of “knowledge translation and evidence-informed decision making in the development of policies”.
Conclusion
After a lengthy history of malaria control, Oman achieved malaria elimination status. Thanks to an updated elimination program, technically skilled employees, and a good deal of hard work. It is vital to maintain this status since the country is still extremely susceptible to malaria. To keep the malaria-free status, a national plan to maintain the disease’s elimination status and prevent re-emergence must be implemented. Plans should also be underway for documentation and certification of malaria elimination.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
Acknowledgments
We are highly in debt to H.E. Ali Bin Moosa, H.E. Ahmed Al Saidi, late Ali Jaffer Mohammed, Abdallah Al Mandhari, Salim Al Wahaibi, late Ahmed Al Ghassani, Mohammed Al Hosani, Majed S. Al Zadjali, Governorate Malaria focal points and for their guidance and support.
references
- 1. World Health Organization. World malaria report 2021. [cited 2022 January 6]. Available from: https://www.who.int/publications/i/item/9789240040496.
- 2. World Health Organization. Global technical strategy on malaria 2016-2030. [cited 2021 August 1]. Available from: https://www.who.int/publications/i/item/9789240031357.
- 3. World Health Organization. World malaria report 2020: 20 years of global progress and challenges. 2020 [cited 2021 August 1]. Available from: https://www.who.int/publications/i/item/9789240015791.
- 4. World Health Organization. Zeroing in on malaria elimination. [cited 2021 August 6]. Available from: https://www.who.int/publications/i/item/9789240024359.
- 5. World Health Organization. Regional malaria action plan 2016–2020 towards a malaria-free region. [cited 2021August 2]. Available from: https://applications.emro.who.int/docs/EMROPUB_2017_EN_19546.pdf.
- 6. Gill CA. Malaria in Muscat. Indian J Med Res 1916;4(1).
- 7. Mashaal HAH. A story of success: eradication of malaria from Oman 1991–2006. World Health Organization, Eastern Mediterranean Regional Office archive; Cairo. 2006.
- 8. Shidrawi GR. Report on a visit to the Sultanate of Oman, 28 April–16 May 1982. World Health Organization; 1982. Eastern Mediterranean Regional Office report; EM/MAL/193. [cited 2021 August 2]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3951717/.
- 9. Matta SE. Assignment report: malaria control programme, Oman, January 1975–December 1984. World Health Organization; Cairo: 1984. (Eastern Mediterranean Regional Office archive). [cited 2021 August 2]. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3951717/.
- 10. Snow RW, Amratia P, Zamani G, Mundia CW, Noor AM, Memish ZA, et al. The malaria transition on the Arabian Peninsula: progress toward a malaria-free region between 1960–2010. Advances in Parasitology 2013;82:205-251.
- 11. Zahar AR, Delfini LF, Ruebush RK. Report on assessment on the malaria control programme Sultanate of Oman. World Health Organization; Cairo: 1982. (Eastern Mediterranean Regional Office archive). [cited 2021 August 2]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3951717/.
- 11. Parves SD. Anophelines of Sultanate of Oman. Unpublished report; 1995.
- 12. Simon B, Sow F, Al Mukhaini SK, Al-Abri S, Ali OA, Bonnot G, et al. An outbreak of locally acquired Plasmodium vivax malaria among migrant workers in Oman. Parasite 2017;24.
- 13. Baomar A, Mohamed A. Malaria outbreak in a malaria-free region in Oman 1998: unknown impact of civil war in Africa. Public Health 2000 Nov;114(6):480-483.
- 14. Ganguly SS, Al-Shafaee MA, Al-Lawati JA, Dutta PK, Duttagupta KK. Epidemiological transition of some diseases in Oman: a situational analysis. East Mediterr Health J 2009 Jan-Feb;15(1):209-218.
- 15. Booij P, Holoubek I, Klánová J, Kohoutek J, Dvorská A, Magulová K, et al. Current implications of past DDT indoor spraying in Oman. Sci Total Environ 2016 Apr;550:231-240.
- 16. Ullah MM, Yar A, Al Balushi MD, Al Aliyani NR, Kalarikkal B, Miranda RI, et al. Directorate of disease surveillance and control, directorate general of health services, Al Buraimi Governorate, Ministry of Health, Sultanate of Oman. Infect Dis Rep 2020;12(8304):8304.
- 17. Jairajpuri ZS, Rana S, Hassan MJ, Nabi F, Jetley S. An analysis of hematological parameters as a diagnostic test for malaria in patients with acute febrile illness: an institutional experience. Oman Med J 2014 Jan;29(1):12-17.
- 18. Al Awaidy ST, Faraj M. Infectious diseases in Oman: a review and progress towards elimination and eradication. Indian J App Res 2017;7:555-557.
- 19. Ministry of Information. Statistical yearbook 2020: issue 48 [cited 2021 June 24]. Available from: https://www.ncsi.gov.om/Elibrary/Pages/LibraryContentDetails.aspx?ItemID=/fm/apwu0drCXa/PQ1fExQ%3D%3D7.
- 20. Ministry of Health. Annual health report 2020. 2020 [cited 2021 July 20]. Available from: https://www.moh.gov.om/en/web/statistics/-/-2019.
- 21. Atta H, Zamani G. The progress of roll back malaria in the Eastern Mediterranean Region over the past decade. East Mediterr Health J 2008;14(Suppl):S82-S89.
- 22. World Health Organization. A framework for malaria elimination. 2017 [cited 2022 March 7]. Available from: https://www.ncsi.gov.om/Elibrary/Pages/LibraryContentDetails.aspx?ItemID=/fm/apwu0drCXa/PQ1fExQ%3D%3D.
- 23. Ministry of Health. Manual on communicable diseases. 2017 [cited 2021 August 23]. Available from: https://www.moh.gov.om/documents/236878/0/communicable+diseases+Manual/a0577e5e-cc5a-4cb6-a460-832e37b6b587.