The heart is considered the ultimate icon of love and compassion. It is also peculiar in having an almost immunity to cancer. A search on Google or PubMed for cardiac lesions, will yield very few results and are littered with individual case reports and some review articles. There are not many original articles, case series, or clinical trials available on these rare but significant lesions.
Despite the existence of cardiac lesions being known to mankind since the Middle Ages, they continue to remain a diagnostic puzzle and therapeutic challenge to physicians worldwide. The first successful resection of a cardiac tumor was performed by Crawford in 1954.1
Cardiac tumors may be primary (benign or malignant) or metastatic (malignant). Metastatic tumors of the heart are 30 times more common. Only 25% of primary cardiac tumors are malignant and, of these, 75% are sarcomas.2 Primary tumors to the heart are extremely rare and are seldom encountered in clinical practice. However, in the current era of sophisticated diagnostic imaging, their prevalence is increasing. The overall prevalence of primary cardiac tumors is between 0.17% and 0.19%. Different autopsy series estimate their incidence to be anywhere from 0.001% to 0.19%.3,4
Cardiac lesions are usually asymptomatic and are detected only incidentally. Symptoms, if present, are varied and depend on the location of the area involved. Presentation features include congestive heart failure from intracardiac obstruction, systemic embolization, constitutional symptoms, and arrhythmias.
Cardiac tumors vary in size and shape. Their size and location within the heart determines the clinical presentation of the patient and line of treatment. In adults, somewhat mushy, gelatinous type of tumor called myxoma is the most common; in infants and children, rhabdomyomas predominate.
Primary cardiac lesions pose as a diagnostic and therapeutic challenge because of their rarity. Thus, the aim of our study is to highlight the clinical picture, line of diagnosis, and treatment guidelines of five such primary cardiac lesion cases that presented to our institute.
Case reports
Case one: cardiac lipoma
A 60-year-old male patient presented to the emergency department with chest pain associated with dizziness for the last 15 days. The pain radiated to the left arm and left side of his neck. On review of his symptoms, the patient mentioned that he was also experiencing shortness of breath preceded by palpitations for more than one month. His medical history included hypertension and he was on regular medication. All his laboratory findings and blood work were within normal limits. His physical examination was unremarkable. Electrocardiogram was done which was within normal limits. However, an echocardiogram revealed a large, heterogeneous, mobile mass, in the right atrium attached to the lateral border measuring 55 × 45 mm and involving the inter-atrial septum [Figure 1]. Computed tomography (CT) scan and magnetic resonance imaging (MRI) were done, and a provisional diagnosis of right atrial myxoma was made. A cardiothoracic surgery (CVTS) consultation was also done. Given the patient’s significant symptoms and the large size of the mass, surgical resection was planned. A well circumscribed, right atrial mass of 55 × 45 mm was removed. It was found to be involving the right lateral border, right inter-atrial septum, and right atrial wall. The specimen was sent to the histopathology department for routine examination. On receiving the specimen, the external surface was well encapsulated, glistening, and the cut surface was smooth and yellowish. Multiple paraffin-embedded and hematoxylin and eosin (H&E)-stained sections were examined under the microscope, which revealed a well-circumscribed mass lesion comprised of mature adipocytes in sheets and surrounded by fibrous bands [Figure 2]. A final diagnosis of right atrial lipoma was made.
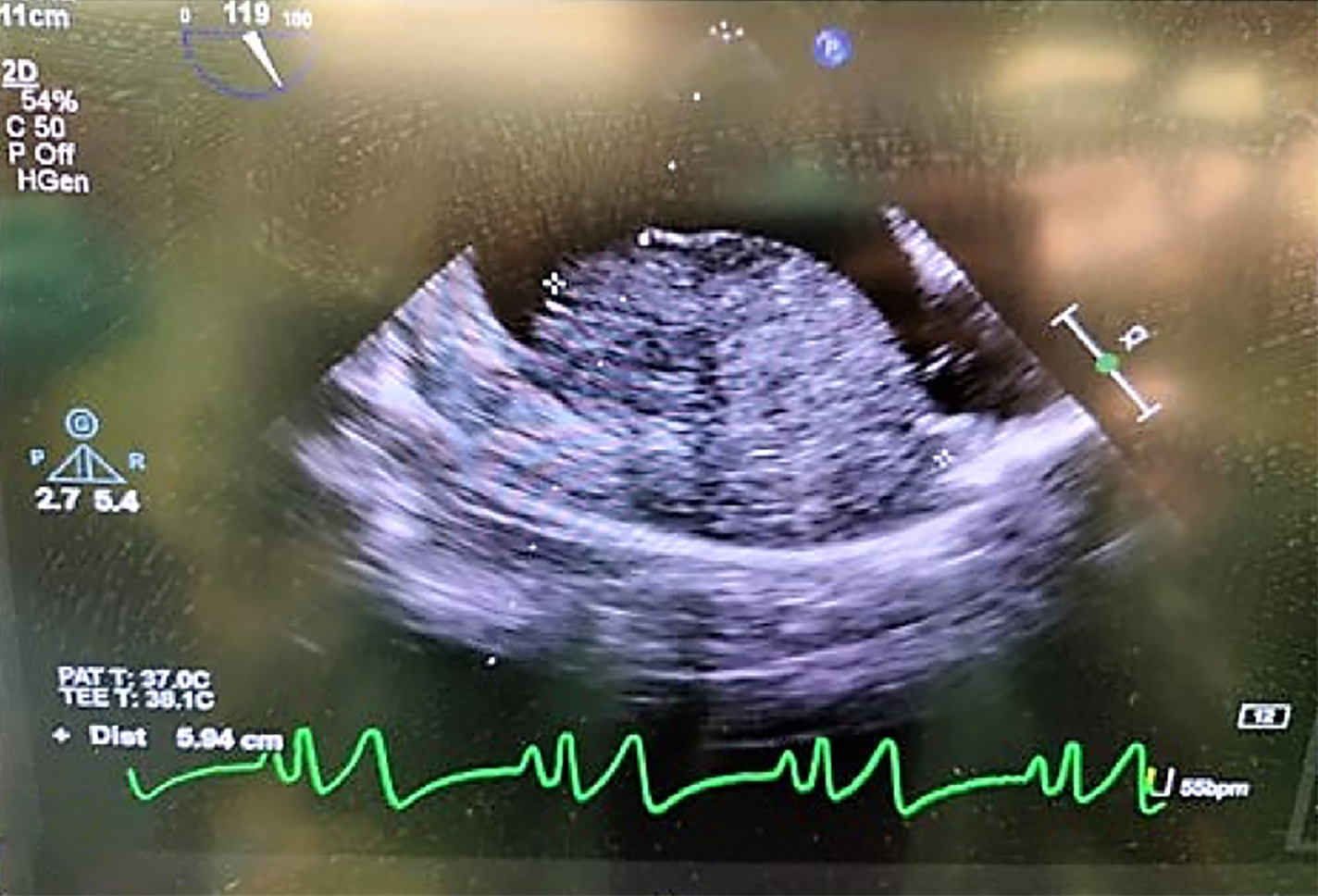 Figure 1: Echocardiogram showing a large, heterogeneous, mobile mass, in the right atrium.
Figure 1: Echocardiogram showing a large, heterogeneous, mobile mass, in the right atrium.
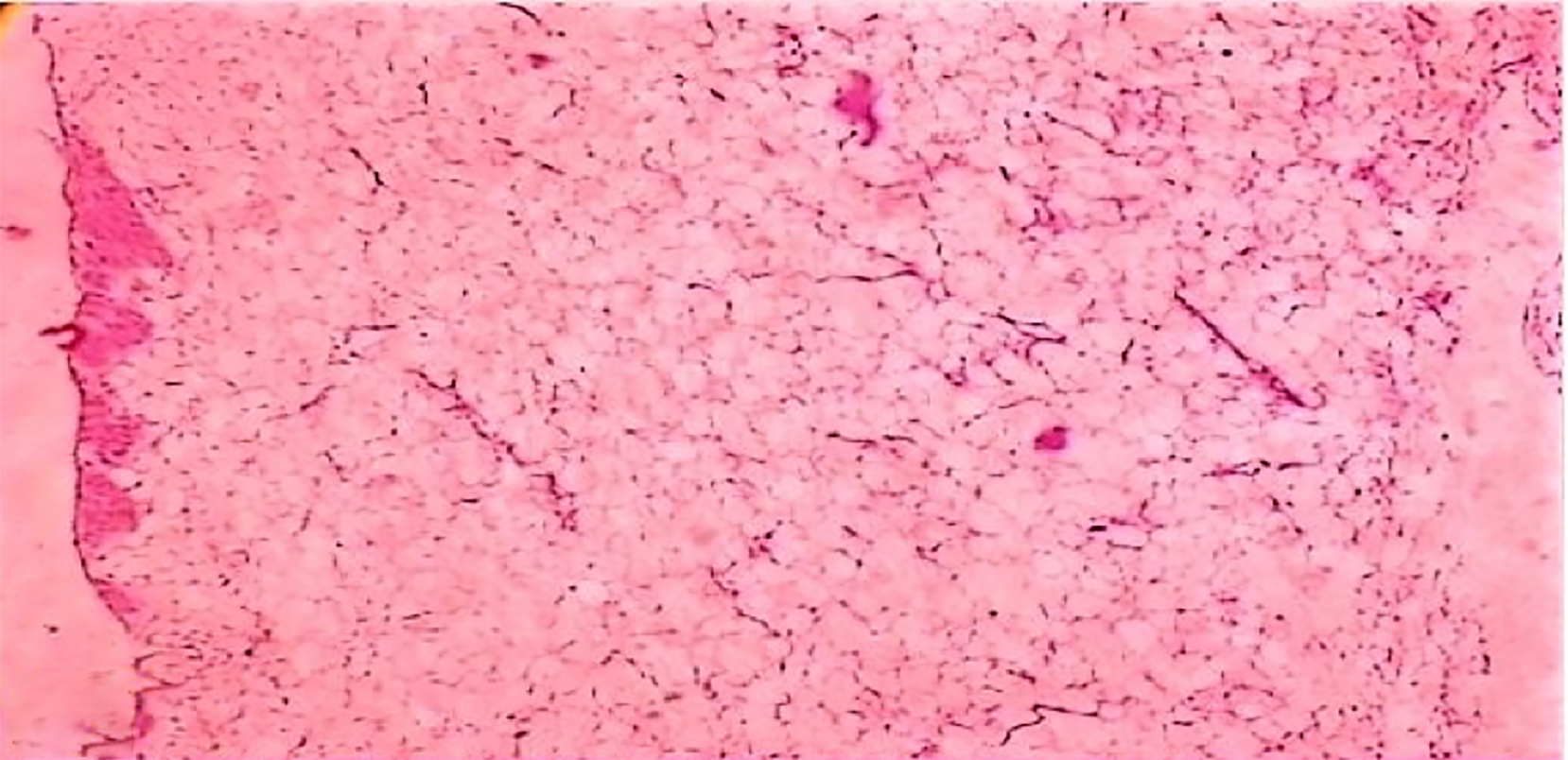 Figure 2: Photomicrograph showing well-circumscribed mass lesion comprised of mature adipocytes in sheets separated by thin wisps of fibrous tissue in a case of lipoma (hematoxylin and eosin staining, magnification = 100 ×).
Figure 2: Photomicrograph showing well-circumscribed mass lesion comprised of mature adipocytes in sheets separated by thin wisps of fibrous tissue in a case of lipoma (hematoxylin and eosin staining, magnification = 100 ×).
Case two: cardiac myxoma
A 53-year-old female presented to the emergency department with complaints of dyspnea, palpitations associated with fainting episodes and chest pain upon exertion for the last several months. Her medical history included hypertension and she was on irregular self-medication. All her laboratory findings and blood work were within normal limits. Her physical examination was unremarkable. Vitals were mostly normal except for blood pressure (145/90). Electrocardiogram was within normal limits. 2D echocardiogram revealed a left atrial mass myxoma measuring 7 × 5 × 3 cm. Further high-resolution CT thorax was done which revealed a well-defined hypodense lesion in the left atria with a differential diagnosis of left atrial myxoma or thrombus [Figure 3]. Additional imaging studies including cardiac MRI were performed which further confirmed the mass and its location. A CVTS consultation and surgery were performed, and a large size mass measuring 65 × 45 × 30 mm was removed and submitted for histopathology examination. In the histopathology section, a nodular mass with a whitish, soft, and glistening external surface was received. The cut surface was solid, whitish with foci of hemorrhage. Multiple paraffin-embedded and H&E-stained sections were examined under the microscope which revealed a well-circumscribed mass with low cellularity and composed of spindle- to-stellate cells with round to oval nuclei and eosinophilic cytoplasm. The stroma was myxoid and showed foci of hemorrhage and scattered pigment- laden macrophages. A final diagnosis of left atrial myxoma was made [Figure 4].
 Figure 3: High-resolution CT thorax showing a well-defined hypodense lesion in the left atria in a case of cardiac myxoma.
Figure 3: High-resolution CT thorax showing a well-defined hypodense lesion in the left atria in a case of cardiac myxoma.
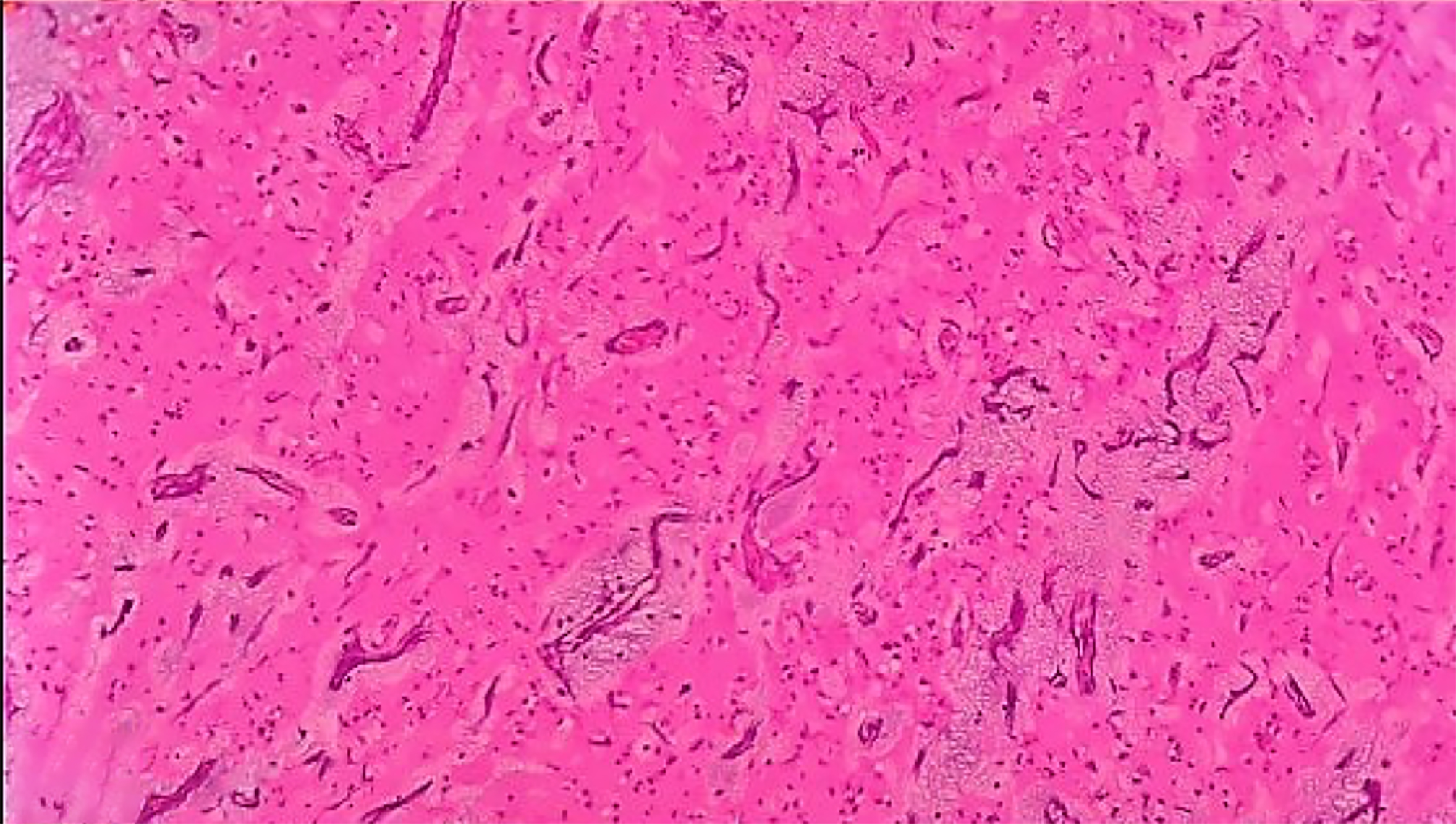 Figure 4: Photomicrograph showing myxoid stroma, foci of hemorrhage, and scattered pigment-laden macrophages in a case of left atrial myxoma (hematoxylin and eosin staining, magnification = 100 ×).
Figure 4: Photomicrograph showing myxoid stroma, foci of hemorrhage, and scattered pigment-laden macrophages in a case of left atrial myxoma (hematoxylin and eosin staining, magnification = 100 ×).
Case three: cardiac calcified amorphous tumor
A 32-year-old male patient presented to the emergency department with complaints of dyspnea on exertion and palpitations for two months. His past medical history included hypertension and he was on erratic self-medication. An extensive workup was done which included an echocardiogram and cardiac imaging (CT thorax) which showed a large right atrial mass with mild cardiomegaly and dilated right ventricle and right atrium. It was provisionally diagnosed as right atrial myxoma [Figure 5]. The patient underwent surgical resection of the mass under the clinical diagnosis of cardiac myxoma. In the pathology department, a tumor of 4 × 2 × 2 cm was received which was grey-white and firm in consistency. On the cut section, the specimen was yellowish-white with few hemorrhagic and calcified areas. Multiple random and paraffin-embedded sections were H&E-stained and examined under the microscope. Light microscopy revealed diffuse amorphous eosinophilic material along with multiple focal areas of calcification [Figure 6].
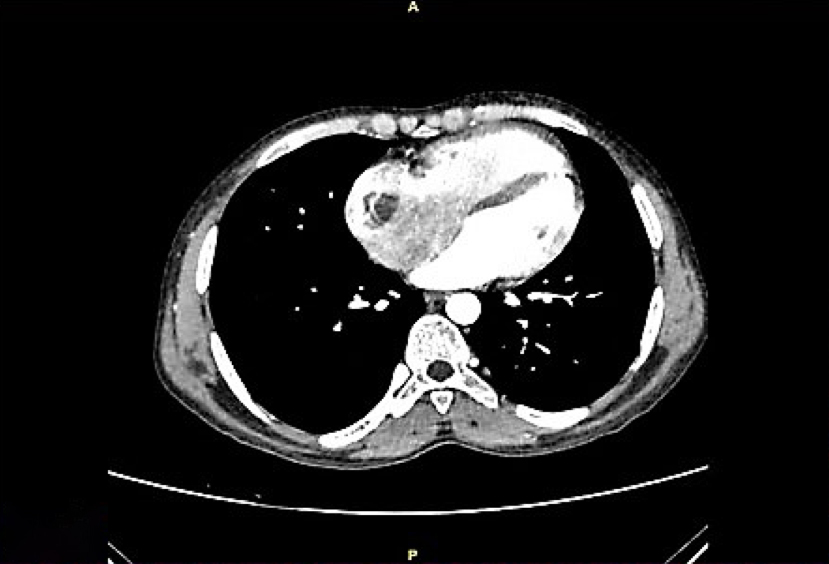 Figure 5: CT thorax showing a large right atrial mass with mild cardiomegaly and dilated right ventricle and right atrium.
Figure 5: CT thorax showing a large right atrial mass with mild cardiomegaly and dilated right ventricle and right atrium.
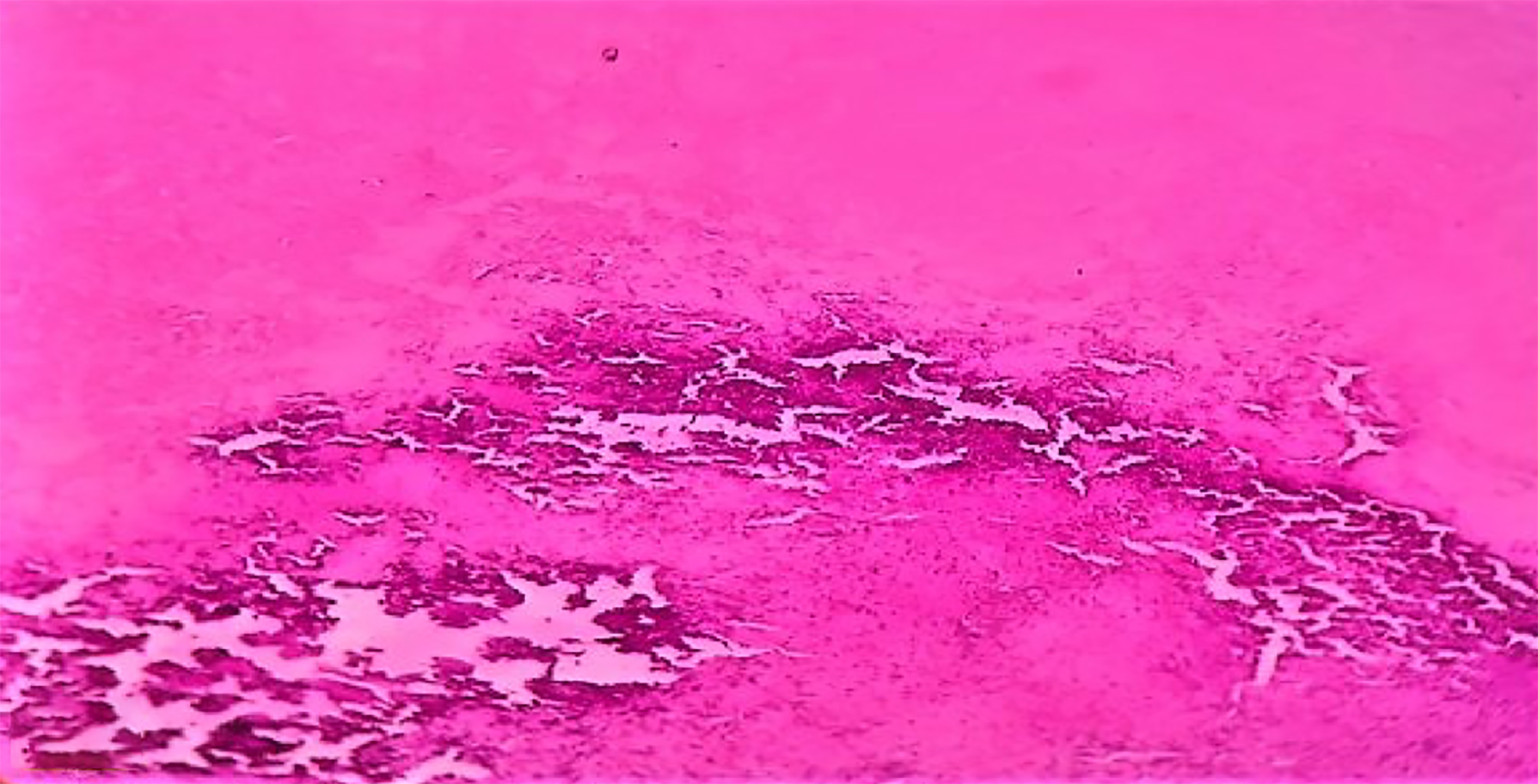 Figure 6: Photomicrograph showing diffuse amorphous eosinophilic material along with multiple areas of calcification in cardiac amorphous calcified tumor (hematoxylin and eosin staining, magnification = 100 ×).
Figure 6: Photomicrograph showing diffuse amorphous eosinophilic material along with multiple areas of calcification in cardiac amorphous calcified tumor (hematoxylin and eosin staining, magnification = 100 ×).
Case four: cardiac rhabdomyoma
An eight-month-old male patient was referred to cardiac emergency with severe breathlessness more so during feeding and inability to gain weight. An extensive workup was done which included a chest X-ray and echocardiogram. The X-ray showed mild cardiomegaly while echocardiogram showed a small echogenic right ventricular and septal mass which was diagnosed as rhabdomyoma. A cardiothoracic consultation was obtained, the patient was operated on, and a specimen was sent for histopathological examination. In the pathology department, a specimen measuring 0.8 × 0.4 × 0.4 cm was received. It was processed and paraffin-embedded tissue was stained with H&E and examined under the microscope. Light microscopy revealed a well-circumscribed tumor with large polygonal cells showing a centrally placed nuclei with clear to granular cytoplasm. Some cells were showing thin radiating processes known as ‘spider cells’ pathognomic for rhabdomyoma [Figure 7]. A final diagnosis of rhabdomyoma right ventricle was made.
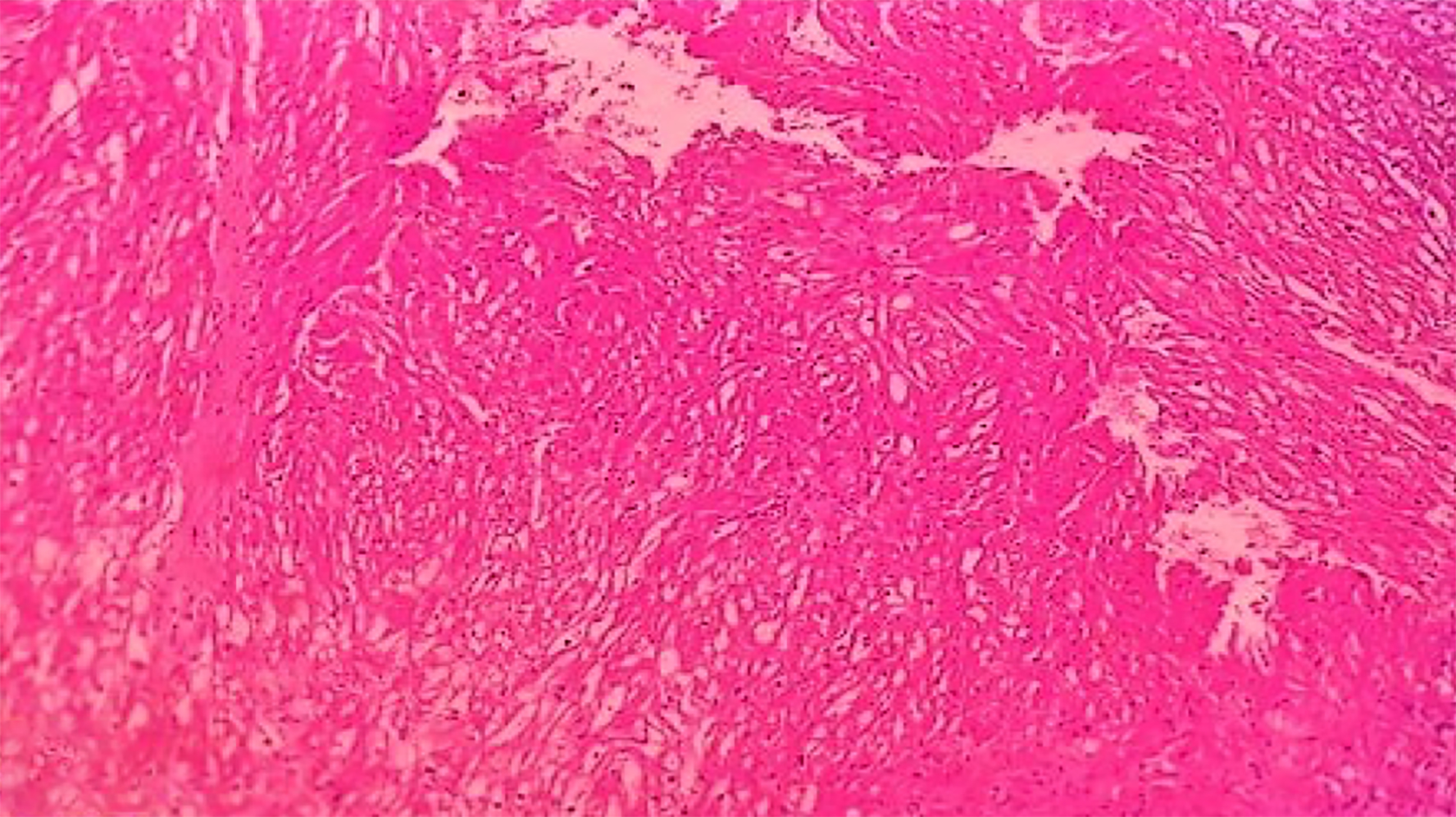 Figure 7: Photomicrograph showing a tumor with large polygonal cells showing a centrally placed nuclei and with clear to granular cytoplasm in cardiac rhabdomyoma (hematoxylin and eosin staining, magnification = 100 ×).
Figure 7: Photomicrograph showing a tumor with large polygonal cells showing a centrally placed nuclei and with clear to granular cytoplasm in cardiac rhabdomyoma (hematoxylin and eosin staining, magnification = 100 ×).
Case five: pericardial cyst
A 48-year-old male patient presented to the emergency department with complaints of repeated episodes of shortness of breath and persistent cough for the past 10 days. It was associated with two episodes of non-exertional chest tightness (lasting for one-minute duration each) over the last two days, which resolved spontaneously. His medical history included hypertension for the past eight years and he had been on regular medication. At the time of presentation, his physical examination was unremarkable. All his laboratory findings and blood work were within normal limits, along with negative cardiac enzymes. Electrocardiogram showed a normal sinus rhythm. Chest X-ray showed a large opacity concealing the right heart border. His echocardiogram was normal, and no pericardial effusion was seen. A CT scan was done, which revealed the presence of a 5 × 3 cm cyst at the right cardio phrenic angle. A provisional diagnosis of the right pericardial cyst was made. Subsequently, a CVTS consultation was done for the patient. Given the patient’s significant symptoms and large size of the mass, complete surgical resection of the cyst was performed. The excised tissue was sent to the histopathology department for examination. Grossly, the cyst measured 5 × 3 × 2 cm and weighed 40 g. The external surface was smooth, when opened 40 mL of serous fluid oozed out. Cut surface was unilocular with a smooth cyst lining. Multiple paraffin-embedded and H&E-stained sections were examined under the microscope. It revealed a cystic mass, with its wall lined by a single layer of flattened epithelium along with underlying fibrous tissue that showed focal areas of chronic inflammatory infiltrate. Few congested blood vessels were noted. Deeper fibro-adipose tissue was also seen [Figure 8]. A final diagnosis of right simple pericardial cyst was made.
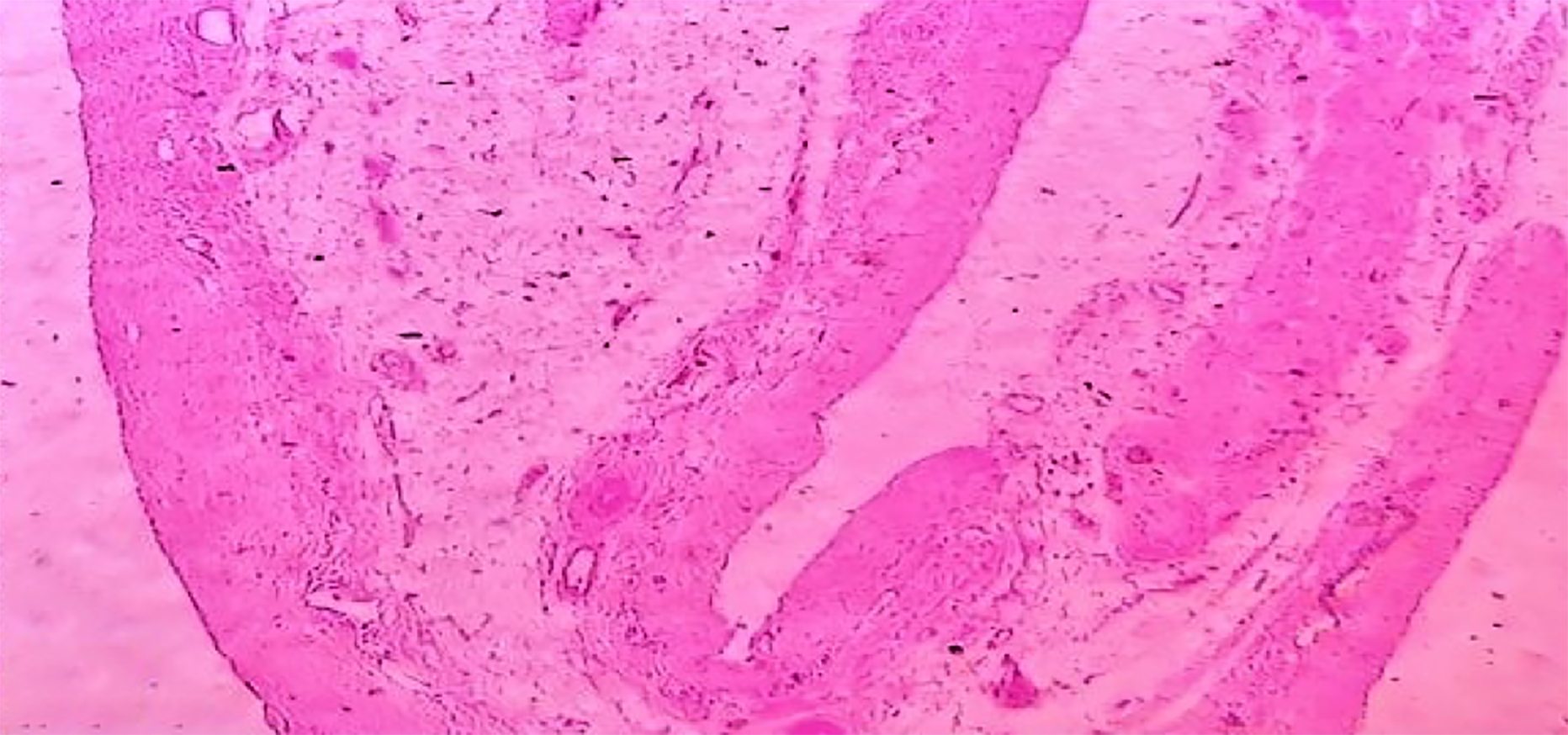 Figure 8: Photomicrograph showing a cyst wall lined by a single layer of flattened epithelium along with underlying fibrous tissue in a case of pericardial cyst (hematoxylin and eosin staining, magnification = 100 ×).
Figure 8: Photomicrograph showing a cyst wall lined by a single layer of flattened epithelium along with underlying fibrous tissue in a case of pericardial cyst (hematoxylin and eosin staining, magnification = 100 ×).
Discussion
A cardiac lipoma is a rare benign tumor of the heart, most commonly found in the endocardium of the right atrium and the left ventricle. It represents only 8.4% of all primary cardiac tumors (which are in themselves very rare, the overall prevalence varying between 0.17% and 0.19%).5 A cardiac lipoma is an encapsulated tumor, composed primarily of mature fat cells. It is usually seen in the fifth and sixth decades of life but can occur in any age group. Both males and females may be equally affected. It is usually asymptomatic. Symptoms, if present, depend upon the tumor size and location within the heart and varies from mild chest discomfort to dyspnea and even sudden death. Cardiac MRI is the investigation of choice. Histopathological examination is required for confirmation of diagnosis and to rule out well-differentiated liposarcoma. Excision surgery is part of the treatment. To avoid a tumor recurrence, it is crucial to remove the complete tumor together with the capsule and pedicle intraoperatively.6
Cardiac myxoma is the most common primary heart tumor seen in adults. It is most commonly found in the left atrium, occurring as a sporadic, solitary, and pedunculated mass close to the fossa ovalis. It is a rare and benign neoplasm with an approximate incidence of up to 0.2% in some autopsy series.7 It usually affects people aged between 30–60 years.8 Females are generally affected more than males. General symptoms associated with cardiac myxomas can be, breathing difficulty when lying flat or on one side, sleep apnea, chest pain or tightness, dizziness, fainting, palpitations, and exertional dyspnea. Complications of a myxoma can include embolism, valve obstruction, intracardiac flow obstruction, and other constitutional symptoms. As a result, it can be potentially life-threatening and thus calls for prompt diagnosis and surgical resection. Echocardiogram (both transthoracic and transesophageal) is the imaging modality of choice. Histopathology (including positivity for endothelial cell markers - CD31 and CD34) is required for definitive diagnosis. Prognosis is excellent if the tumor is promptly resected.7
Calcified amorphous tumor (CAT) is a rare benign intracavitary mass, composed of nodular calcium deposits on a background of amorphous fibrinous material. It is most commonly found in the mitral annulus and left ventricle, although it may occur in any chamber of the heart.9 About 44 cases of CAT have been documented so far, 10% being in association with stroke.9 Females have shown greater preponderance than males. The pathogenesis still remains largely unknown. The most common clinical presentation is dyspnea on exertion, occurring due to blood flow obstruction by the mass. Other presenting features can be syncope, angina, pulmonary embolism, or systemic embolism. Rarely, a patient may just get diagnosed incidentally. Echocardiogram is the imaging modality of choice. Histopathology is required for definitive diagnosis since clinical and echocardiological presentations of CAT are similar. Surgical resection is the gold standard of treatment. However, in high-risk patients (where surgical intervention may be dangerous), anticoagulation therapy and long-term follow-up might be considered alternative modes of treatment.9
A cardiac rhabdomyoma is the most common type of pediatric cardiac tumors, occurring during gestation or within one year of birth. It is a rare and benign mesenchymal neoplasm of striated muscle origin, the approximate incidence being approximately 1 in 20 000 births.10 It is most commonly associated with tuberous sclerosis and usually involves the ventricular myocardium, atria, cavoatrial junction, or the epicardial surface. Ultrasound or echocardiogram is the usual imaging modality of choice. The majority of cardiac rhabdomyomas are asymptomatic and regress spontaneously. However, if they are symptomatic (causing left ventricular outflow tract obstruction, refractory arrhythmias, or hemodynamic compromise with subsequent congestive cardiac failure), partial or complete surgical resection is the treatment of choice.
A pericardial cyst of the mediastinum is typically found at the cardiophrenic angle. It may occur in patients of all age groups. It is usually asymptomatic; rarely it may present with dyspnea, chest pain, or chronic cough. It is considered as a rare congenital anomaly with an approximate incidence of 1 in 100 000 persons.11 Pericardial cysts comprise only 7% of all mediastinal masses and 33% of all mediastinal cysts.11 CT scan without contrast is the investigation of choice wherein findings include a single non-enhancing homogenous ovoid thin-walled mass without any solid component. A histopathological examination is done to confirm the diagnosis. Since most patients are asymptomatic, the treatment is usually conservative. If the patient becomes symptomatic or the size of the cyst progressively increases, then surgical intervention may be needed. These surgical procedures may include percutaneous aspiration, ablation/ethanol sclerosis, surgical resection of cyst via thoracotomy, sternotomy, video-assisted thoracoscopic surgery, or mediastinoscopy.11
Conclusion
Primary cardiac lesions are still so rare that their overall prevalence is 0.17–0.19%, of which 75% are benign and 25% are malignant. Presently, the only evidential data available for the management of these tumors are derived from either small case series or case reports. The primary challenge lies in the timely diagnosis of these tumors since their presenting signs and symptoms are mostly non-specific and could remain undiagnosed until a late stage. This might adversely affect the overall prognosis and even the survival of the patient. Henceforth, early diagnosis and prompt treatment are the need of the hour to ensure better outcomes for the patient. A multidisciplinary approach and quick collaborative teamwork of the concerned physicians, radiologists, cardiothoracic surgeons, and above all pathologists would be most optimal to treat primary cardiac lesions.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study. Informed consent is taken for publication and research purposes.
references
- 1. Chitwood Jr WR. Clarence Crafoord and the first successful resection of a cardiac myxoma. The Annals of Thoracic Surgery 1992;54(5):997-998.
- 2. Leja MJ, Shah DJ, Reardon MJ. Primary cardiac tumors. Tex Heart Inst J 2011;38(3):261-262.
- 3. Wu S, Teng P, Zhou Y, Ni Y. A rare case report of giant epicardial lipoma compressing the right atrium with septal enhancement. J Cardiothorac Surg 2015 Nov;10:150.
- 4. Wang H, Hu J, Sun X, Wang P, Du Z. An asymptomatic right atrial intramyocardial lipoma: a management dilemma. World J Surg Oncol 2015 Feb;13:20.
- 5. Ismail I, Al-Khafaji K, Mutyala M, Aggarwal S, Cotter W, Hakim H, et al. Cardiac lipoma. J Community Hosp Intern Med Perspect 2015;5(5):28449.
- 6. Griborio-Guzman AG, Aseyev OI, Shah H, Sadreddini M. Cardiac myxomas: clinical presentation, diagnosis and management. Heart 2022 May;108(11):827-833.
- 7. Reynen K. Cardiac myxomas. N Engl J Med 1995 Dec;333(24):1610-1617.
- 8. Formelli B, Farina A, Pescini F, Palumbo V, Grazia D’Alfonso M, Oddo A, et al. Cardiac calcified amorphous tumor as a rare cause of ischemic stroke: clinical case. Circ Cardiovasc Imaging 2020 Jan;13(1):e009623.
- 9. Guschmann M, Entezami M, Becker R, Vogel M. Intrauterine rhabdomyoma of the heart. A case report. Gen Diagn Pathol 1997 Dec;143(4):255-259.
- 10. Meredith A, Zazai IK, Kyriakopoulos C. Pericardial cyst. InStatPearls 2022. StatPearls Publishing.
- 11. Qamar Y, Gulzar M, Qamar A, Sabry H, Minhas T. An incidental finding of a large pericardial cyst. Cureus 2022 Apr;14(4):e23917.