Entomophthoromycosis is a rare subcutaneous fungal infection seen in immunocompetent individuals, and is caused by Conidiobolus coronatus, C. incongruus, and C. lampraugesa. Cases have emerged mostly from tropical regions of Africa, South America, and Asia.1 Our early patients had mixed responses to treatment such as slow response and delayed recurrence beyond one year of follow-up. This article describes our experience with a modified protocol. The drug regimen has an initial ‘intensive phase’ aimed at eliciting early response, followed by an ‘eradication phase’ which seeks to prevent delayed recurrence commonly seen on long-term follow-up. This study tries to establish a universal treatment protocol that can treat and prevent delayed recurrence of the disease.
Case Report
We report the results of five cases treated over the past five years in our institution [Table 1].
Table 1: Rhino-facial entomophthoromycosis cases treated at All India Institute of Medical Sciences between May 2013 and May 2020.
|
1
|
42/Male
|
Biopsy
|
KI + Itraconazole
|
10
|
Skin rashes
|
Complete
|
48
|
|
2
|
18/Female
|
Biopsy
|
KI + Itraconazole
|
10
|
Hypothyroidism
|
Complete
|
36
|
|
3
|
45/Male
|
Biopsy
|
KI + Itraconazole
|
10
|
None
|
Complete
|
32
|
|
4
|
35/Male
|
FESS
|
KI + Itraconazole
|
12
|
None
|
Complete
|
28
|
KI: potassium iodide; FESS: functional endoscopic sinus surgery.
All the patients presented with a three to six months history of progressive facial swelling, nasal obstruction, and reduced sensation in the swollen area [Figure 1]. The induration typically extended beyond the swelling. Sub-labial biopsy was performed to confirm the diagnosis. All patients underwent complete hematological and clinical evaluation to rule out systemic comorbidities. All were found to be immunocompetent.
 Figure 1: (a) Typical presentations of conidiobolomycosis depicting subcutaneous facial swelling. (b) The characteristic nasal obstruction decreased sensation over the area of swelling. The induration typically extended beyond the swelling.
Figure 1: (a) Typical presentations of conidiobolomycosis depicting subcutaneous facial swelling. (b) The characteristic nasal obstruction decreased sensation over the area of swelling. The induration typically extended beyond the swelling.
The culture of the biopsy showed conidia with papillate base, confirmatory for entomophthoromycosis [Figure 2]. After the confirmation of the diagnosis, patients were initiated on supersaturated potassium iodide (KI) solution, prepared by dissolving KI in absolute ethyl alcohol (1 gm/mL, i.e., one drop ~ 67 mg). The dose was titrated for adverse effects, initially starting with three drops thrice daily orally, progressively increasing up to 20 drops based on the tolerance of skin and gastrointestinal side effects. Patients were simultaneously initiated on oral itraconazole therapy at 400 mg twice daily for two days as a loading dose, followed by 200 mg twice daily for six months.1 This dosage schedule was used in our pilot patient, a 16-year-old girl who had a good response to this protocol, though fungal elements persisted in the area of induration post six months of therapy.1 After monitoring her thyroid, liver, and renal functions, monotherapy of KI solution drops was continued for additional four months for complete resolution.
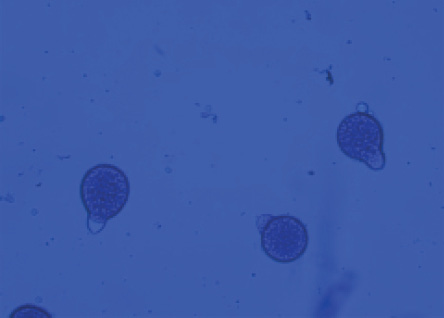 Figure 2: Microbiological review of culture specimen in lactophenol cotton blue staining under 40 × magnification revealed conidia with papillate base.
Figure 2: Microbiological review of culture specimen in lactophenol cotton blue staining under 40 × magnification revealed conidia with papillate base.
All patients responded well to our two-phase treatment protocol with no recurrence noted over a minimum follow-up period of 24 months. One patient who underwent surgery prior to being referred to us had residual fungal induration as revealed by biopsy; he needed two extra months of KI drops therapy [Figure 3]. Our criteria for complete resolution was complete resolution of swelling and induration. During therapy, one patient developed transient skin rashes and another hypothyroidism, which were managed with antihistamines and thyroxine supplementation. The latter patient’s transient hypothyroidism settled down over the next 36 months.
 Figure 3: Minimal induration persists even after resolution of swelling, suggestive of residual lesion. Biopsy revealed fungal elements retained in the induration (red arrow).
Figure 3: Minimal induration persists even after resolution of swelling, suggestive of residual lesion. Biopsy revealed fungal elements retained in the induration (red arrow).
Discussion
Entomophthoromycosis is clinically rare and it should be differentiated from other neoplastic lesions.2 Within the limited anti-fungal medication options, we should choose the most appropriate agent. Our five-year literature search with keywords ‘rhino-facial fungal infection’, ‘entomophthoromycosis’, and ‘conidiobolomycosis’ yielded 13 studies over the period 2014–2020 [Table 2].3–15
Table 2: Review of five years’ literature on management of cases of entomophthoromycosis.
|
Yu et al,3 2014
|
China
|
1
|
Surgical and Medical
|
Itraconazole
|
9
|
|
Raveenthiran et al,4 2015
|
India
|
16
|
Surgical and Medical
|
KI. In one case itraconazole was added
|
2–8
|
|
Cherian et al,5 2015
|
India
|
1
|
Surgical and Medical
|
Itraconazole and terbinafine
|
6
|
|
Arora et al,62016
|
India
|
1
|
Medical
|
KI and itraconazole
|
1
|
|
Gupta et al,7 2016
|
India
|
10
|
Medical
|
KI, itraconazole, amphotericin B, and fluconazole
|
6–9
|
|
Cao et al,8 2018
|
China
|
1
|
Medical
|
KI, trimethoprim-sulfamethoxazole, and itraconazole
|
6
|
|
Deak et al,9 2018
|
UAE
|
1
|
Surgical and Medical
|
Itraconazole
|
18
|
|
Gupta et al,10 2018
|
India
|
2
|
Medical
|
KI and itraconazole/ voriconazole
|
5 and 6
|
|
Das et al,11 2019
|
India
|
6
|
Medical
|
KI, itraconazole, fluconazole, ketoconazole, terbinafine, and steroids
|
5–6
|
|
Chaiyasate et al,12 2020
|
Thailand
|
3
|
Medical
|
Itraconazole, KI, and cotrimoxazole
|
6–12
|
|
Wankhade et al,13
2020
|
India
|
2
|
Surgical and Medical
|
Amphotericin
|
1
|
|
Sigera et al,14 2020
|
Sri Lanka
|
3
|
Surgical and Medical
|
Itraconazole and terbinafine/amphotericin
|
4–6
|
KI: potassium iodide.
The treatment was primarily medical, except for six studies where surgical debridement was also performed.3–5,9,13,14 The medical management included KI, itraconazole, amphotericin B, fluconazole, terbinafine, cotrimoxazole, and ketoconazole. The treatment duration ranged from a minimum of one month to a maximum of 18 months. In the majority of the studies, the treatment duration was six months. The above data demonstrates a lack of uniformity in approach. As the infection is typically seen in immunocompetent individuals, surgical debridement is not warranted and may instead cause more resistance due to fungal dissemination and tissue scarring. This was observed in one of our cases who had undergone surgery before being referred to us. The patient required two additional months of KI monotherapy to subdue the persistent induration. The use of inappropriate anti-fungal medication for inadequate time period leads to partial response and resistance. This can be very dangerous for the patient, considering the availability of limited anti-fungal medications. Debridement also helps in dissemination of the disease and prevents early resolution. Our study emphasizes the need to use appropriate anti-fungal medication for adequate duration to prevent resistance and ascertain a complete response. The surgical debridement should also be limited to rare scenarios where there is no response to treatment and as a last resort.
Our standardized protocol of management with a predefined treatment duration is summarized in Table 3. The treatment begins after the diagnosis of entomophthoromycosis is confirmed by pathological or microbiological evaluation. In our experience, a biopsy from any persistent minimal residual induration invariably reveals fungal elements requiring prolonged therapy.
Table 3: The protocol for managing entomophthoromycosis cases.
Our definition of response is complete resolution of induration, indicating eradication of fungal elements. In our two-phase protocol, the initial ‘intensive phase’ with a two-drug therapy protocol is meant to achieve rapid response without the need for surgery. The transient side effects of this phase are managed with dose adjustments. The second ‘eradication phase’ consists of KI monotherapy which seeks total eradication of the fungus, thus preventing the common problem of long-term recurrence. In case of non-resolution of swelling, a microbiological analysis should be performed to identify the most appropriate drug.
The antifungal action of KI is observable with Splendore-Hoeppli reaction on fungal infections such as sporotrichosis, entomophthoromycosis, chromoblastomycosis, and mycetomas.16 KI is hypothesized to enhance the outcome of complement fixation-dependent cytolysis by either enhancing or retarding the reaction.17 Contraindications to KI include pregnancy or hypersensitivity to iodide or acute infections like tuberculosis or bronchitis.18 Dose limiting-adverse reactions include hypothyroidism, parotitis, acneiform skin eruptions, nausea, or vomiting.19 Adding a second anti-fungal agent may enhance the response leading to early disappearance of swelling and induration. Long-term recurrence of the infection is due to the incomplete resolution of induration which harbors the fungus. This has led us to consider the complete resolution of induration as a marker for eradication of fungus. Surgery induces dissemination of fungus and is associated with poorer response to treatment and the need for prolonged treatment. A four-month regimen of KI drops helps in eradication of the fungus and is vital to prevent delayed recurrence.
Conclusion
The primary treatment modality for entomophthoromycosis is with KI solution in titrating doses. The addition of synergistic antifungals like itraconazole accelerates the resolution. The total duration of our treatment protocol is 10 months with phase 1 (intensive phase) comprising two-drug therapy (KI and itraconazole) for six months, followed by phase 2 (eradication phase) for four months of monotherapy with KI drops. Early cessation of treatment is associated with delayed recurrence. The reappearance of induration is an early sign of recurrence and should be evaluated. Hypothyroidism may occur during therapy and needs regular monitoring throughout the treatment period. Surgical debridement should be avoided due to its long-term detrimental effects. Any delayed response to treatment would warrant microbiological analysis with reconfirmation of diagnosis and its sensitivity pattern.
Disclosure
The authors declared no conflicts of interest. Informed consent has been obtained from all the patients included in the study. Institutional permission has been obtained to publish the data and patients’ consent has been obtained to use their clinical photographs for publication.
references
- 1. Chappity P, Hallur V. Subcutaneous fungal infection of the face. Lancet Infect Dis 2021 Feb;21(2):296.
- 2. Prabhu RM, Patel R. Mucormycosis and entomophthoramycosis: a review of the clinical manifestations, diagnosis and treatment. Clin Microbiol Infect 2004 Mar;10(Suppl 1):31-47.
- 3. Yu WN, Chen CJ, Chen CM. Pharyngeal entomophthoromycosis. J Chin Med Assoc 2014 Jun;77(6):337-340.
- 4. Raveenthiran V, Mangayarkarasi V, Kousalya M, Viswanathan P, Dhanalakshmi M, Anandi V. Subcutaneous entomophthoromycosis mimicking soft-tissue sarcoma in children. J Pediatr Surg 2015 Jul;50(7):1150-1155.
- 5. Cherian LM, Varghese L, Panchatcharam BS, Parmar HV, Varghese GM. Nasal conidiobolomycosis: a successful treatment option for localized disease. J Postgrad Med 2015 Apr-Jun;61(2):143-144.
- 6. Arora N, Bhargava EK, Rai V. Nasal conidiobolomycosis- the unknown threat. J Clin Diagn Res 2016 Dec;10(12):MJ01.
- 7. Gupta M, Narang T, Kaur RJ, Manhas A, Saikia UN, Dogra S. A prospective case series evaluating efficacy and safety of combination of itraconazole and potassium iodide in rhinofacial conidiobolomycosis. Int J Dermatol 2016 Feb;55(2):208-214.
- 8. Cao C, Khader JA. Rhinofacial entomophthoromycosis. N Engl J Med 2018 Mar;378(9):e13.
- 9. Deak L, Mudalagiriyappa S, Ballin A, Saxton D, Chakrabarti A. A rhinofacial conidiobolus coronatus fungal infection presenting as an intranasal tumor. Sultan Qaboos Univ Med J 2018 Nov;18(4):e549-e552.
- 10. Gupta N, Kumar R, Ramteke P, Soneja M. Look before you leap: a case series of conidiobolomycosis from the Indian subcontinent. J Family Med Prim Care 2018 Sep-Oct;7(5):1113-1115.
- 11. Das SK, Das C, Maity AB, Maiti PK, Hazra TK, Bandyopadhyay SN. Conidiobolomycosis: an unusual fungal disease-our experience. Indian J Otolaryngol Head Neck Surg 2019 Nov;71(Suppl 3):1821-1826.
- 12. Chaiyasate S, Salee P, Sukapan K, Teeranoraseth T, Roongrotwattanasiri K. Rhinofacial entomophthoramycosis case series, the unusual cause of facial swelling. Ann Med Surg (Lond) 2020 Jul;57:41-45.
- 13. Wankhade AB, Patro P, Arora RD, Nagarkar NM. Nasofacial rhinoentomophthoramycosis: a report of two cases from Central India. J Oral Maxillofac Pathol 2020 Feb;24(Suppl 1):S124-S127.
- 14. Sigera LS, Janappriya GH, Lakshan MT, Pitigalage NJ, Jayasekera PI, Dayasena RP, et al. Rhinofacial conidiobolomycosis: a case series and review of the literature. Ear Nose Throat J 2021 Sep;100(5_suppl):835S-841S.
- 15. Dutta S, Sarkar S, Linka U, Dora S. Conidiobolomycosis: a case report of rare fungal infection from the eastern India. Indian Dermatol Online J 2015 Nov-Dec;6(6):393-395.
- 16. Sterling JB, Heymann WR. Potassium iodide in dermatology: a 19th century drug for the 21st century-uses, pharmacology, adverse effects, and contraindications. J Am Acad Dermatol 2000 Oct;43(4):691-697.
- 17. Maiti P, Das S, Ghosh T, Dey R. Effects of potassium iodide on low avid immunological reactions: probable mechanism of action on selective fungal infections. Ann Med Health Sci Res 2013 Jul;3(3):397-401.
- 18. Jones HE. Fungal infections. Dermatology. Norwalk Connel: Appleton & Langec; 1991. p.154.
- 19. Wiederman BL. Sporotrichosis. Textbook of pediatric infectious diseases. Philadelphia: Saunders, 1992.