Down syndrome (DS), also known as trisomy 21, is the most common chromosomal abnormality found in humans. These patients manifest anatomical abnormalities in the respiratory tract such as a smaller trachea, enlarged adenoids and tonsils, macroglossia, narrow upper airway, tracheobronchial malacia, and hypotonia of upper airway, predisposing them to aspiration and glossoptosis. A review by Watts et al,1 on children with DS revealed that lower respiratory tract infections (LRTIs) were responsible for 43–78% of their hospitalizations, with at least 50% requiring ventilatory support. Patients with DS have several issues like anatomical aberrations in the upper respiratory tract and underlying immune dysregulation. They also tend to resist non-invasive ventilation (NIV) as many are mentally challenged with intellectual disability, attention problems, cognitive dysfunction, and proneness to tantrums. Therefore, when they develop serious respiratory illnesses such as COVID-19, they have a stormy course and sometimes unfavorable outcomes. Based on their clinical presentation, DS patients with COVID-19 should be offered invasive ventilation and monitored closely.
We report our experience of three DS patients who were admitted to our intensive care unit (ICU) with COVID-19 infection confirmed by positive reverse transcriptase polymerase chain reaction from nasopharyngeal swabs.
Case Report
Case one
A 37-year-old female, with DS, was admitted to the COVID-19 ICU with tachypnoea (respiratory rate of 35/min), oxygen saturation (SpO2) of 88%, and with bilateral infiltrates on chest radiograph [Figure 1]. NIV was initiated on arrival with the following settings: pressure support (PS) of 15 cm of water, positive end-expiratory pressure (PEEP) of 10 cm of water, and a fraction of inspired oxygen (FiO2) of 0.6. After six days of NIV, she improved clinically and radiologically with an acceptable partial pressure of oxygen (PaO2)/FiO2 (P/F) ratio. She was discharged from the hospital on day 13 of admission.
 Figure 1: Chest radiograph in anteroposterior view of patient one with bilateral infiltrates suggestive of COVID-19 pneumonia.
Figure 1: Chest radiograph in anteroposterior view of patient one with bilateral infiltrates suggestive of COVID-19 pneumonia.
Case two
A 32-year-old female, with DS, was admitted with tachypnea and desaturation (SpO2: 85%). NIV was initiated (PS:12 cm of water, PEEP: 12 cm of water, FiO2: 0.7). Her oxygen requirement kept increasing (P/F ratio consistently < 100 for two days) and had no improvement in the chest radiograph [Figure 2]. After four days of NIV, she was intubated and ventilated. Prone ventilation was instituted as per international guidelines and neuromuscular blockade was resorted to while the patient remained in a prone position.2 Fentanyl and midazolam infusions were used for sedo-analgesia. She was extubated after five days of mechanical ventilation and discharged on day 21.
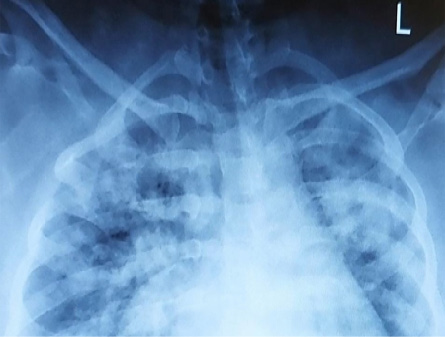 Figure 2: Chest radiograph in anteroposterior view of patient two with bilateral infiltrates suggestive of COVID-19 pneumonia.
Figure 2: Chest radiograph in anteroposterior view of patient two with bilateral infiltrates suggestive of COVID-19 pneumonia.
Case three
A 24-year-old male with DS was admitted to COVID-19 ICU and initiated on NIV (PS: 8 cm of water, PEEP: 10 cm of water, FiO2: 1) in view of tachypnoea and desaturation (SpO2: 87%). Chest radiograph showed bilateral infiltrates consistent with COVID-19 pneumonia [Figure 3]. Although respiratory distress settled with the above ventilatory settings, P/F ratio remained low for two days (the lowest being 61). Invasive ventilation was started and prone ventilation was initiated as was done for patient two. In view of leukocytosis and the presence of multi-drug resistant bacteria in tracheal secretion culture, broad-spectrum intravenous antibiotics were started based on the sensitivity report. Serial chest radiographs and arterial blood gas analysis showed consistent improvement. The trachea was extubated after nine days of mechanical ventilation and thereafter managed with NIV for another two days followed by oxygen therapy. The patient was discharged from the hospital on day 19.
 Figure 3: Chest radiograph in anteroposterior view of patient three with bilateral infiltrates suggestive of COVID-19 pneumonia.
Figure 3: Chest radiograph in anteroposterior view of patient three with bilateral infiltrates suggestive of COVID-19 pneumonia.
Demography details, duration of ventilation, adverse events, inflammatory markers, relevant investigations, medications used, and duration of hospital stay have been summarized in Tables 1 and 2.
Table 1: Demographic data, relevant investigations, and inflammatory markers.
|
|
|
Arrival
|
Highest
|
Arrival
|
Highest
|
Arrival
|
Lowest
|
Arrival
|
Highest
|
Arrival
|
Highest
|
Arrival
|
Highest
|
Arrival
|
Highest
|
|
1
|
37, F
|
69
|
6.92
|
16.07
|
4.79
|
9.80
|
1.65
|
1.65
|
51.4
|
51.4
|
1458
|
1629
|
0.46
|
0.46
|
471
|
471
|
|
2
|
32, F
|
80
|
9.95
|
29.39
|
8.41
|
25.36
|
1.00
|
0.70
|
18.8
|
109.0
|
-
|
-
|
0.45
|
1.20
|
344
|
488
|
WBC: White blood cells, CRP: C-reactive protein, LDH: lactate dehydrogenase.
All three patients had hypothyroidism as an associated problem.
Table 2: Details of ventilatory support, oxygenation, duration of hospital stay, and supportive treatment.
|
1
|
NIV
|
6
|
Not applicable
|
None
|
Day 13
|
120
|
10
|
Convalescent plasma, dexamethasone,
broad-spectrum antibiotics, favipiravir, and LMWH
|
|
2
|
NIV and IV
|
NIV: 4+3
IV: 5
|
After 5 days
|
None
|
Day 21
|
90
|
14
|
Tocilizumab,
Dexamethasone,
broad-spectrum antibiotics,
favipiravir, and
LMWH
|
IV: invasive ventilation; NIV: non-invasive ventilation; P/F: PaO2/FiO2; PEEP: positive end-expiratory pressure; LMWH: low molecular weight heparin.
Discussion
Intellectual impairment, disorders of the cardiovascular system, dependency on family members, and immune dysregulation are the associated factors that further predispose DS patients to adverse pulmonary complications. The proposed mechanism of immune dysregulation is that several genes encoded in chromosome 21 are over-expressed in patients with DS. Hence, these patients have increased levels of circulating cytokines such as tumor necrosis factor-α, interleukin-β, and interleukin-λ, along with an altered cell-mediated immunity. Therefore, DS patients tend to have exaggerated inflammatory responses and infectious diseases tend to be more severe in them. Additionally, DS patients can be expected to have especially stormy courses of COVID-19 due to the following factors. These comprise abnormalities of upper airway predisposing them to frequent respiratory tract infections in addition to intellectual disabilities.3 Underlying pulmonary hypertension, obstructive sleep apnea, and chronic lung disease resulting from chronic respiratory tract infections also make the disease process tempestuous for these patients. DS patients are also more susceptible to secondary bacterial infections due to the likelihood of underlying chronic lung disease.4
Patients with DS find it exceedingly difficult to cooperate with treatments such as NIV due to characteristics like intellectual disability, attention problems, cognitive dysfunction, and proneness to tantrums. Due to these multiple issues, previous papers have shown that these patients have worse outcomes.5 In Oman, the birth prevalence of DS is 2.4 in 1000 which translates to about 120 affected births/year.6
In a retrospective study, Pérez-Padilla et al,7 presented their data derived from a Mexican national database of 60 DS patients who were hospitalized during the H1N1 pandemic of 2009. They concluded that patients with DS had a higher propensity for hospitalization, endotracheal intubation, and death due to pulmonary complications. Even after being successfully weaned off mechanical ventilation, it was found difficult to expect assisted respiratory exercises like incentive spirometry from these patients. They recommended that DS patients should be protected against seasonal influenza viruses by vaccination.7 Vita et al,8 have also suggested early vaccination in this high-risk category of patients for the same reasons.
In a recent international online survey, Hüls et al,9 identified 1046 patients with DS from a total of 59 025 hospitalized patients and the mortality rate was 13% in DS patients. The authors suggested that patients with DS should be considered a priority group for COVID-19 vaccination. The mortality in hospitalized DS patients is higher than the mortality in the general population of patients admitted due to COVID-19 infection.10 Considering these realities, we recommend that all DS patients in Oman should be considered a priority group for vaccinations.
Conclusion
Patients with DS with COVID-19 disease and presenting with hypoxic respiratory failure should be closely monitored clinically. Managing NIV is challenging in these patients due to underlying intellectual problems and their dependency on family members. Where managing with NIV is difficult, early invasive ventilation should be considered, especially if a clinical course is expected to worsen based on inflammatory markers, chest radiograph, P/F ratio, and clinical signs. DS patients should be given top priority in immunization programs against respiratory infections including COVID-19.
Disclosure
The authors declared no conflicts of interest. Written consent was obtained from the patient and family members.
references
- 1. Watts R, Vyas H. An overview of respiratory problems in children with Down’s syndrome. Arch Dis Child 2013 Oct;98(10):812-817.
- 2. Guérin C, Albert RK, Beitler J, Gattinoni L, Jaber S, Marini JJ, et al. Prone position in ARDS patients: why, when, how and for whom. Intensive Care Med 2020 Dec;46(12):2385-2396.
- 3. Espinosa JM. Down syndrome and COVID-19: a perfect storm? Cell Rep Med 2020 May;1(2):100019.
- 4. Sullivan KD, Evans D, Pandey A, Hraha TH, Smith KP, Markham N, et al. Trisomy 21 causes changes in the circulating proteome indicative of chronic autoinflammation. Sci Rep 2017 Nov;7(1):14818.
- 5. Emami A, Javanmardi F, Akbari A, Asadi-Pooya AA. COVID-19 in patients with Down syndrome. Neurol Sci 2021 May;42(5):1649-1652.
- 6. Ministry of Health. Guideline for medical management of children and young people with Down syndrome. 2015 [cited 2021 July 6]. Available from: https://www.moh.gov.om/documents/272928/3240138/Guideline+for+Management+of+Down+Syndrome.pdf/cdc238c4-92da-78f1-9dd9-50abbee03779.
- 7. Pérez-Padilla R, Fernández R, García-Sancho C, Franco-Marina F, Aburto O, López-Gatell H, et al. Pandemic (H1N1) 2009 virus and Down syndrome patients. Emerg Infect Dis 2010 Aug;16(8):1312-1314.
- 8. Vita S, Di Bari V, Corpolongo A, Goletti D, Espinosa J, Petracca S, et al; INMI COVID-19 study groups. Down syndrome patients with COVID-19 pneumonia: a high-risk category for unfavourable outcome. Int J Infect Dis 2021 Feb;103:607-610.
- 9. Hüls A, Costa AC, Dierssen M, Baksh RA, Bargagna S, Baumer NT, et al; T21RS COVID-19 Initiative. Medical vulnerability of individuals with Down syndrome to severe COVID-19-data from the Trisomy 21 Research Society and the UK ISARIC4C survey. EClinicalMedicine 2021 Mar;33:100769.
- 10. Chang PC, Yang CC, Kao KC, Wen MS. Clinical outcomes of patients hospitalized for COVID-19 versus SARS: a meta-analysis. Aging (Albany NY) 2020 Nov;12(24):24552-24569.