A21-year-old male diagnosed with familial hypofibrinogenemia and had multiple admissions for bleeding episodes. He was diagnosed with hypertension at 12 years old and was started on treatment. A computed tomography angiography (CTA) at that time showed a normal diameter of the aorta and no major vascular changes. A recent CTA done when the patient was 21 years old revealed long segment narrowing of the distal thoracic and abdominal aorta, with severe stenosis, at the level of renal artery bifurcation with bilateral renal artery stenosis and significant collaterals within the mesentery, while the aorta above and below was normal in caliber. Hence a diagnosis of middle aortic syndrome (MAS) was made [Figure 1].
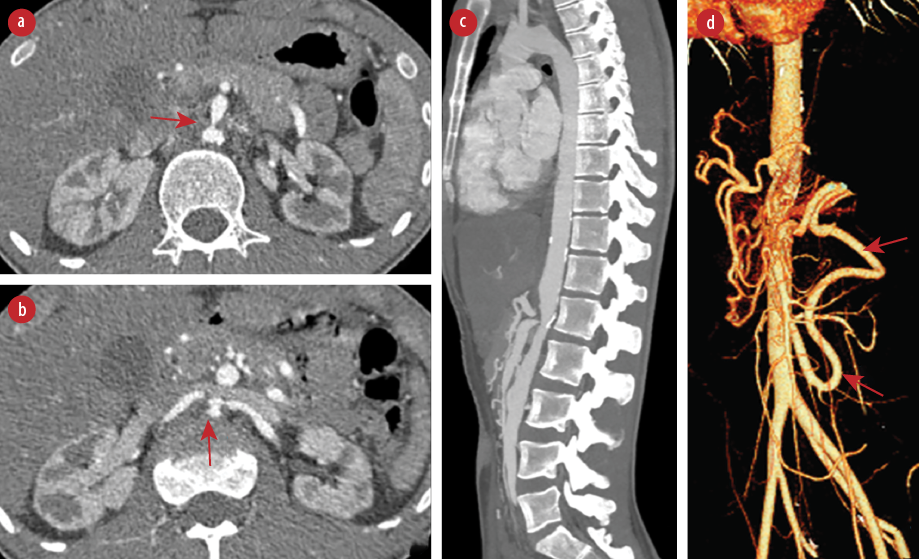 Figure 1: Computed tomography angiography (CTA) of the aorta. (a) Axial view at the level of superior mesenteric artery (SMA) origin (red arrow) and (b) at the level of renal arteries (red arrow) showing focal short segment severe luminal narrowing of the aortic lumen, origin of SMA, and bilateral renal arteries. (c) Sagittal maximum intensity projection CTA image showing focal short segment severe luminal narrowing of the aortic lumen, celiac axis, and SMA origin. (d) 3D volume rendered image showing enlarged splanchnic collateral (inferior mesenteric artery and arc of Riolan) (red arrows).
Figure 1: Computed tomography angiography (CTA) of the aorta. (a) Axial view at the level of superior mesenteric artery (SMA) origin (red arrow) and (b) at the level of renal arteries (red arrow) showing focal short segment severe luminal narrowing of the aortic lumen, origin of SMA, and bilateral renal arteries. (c) Sagittal maximum intensity projection CTA image showing focal short segment severe luminal narrowing of the aortic lumen, celiac axis, and SMA origin. (d) 3D volume rendered image showing enlarged splanchnic collateral (inferior mesenteric artery and arc of Riolan) (red arrows).
MAS is a rare vascular pathology confined to the distal thoracic or abdominal aorta.1 It is characterized by segmental or diffuse narrowing of the aorta or its branches. The majority of the cases of MAS are congenital, caused by an anomaly of fusion of the paired embryonic dorsal aorta. Renal artery involvement occurs in 65–70% and visceral involvement in 25%.2 It can be acquired as a result of conditions such as Takayasu arteritis, neurofibromatosis, or fibromuscular dysplasia. Although our patient has normal inflammatory markers and a negative autoimmune screen, the evidence of previous normal aorta caliber and the current radiological changes of multiple artery stenosis makes the diagnosis of acquired MAS secondary to Takayasu arteritis most likely.
Presentation is usually with refractory hypertension in young people. Kadoya et al,3 reported a similar patient with congenital MAS who presented with juvenile hypertension. Other presentations can be abdominal pain due to mesenteric ischemia, early fatigue, and bilateral lower limb claudication. Diagnosis is made with CTA or magnetic resonance angiography. The classical finding on CTA is a progressive narrowing of the distal descending thoracic and abdominal aorta with collaterals.4
Management includes the best medical therapy through blood pressure control. In addition, patients may require an endovascular, surgical, or hybrid approach for renal artery/mesenteric stenosis and disabling claudication. Each strategy has its limitations and needs to be individualized. Intervention is usually indicated in severe hypertension or in childhood and teenage years to prevent the cardiovascular complications of prolonged hypertension such as coronary artery disease, congestive heart failure, left ventricular hypertrophy, and cerebrovascular accidents.2
These patients need to be on long-term follow-up with a multidisciplinary team. The prognosis of conservative management is usually poor; therefore, surgical reconstruction is advised.1,2 Our patient was managed with blood pressure control only, and all surgical options were deferred as his hematological condition made him at high risk of bleeding. His blood pressure was controlled using two anti-hypertensive medications.
Disclosure
The authors declared no conflicts of interest. A written consent was obtained for the publication of this case report.
references
- 1. Delis KT, Gloviczki P. Middle aortic syndrome: from presentation to contemporary open surgical and endovascular treatment. Perspect Vasc Surg Endovasc Ther 2005 Sep;17(3):187-203.
- 2. Rumman RK, Nickel C, Matsuda-Abedini M, Lorenzo AJ, Langlois V, Radhakrishnan S, et al. Disease beyond the arch: a systematic review of middle aortic syndrome in childhood. Am J Hypertens 2015 Jul;28(7):833-846.
- 3. Kadoya Y, Zen K, Saburi M, Matoba S. Mid-aortic syndrome: a rare cause of juvenile hypertension. Intern Med 2018 Feb;57(3):447.
- 4. Kusel K, Zubrowski H, Weerakkody Y. Sonographic findings in mid-aortic syndrome. BJR Case Rep 2020 Oct;7(1):20200123.