Neck masses are common in clinical practice and affect all age groups. It can be acute or chronic, benign or malignant, and congenital or acquired. Branchial cysts are commonly unilateral slow-growing swellings on the lateral neck resulting from persisting branchial apparatus, most common being second branchial arch anomalies.1,2 They are the second commonest congenital head and neck lesions after thyroglossal duct cysts, and are clinically apparent in late childhood or early adulthood, with higher incidence rates in males than females.3-5 We report a rare case of bilateral branchial cysts in a young woman.
Case Report
A 23-year-old woman presented with bilateral painless neck swelling for one year which was gradually enlarging. There was no history of pain, fever, skin changes, discharge, or swelling elsewhere in the body. Aside from the swelling, there was no significant ear, nose, and throat symptom. She denied any B symptoms, hyper- or hypothyroid symptoms, or contact with a tuberculosis patient. There was no similar problem or malignancy in the family. The patient denied a personal or family history of renal anomalies or hearing loss. She was also a non-smoker and teetotaler.
Upon neck examination, there were bilateral soft cystic masses at level II anterior to sterno-cleidomastoid muscle (SCM). Left-sided mass measured 4 × 6 cm. The right-sided mass was smaller at 2 × 3 cm. Both swellings had well-defined margins, smooth surfaces, and were non-tender with normal overlying skin [Figure 1]. Other ear, nose, and throat findings including those of nasopharyngolaryngoscopy were unremarkable.
 Figure 1: Bilateral soft cystic neck swelling at level II-III, well-defined and anterior to the sternocleidomastoid muscle.
Figure 1: Bilateral soft cystic neck swelling at level II-III, well-defined and anterior to the sternocleidomastoid muscle.
Fine needle aspiration cytology showed a hypocellular smear with foamy macrophages, cholesterol crystals, inflammatory cells, and proteinaceous fluid. No epithelial, atypical, or malignant cells were seen. These findings were consistent with those of a cyst. Tuberculosis workups were negative. Neck ultrasonography (USG) revealed bilateral well-defined hypoechoic masses with echogenic debris within. Neck computed tomography (CT) scan showed two well-defined cystic lesions (3.3 × 2.7 × 4.8 cm on the right; 4.0 × 2.2 × 6.8 cm on the left) with no extension seen medial to SMC or lateral to carotid space [Figure 2]. This confirmed the ultrasound findings and ruled out malignancy. USG and CT findings were highly suggestive of bilateral type II branchial cleft cysts. In addition, abdominal and renal USG revealed normal findings, thus excluding the possibility of branchiootorenal syndrome.
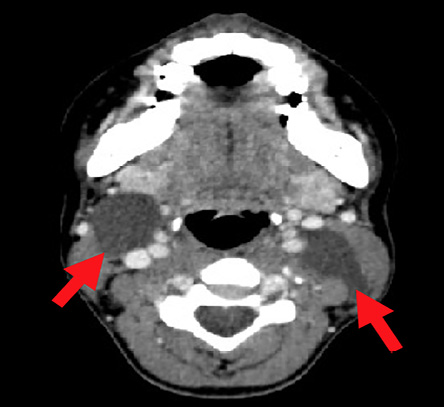 Figure 2: CT scan (axial view) showing bilateral neck swelling. The right swelling is anterior to sternocleidomastoid muscle (SCM) and the left swelling is deep to SCM (arrows).
Figure 2: CT scan (axial view) showing bilateral neck swelling. The right swelling is anterior to sternocleidomastoid muscle (SCM) and the left swelling is deep to SCM (arrows).
Complete bilateral surgical excision of both branchial cysts was performed, one at a time. On each side, a skin crease transverse incision was made at lateral upper one-third of the neck. Subplatysmal flap was raised and SCM retracted laterally to expose the lesion. The right lesion extended superiorly to the right posterior belly of digastric muscle, laterally to lateral border of SCM, medially to laryngeal framework, and inferiorly to the level of thyroid cartilage. The cyst was sitting on the right internal jugular vein, but not attached to it [Figure 3]. The left lesion extended superiorly to posterior belly of digastric muscle, 1 cm laterally to the lateral border of SCM, medially to the carotid space, and inferiorly to left inferior belly of omohyoid muscle. The left lesion, which was excised first, presented with considerable difficulties, being much larger than the other and located posterior to SCM. It was also posterior to the left carotid artery and extremely close to it. Despite these difficulties, we managed to dissect it out without vascular injury or other complications. The excised right and left lesions measured 3 × 4 cm [Figure 4] and 7 × 4 cm, respectively. Both contained straw-colored fluid upon aspiration. There was no sinus extension to the pharynx. Bilateral drains were inserted and removed on the third day of excision. Postoperatively, the patient recovered well. Histopathology showed a cyst lined by squamous epithelial cells with stroma, containing numerous lymphoid tissues, and establishing our initial diagnosis.
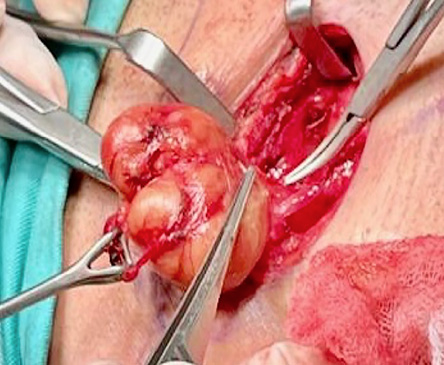 Figure 3: Intraoperative view of the right branchial cyst, which measured 3 × 4 cm after excision. Note the yellowish encapsulated lesion.
Figure 3: Intraoperative view of the right branchial cyst, which measured 3 × 4 cm after excision. Note the yellowish encapsulated lesion.
 Figure 4: The specimen of right branchial cyst measuring 3 × 4 cm.
Figure 4: The specimen of right branchial cyst measuring 3 × 4 cm.
Discussion
Differential diagnosis of chronic neck masses should take into account the patient’s age group and the character of the swelling. The diagnostic possibilities include thyroid pathology, branchial cysts, laryngocele, thyroglossal duct cysts, and dermoid cysts.6 Branchial cleft cysts, as in the present case, are congenital anomalies. Even for young patients, the possibility of malignancies such as lymphoma, papillary thyroid carcinoma, and secondary metastasis should be considered. A recent retrospective study of 28 cases revealed 10.7% malignancy.7 For malignant cases, it is important to consider metastatic cystic squamous cell carcinoma to a lymph node from an oropharyngeal human papillomavirus-associated squamous cell carcinoma, found in 3% of the cases.8,9
Branchial cysts commonly present as a single, painless mass in the neck of a child or young adult, usually on the left side, less frequently on the right. Only 2–3% of presentations are bilateral; multiple ones are rare.1,2 Although congenital, branchial cysts are slow-growing lesions, taking years to develop and manifest with variable sizes and locations. Second (type II) branchial cysts are categorized into four sub-types based on their anatomical positions.10 Our patient had a type II branchial cyst which lay anterior to the SCM, and adjacent and lateral to the carotid sheath.10
Bilateral lesions may have a familial association with autosomal dominant inheritance.11 Branchiootorenal syndrome is characterized by branchiogenic anomalies, hearing loss, and congenital anomalies of the kidney and urinary tract.12 It is confirmed with genetic tests.13 Our patient neither had familial history of the syndrome nor its symptoms.
The bilateral branchial cysts may also present with local compressive symptoms such as dysphagia, dysphonia, dyspnea, and stridor.14 The cysts may become infected and painful following an upper respiratory tract infection, suppuration, fistula formation, or discharging sinus.15 Infected branchial cysts may also develop into potentially life-threatening retropharyngeal abscess.16
The diagnosis of branchial cysts may seem straightforward with high diagnostic accuracy, as demonstrated by previous case series.4,17 On the contrary, in a case series by Zaifullah et al,2 correct clinical diagnosis was made only in five of 12 (41.6%) cases, mainly due to misdiagnoses as neck abscess, neoplastic lymphadenopathy, cold abscess, neoplasms, or thyroid pathology. Poor diagnostic accuracy was also reported by another study where only 41.2% (14 of 34) of cases were correctly diagnosed on presentation.18
Fine needle aspiration cytology is recommended prior to surgical intervention as it is diagnostic and therapeutic, as it can relieve the symptoms and temporarily shrink the cyst. Cytology typically demonstrates benign epithelial cells with cholesterol crystals and lymphoid aggregates.18 Our case showed a cyst lined by squamous epithelial cells with stroma containing cholesterol crystals and numerous lymphoid tissues, confirming the diagnosis of the branchial cyst.
In the primary health care setting, USG may be used for initial imaging to differentiate cystic from solid lesions, measure size, and differentiate high-flow from low-flow vascular malformations. It is non-invasive, rapid, and low-cost with non-ionizing radiation, although the extent of the lesion may not be determined accurately.6 CT or magnetic resonance imaging scan is needed where the cyst is extensive or in an unusual site in order to delineate its extension and anatomical relation to adjacent structures before definitive surgical excision.1
Surgical excision is best performed in non-infected neck to minimize risks of bleeding and postoperative infection.3. It is possible to completely excise both sides of a bilateral lesion in a single carefully planned surgical session, as in the present case. Complete excision with no prior surgery has a low recurrence rate of 3–4%, while re-excision of branchial cysts following previous improper surgery has a high recurrence rate of up to 20%.18 Recurrent cases may be complicated by fibrosis from previous surgery which further increases the likelihood of incomplete excision.19
There is also a risk of malignant transformation of the branchial cyst; primary branchiogenic carcinoma. Even though it is extremely rare, it must be excluded prior to surgical intervention as it entails a different course of treatment.20 Al-Mufarrej et al,14 found malignant degeneration in four of 421 (1%) cases in older patients (> 45 years) with branchial anomalies.
Conclusion
Branchial cysts are congenital neck lesions commonly presented as unilateral neck swelling during early adulthood. We reported a rare case of bilateral branchial cysts in a young woman which was successfully diagnosed and excised. Meticulous clinical examinations and investigations are crucial before embarking on any surgical treatment. Numerous differential diagnoses are possible and will depend on the patient’s age, the location of the mass, the detailed characterization of the mass as well as the associated symptoms. The presence of bilateral branchial cysts should raise suspicion of a larger clinical syndrome which should be probed further, which includes meticulous personal and family history. Primary health care practitioners play an important role in detecting the possibility of branchial anomalies and arranging for referral to secondary care.
Disclosure
The authors declared no conflicts of interest. Informed written consent was taken from the patient.
Acknowledgments
We thank the Director General of Health Malaysia for his permission to publish this article vide Ref. NIH.800-4/4/1 Jld. 99(42).
references
- 1. Chandramani BM, Palak S, Rao N. Branchial cleft cyst- A rare presentation and review of literature. Int J Curr Res 2016 Dec;8(12):43789-43792.
- 2. Zaifullah S, Yunus MR, See GB. Diagnosis and treatment of branchial cleft anomalies in UKMMC: a 10-year retrospective study. Eur Arch Otorhinolaryngol 2013 Mar;270(4):1501-1506.
- 3. Anoop AR. Akhtar W, Yadav Y. A clinical study of second branchial cleft anomalies: our experience in a teaching hospital in Northern India. J Head Neck Physicians Surg 2020 Dec;8(2):96.
- 4. Li W, Xu H, Zhao L, Li X. Branchial anomalies in children: a report of 105 surgical cases. Int J Pediatr Otorhinolaryngol 2018 Jan;104:14-18.
- 5. Chavan S, Deshmukh R, Karande P, Ingale Y. Branchial cleft cyst: a case report and review of literature. J Oral Maxillofac Pathol 2014 Jan;18(1):150.
- 6. Haynes J, Arnold KR, Aguirre-Oskins C, Chandra S. Evaluation of neck masses in adults. Am Fam Physician 2015 May;91(10):698-706.
- 7. Yehuda M, Schechter ME, Abu-Ghanem N, Golan G, Horowitz G, Fliss DM, et al. The incidence of malignancy in clinically benign cystic lesions of the lateral neck: our experience and proposed diagnostic algorithm. Eur Arch Otorhinolaryngol 2018 Mar;275(3):767-773.
- 8. Muller S, Aiken A, Magliocca K, Chen AY. Second branchial cleft cyst. Head Neck Pathol 2015 Sep;9(3):379-383.
- 9. Pietarinen-Runtti P, Apajalahti S, Robinson S, Passador-Santos F, Leivo I, Mäkitie AA. Cystic neck lesions: clinical, radiological and differential diagnostic considerations. Acta Otolaryngol 2010 Feb;130(2):300-304.
- 10. Arshad M, Ashafaq U, Aslam M. Branchial cleft cyst; second branchial cleft cyst and sinus, diagnosis and management. Prof Med J 2019 Mar;26(3):523-527.
- 11. Mailleux P, Lismonde Y. Adult presentation of a complete second branchial cleft fistula diagnosed by US and CT, autosomal dominant transmission in three members of the family: case report. Open J of Medical Imaging 2020 Apr;10(2):125-131 .
- 12. Unzaki A, Morisada N, Nozu K, Ye MJ, Ito S, Matsunaga T, et al. Clinically diverse phenotypes and genotypes of patients with branchio-oto-renal syndrome. J Hum Genet 2018 May;63(5):647-656.
- 13. Morisada N, Nozu K, Iijima K. Branchio-oto-renal syndrome: comprehensive review based on nationwide surveillance in Japan. Pediatr Int 2014 Jun;56(3):309-314.
- 14. Al-Mufarrej F, Stoddard D, Bite U. Branchial arch anomalies: Recurrence, malignant degeneration and operative complications. Int J Pediatr Otorhinolaryngol 2017 Jun;97:24-29.
- 15. Valentino M, Quiligotti C, Carone L. Branchial cleft cyst. J Ultrasound 2013 Mar;16(1):17-20.
- 16. Huang RY, Damrose EJ, Alavi S, Maceri DR, Shapiro NL. Third branchial cleft anomaly presenting as a retropharyngeal abscess. Int J Pediatr Otorhinolaryngol 2000 Aug;54(2-3):167-172.
- 17. Kalra VK, Rattan KN, Yadav SP, Bhukar S, Dheeraj S. Second branchial anomalies: a study of 94 cases. Indian J Otolaryngol Head Neck Surg 2017 Dec;69(4):540-543.
- 18. Daoud FS. Branchial cyst: an often forgotten diagnosis. Asian J Surg 2005 Jul;28(3):174-178.
- 19. Mehmi N, Kumar R, Sagar P, Singh CA, Kumar R, Thakar A, et al. Importance and impact of appropriate radiology in the management of branchial cleft anomalies. Indian J Otolaryngol Head Neck Surg 2019 Oct;71(Suppl 1):953-959.
- 20. Colella G, Boschetti CE, Spuntarelli C, De Cicco D, Cozzolino I, Montella M, et al. Primary branchiogenic carcinoma: malignant degeneration of a branchial cyst, a case report. Cancer Rep (Hoboken) 2021 Apr;4(2):e1315.