|
Abstract
Objective: To study the effect of cigarette smoking on seminal fluid parameters, namely; volume, sperm concentration, and motility, as well as morphology, leukocyte infiltration, among males complaining of infertility.
Methods: Between August 2010 and July 2011, seminal fluid analysis was done for 1438 males who are partners of couples who visited the infertility clinic at Prince Rashid Ben Al Hassan Hospital (PRH) for infertility. The men who fit the inclusion criteria (n=960) were classified into two groups: group a (non-smokers; n=564) and group B (smokers; n=396), which represents 41.25% of the study group. Seminal fluid was collected using masturbation after 3-5 days of abstinence then analyzed for volume, sperm count, sperm concentration, motility and morphology. In order to analyze whether the number of cigarettes smoked per day has an effect on the spermatogram; the smoking men were divided into two subgroups: the heavy smokers (n=266) and non-heavy smokers (n=130).
Results: A total of 960 adult males were enrolled. Their age ranged between 21 and 76 years, 564 were non-smokers with mean age of 36. 45±6.27 (Mean±SD). Three-hundred-and-ninety-six were smokers with a mean age of 34.35±4.25 (Mean±SD). There was a significant effect of smoking on the motility of sperms and the ratios of abnormality (p<0.005). Concentration appeared not to be affected by smoking. Furthermore, the group of heavy smokers were found to have lower sperm concentrations and a higher percentage of abnormal sperms compared to the non-heavy smokers.
Conclusion: Cigarette smoking has a deleterious effect on some of the seminal fluid parameters (motility, morphology and leukocyte count) which in turn may result in male subfertility.
Keywords: Cigarette smoking; Sperm count; Sperm motility; Sperm morphology.
Introduction
Infertility is defined as the inability to conceive after 12 months of unprotected intercourse, and estimations of the World Health Organization indicates that about 8% of couples worldwide, and 10-15% in industrialized nations, experience some form of infertility.1 Male infertility plays a key role in conception difficulties of up to 40% infertile couples. Although in some men, a specific disorder may be present in the majority; however, no apparent reason for infertility can be found. This has drawn attention to the impact of lifestyle and environmental factors, especially diet, obesity, smoking, alcohol intake, recreational drug use, and exposure to environmental toxins, on reproductive health of such men.2
Many studies have shown that cigarette smoking has a deleterious effect on both male and female reproductive systems and fertility.3-10 Nowadays, the population of cigarette smokers is increasing despite the facts about its effects and hazards to human health and this number is reaching one third of worldwide population who are 15 years of age or older.3
Smoking is more prevalent in Jordan compared to developed countries. The prevalence among men aged 18 yrs or more may be as high as 50%.11,12 In addition, male Jordanian smokers tend to be heavier smokers compared to smokers in developed countries.13
Cigarette smoke contains a large number of substances which are recognized as carcinogens and mutagens including radioactive polonium, cadmium, benzopyrene, dimethylbenzanthracene, dimethylnitrosamine, naphthalene and methnaphthalene. However, the toxicity of many of these constituents in cigarette smoke has not been well assessed for their effect on the function of human spermatozoa. Although the effect of cigarette smoking on sperm function was noticed a long time ago, the mechanism by which tobacco smoke affects sperms remains poorly understood.14 Thus, the impact of cigarette smoking on male fertility and sperm characteristics remains a highly controversial issue.15
Cigarette smoking may be associated with subfertility in males and may lead to a decrease in sperm concentration, lower sperm motility, and a reduced percentage of morphologically normal sperms.16-18 Many studies examined the effect of smoking on semen quality have been carried out worldwide.18-21 Some of these studies showed that cigarette smoking results in a reduction of sperm concentration, motility and normal morphology.18 Others have shown that cigarette smoking has a detrimental effect on sperm quality,20 but other study results were inconsistent and conflicting.21
This retrospective study was conducted to determine the effect of cigarette smoking on seminal fluid volume, sperm count, sperm concentration, motility and morphology, as well as viscosity and liquefaction time.
Methods
This retrospective study was conducted at the IVF laboratory, PRH, in which analysis of seminal fluid was done over a period of one year (August 2010 and July 2011) for male partners of couples experiencing infertility. The exclusion criteria included: a) males with abnormal genital examination (varicocele, undefended testicles, hydrocele, small sized testes); b) males with azospermia; c) Males with history of mumps; d) males with history of surgery for inguinal hernia, orchidopexy, or any scrotal surgery; e) males with chronic medical illness (diabetes mellitus, hypertension, thyroid disease, cancer patients, and tuberculosis; and f) males who quit smoking for a period of less than 6 months.
A total of 960 males were included in the study and were classified into two groups: group A-which was taken as the control group (non-smokers; n=564); and group B, which constituted the study group (smokers; n=396). In order to understand whether the number of cigarettes smoked per day affects the seminal fluid parameters, the smoker group was divided into two groups: those who smoke 20 or more cigarettes per day were termed as the heavy smoker group (n=266), while the non-heavy smoker group was mainly comprised of those who smoke less than 20 cigarettes per day (n=130).
Seminal fluid was collected via masturbation into sterile wide - mouth plastic container after 3-5 days of sexual abstinence in a room near the laboratory. Samples with partial spillage were rejected, one sample per male was included in the study. Prior to seminal fluid analysis, samples were allowed to liquefy at 37°C environment, followed by analysis at room temperature.
Routine semen analysis was carried out under light microscopy according to WHO guidelines.22 Semen analysis comprised of ejaculate volume, pH, viscosity, and sperm concentration (million/ml), which were determined using Makler Chamber. While motility was determined as percentage of motile spermatozoa, and morphology as percentage of normally-shaped spermatozoa. The volume of ejaculate was measured by aspirating the whole sample into a graduated pipette, the total sperm count was measured by multiplying the sperm concentration by the volume of ejaculate. For sperm morphology, slides were smeared with a small volume of semen, and allowed to dry at room air temperature, stained with eosin, then read for normal or abnormal sperms according to WHO criteria.22 Sperm motility was determined by evaluating 100 sperms per sample after placing a drop of semen on a slide covered with a cover slip and examined under light microscopy. Motility was defined according to World Health Organization as: type 1 (fast and straight forward motile sperm); type 2 (fast sluggish moving); type 3 (locally shaking sperm); and type 4 (immotile sperm).22
The normal seminal fluid reference points were according to WHO criteria sperm concentration (≥20 millions sperms/ml), morphology (≥30% sperms), motility (≥50% sperms with forward motility category a and b or ≥25% sperms with category A).22
Data were entered into the computer using statistical package for social sciences (SPSS) version 11.0. Data were checked for errors and were corrected. Data were expressed as mean ± SD. A p value of <0.05 was considered statistically significant. In order to understand whether the number of cigarettes smoked per day affects the seminal fluid parameters, we divided the smokers into two groups: those who smoke 20 or more cigarettes per day were termed as the heavy smoker group (n=266) and non-heavy smoker group for those who smoke less than 20 cigarettes per day (n=130).
Results
A total of 960 adult males were enrolled. Their age ranged between 21 and 76 years with a mean age of 35.45±6.27 (Mean±SD). Of these men, 564 were non smokers with a mean age of 36. 45±6.27. While 396 were smokers with a mean age of 34.35±4.25 (Mean ± SD). Table 1 shows the characteristics of the study sample, about 57.29% (n=550) of the study population were aged under 40 years, while body mass index indicated normal weights for 38.8% (n=154) of smokers and 40.6% (n=229) of non-smokers. On the other hand, Table 2 shows the values of seminal fluid parameters such as pH, semen volume, sperm concentration, sperm motility, sperm morphology, and leukocyte infiltration.
Table 1: The characteristics of the study sample.
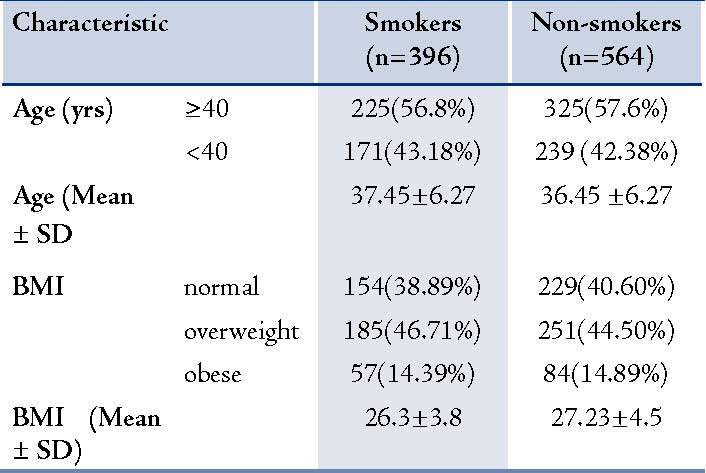
* BMI=Body mass index (kg.cm-2)
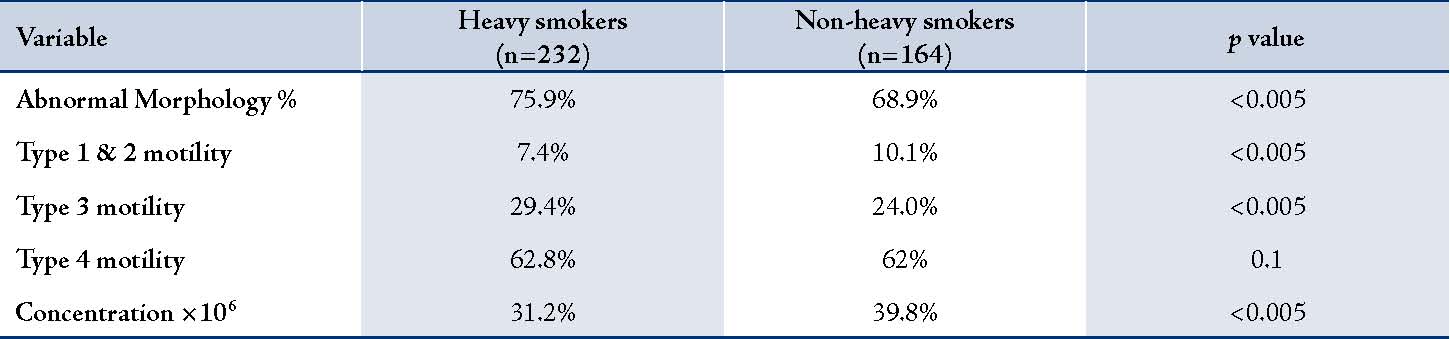
In both groups there was no significant difference between seminal fluid pH and sperm concentration; whereas the sperm morphology was significantly adversely affected by smoking. In terms of sperm motility; type 1 and 2 (progressive motile sperms) were significantly higher among non-smokers (p<0.005). On the other hand; type 4 (immotile sperm) were significantly higher among the smoker group, but the percentages of type 3 (locally shaking sperms) were comparable. While comparing the leukocyte infiltration in semen; it was noticed that leukocyte infiltration was higher among the semen of smokers, and especially among the heavy smokers. The smoking patients were classified according to the number of cigarettes smoked per day (heavy smokers ≥20 cigarettes per day) and non-heavy smokers (<20 cigarettes per day) as shown in Table 3. We noticed that there was a significant decrease in sperm concentration among the group of heavy smokers compared to non-heavy smoking group (p<0.005), and a significant increase in abnormal sperm forms and type 3 motile sperms (p<0.005) were also observed.
Table 2: Semen parameters of smoker and non smoker sample subjects (mean (SD).
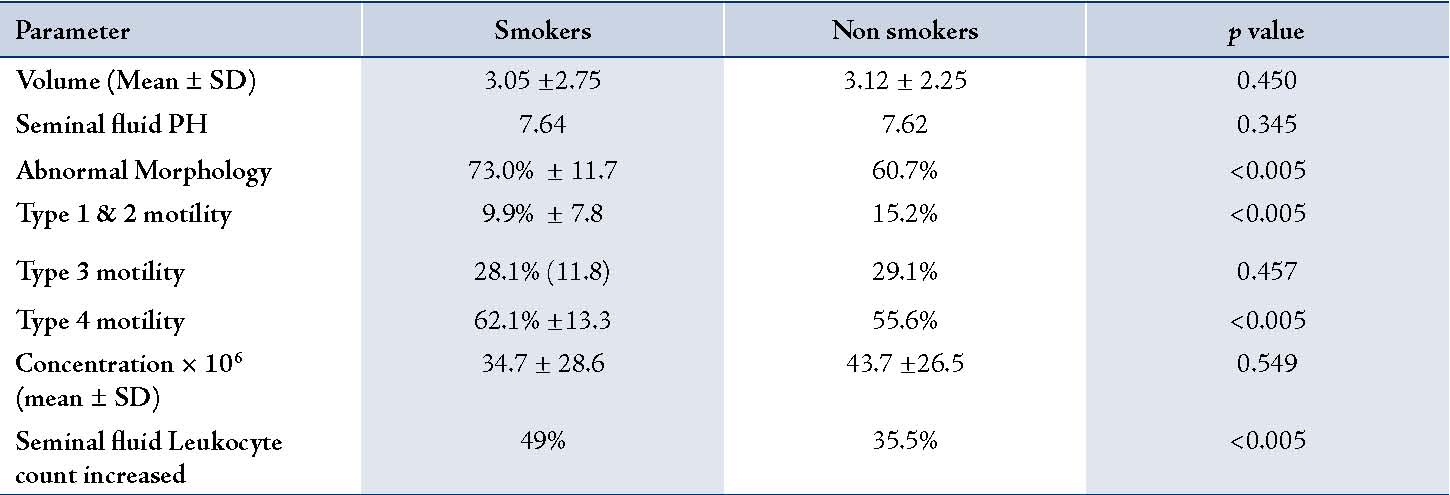
Table 3: Seminal fluid parameters among heavy smokers and non-heavy smokers.
Discussion
Many studies have examined the effect of cigarette smoking on male fertility and showed a negative effect on sperm production, motility and morphology.3-10 The percentage of smokers in our study of infertile men was 41.3% (n=396). The results of this study indicated that cigarette smoking affects sperm motility and results in decreased type 1 and 2 motility, while it increases type 4 mortility, and these results confirm the findings of ealier studies examining the relationship between cigarette smoking and sperm motility.21,23-27 However, our results were inconsistent with the results reported by Ozgur et al.28 who reported that there were no significant differences among smokers and non-smokers in the semen parameters and Collodel et al.9 who reported no significant difference in sperm motility between smokers and non-smokers. This study also showed that sperm morphology is negatively affected by cigarette smoking which confirms the results of Kunzle et al. and Collodel et al.9,20
The seminal fluid volume, sperm concentration and pH values were comparable between the two groups and this confirms the results of the study done by Trummer et al.7,29 who found that there were no significant differences in seminal fluid parameters between smokers and non smokers but the pH results were in contrast with the results of the study conducted by Kunzle et al. who found that there were significantly higher pH results among the smoker group.20
Leukocytes are the major source of reactive oxygen species in the ejaculate and elevated leukocytes may impair fertility by the formation of reactive oxygen species,30 which are in turn harmful to sperm DNA and membrane phospholipids because of oxidation and the effect of excessive oxidation may be detrimental.31 In our study, we found that there was a significant increase in seminal fluid leukocyte count which was also reported in previous studies.29,32 The exact mechanism of increased seminal leukocyte infiltration is not well understood and research on the possible explanations were suggested in previous studies, for example; tobacco metabolites may induce inflammatory reaction which result in the release of inflammatory mediators, which in turn result in the activation of leukocyte infiltration.33 Our study showed that there was a significant decrease in sperm concentration among the group of heavy smokers compared to the non-heavy smokers group (p<0.05), and a significant increase in abnormal sperm forms, as well as type 3 motile sperms (p<0.05). And comparing these results with Collodel et al. who found that sperm concentration was significantly lower among heavy smokers as opposed to non-heavy smokers, they also observed that sperm motility and morphology were not affected; however, their study group was small.
Conclusion
Cigarette smoking has a deleterious effect on some of the seminal fluid parameters (motility, morphology, and leukocyte count) which may in turn result in male subfertility. Therefore, we advise smokers to quit smoking and further studies are needed to verify whether quitting smoking improves male fertility.
Acknowledgements
The authors reported no conflict of interest and no funding was received for this work.
References
1. World Health Organization. Infections, pregnancies, and infertility: perspectives on prevention. Fertil Steril 1987 Jun;47(6):964-968.
2. Brugo-Olmedo S, Chillik C, Kopelman S. Definition and causes of infertility. Reprod Biomed Online 2001;2(1):41-53.
3. Zenzes MT. Smoking and reproduction: gene damage to human gametes and embryos. Hum Reprod Update 2000 Mar-Apr;6(2):122-131.
4. Windham GC, Swan SH, Fenster L. Parental cigarette smoking and the risk of spontaneous abortion. Am J Epidemiol 1992 Jun;135(12):1394-1403.
5. Pasqualotto FF, Lucon AM, Sobreiro BP, Pasqualotto EB, Arap S. Effects of medical therapy, alcohol, smoking, and endocrine disruptors on male infertility. Rev Hosp Clin Fac Med Sao Paulo 2004 Dec;59(6):375-382.
6. Pasqualotto FF, Sobreiro BP, Hallak J, Pasqualotto EB, Lucon AM; FÁBIO F et al. Cigarette smoking is related to a decrease in semen volume in a population of fertile men. BJU Int 2006 Feb;97(2):324-326.
7. Saleh RA, Agarwal A, Sharma RK, Nelson DR, Thomas AJ Jr. Effect of cigarette smoking on levels of seminal oxidative stress in infertile men: a prospective study. Fertil Steril 2002 Sep;78(3):491-499.
8. Zuying Chen et al. Impact of seasonal variation, age and smoking status on human semen parameters: The Massachusetts General Hospital experience. J Exp Clin Assist Reprod 2004;86:1743-1750.
9. G. COLLODEL et al. Semen Quality of Male Idiopathic Infertile Smokers and Nonsmokers: An Ultrastructural Study. J Andro l2010;31:108-113.
10. Augood C, Duckitt K, Templeton AA. Smoking and female infertility: a systematic review and meta-analysis. Hum Reprod 1998 Jun;13(6):1532-1539.
11. Haddad LG, Malak MZ. Smoking habits and attitudes towards smoking among university students in Jordan. Int J Nurs Stud 2002 Nov;39(8):793-802.
12. Ma’aya SP. Jordan: mass media campaign combating smoking requires serious commitment and not just words [Internet]. Geneva: WHO; 2004 [updated 2011; cited 2010 Dec 2]. Available from: http://www.who.int/ tobacco/training/success_stories/en/best_practices_jordan_media.pdf.
13. Amarin ZO. Obstetricians, gynecologists and the anti-smoking campaign: a national survey. Eur J Obstet Gynecol Reprod Biol 2005 Apr;119(2):156-160.
14. Osser S, Liedholm P, Ranstam J. Depressed semen quality: a study over two decades. Arch Androl 1984;12(1):113-116. abstract.
15. Arabi M, Moshtaghi H. Influence of cigarette smoking on spermatozoa via seminal plasma. Andrologia 2005 Aug;37(4):119-124.
16. Lewin A, Gonen O, Orvieto R, Schenker JG. Effect of smoking on concentration, motility and zona-free hamster test on human sperm. Arch Androl 1991 Jul-Aug;27(1):51-54. ABSTRACT.
17. Sofikitis N, Miyagawa I, Dimitriadis D, Zavos P, Sikka S, Hellstrom W. Effects of smoking on testicular function, semen quality and sperm fertilizing capacity. J Urol 1995 Sep;154(3):1030-1034.
18. Zinaman MJ, Brown CC, Selevan SG, Clegg ED. Semen quality and human fertility: a prospective study with healthy couples. J Androl 2000 Jan-Feb;21(1):145-153.
19. Ramlau-Hansen CH, Thulstrup AM, Aggerholm AS, Jensen MS, Toft G, Bonde JP. Is smoking a risk factor for decreased semen quality? A cross-sectional analysis. Hum Reprod 2007 Jan;22(1):188-196.
20. Künzle R, Mueller MD, Hänggi W, Birkhäuser MH, Drescher H, Bersinger NA. Semen quality of male smokers and nonsmokers in infertile couples. Fertil Steril 2003 Feb;79(2):287-291.
21. Chia SE, Lim ST, Tay SK, et al. Factors associated with male infertility: a case-control study of 218 infertile and 240 fertile men. Brit J Obstet Gynaecol (2000).107, 55-61
22. World Health Organization (WHO). Laboratory manual for the examination of human semen and sperm-cervical mucus interaction. 3rd ed. Cambridge, England: Cambridge University Press, 1992.
23. Vine MF, Tse CK, Hu P, Truong KY. Cigarette smoking and semen quality. Fertil Steril 1996 Apr;65(4):835-842.
24. Zavos PM, Correa JR, Antypas S, Zarmakoupis-Zavos PN, Zarmakoupis CN. Effects of seminal plasma from cigarette smokers on sperm viability and longevity. Fertil Steril 1998 Mar;69(3):425-429.
25. Wong WY, Thomas CM, Merkus HM, Zielhuis GA, Doesburg WH, Steegers-Theunissen RP. Cigarette smoking and the risk of male factor subfertility: minor association between cotinine in seminal plasma and semen morphology. Fertil Steril 2000 Nov;74(5):930-935.
26. Zhang JP, Meng QY, Wang Q, Zhang LJ, Mao YL, Sun ZX. Effect of smoking on semen quality of infertile men in Shandong, China. Asian J Androl 2000 Jun;2(2):143-146.
27. Wang SL, Wang XR, Chia SE, Shen HM, Song L, Xing HX, et al. A study on occupational exposure to petrochemicals and smoking on seminal quality. J Androl 2001 Jan-Feb;22(1):73-78.
28. Ozgur K, Isikoglu M, Seleker M, Donmez L. Semen quality of smoking and non-smoking men in infertile couples in a Turkish population. Arch Gynecol Obstet 2005 Feb;271(2):109-112.
29. Trummer H, Habermann H, Haas J, Pummer K. The impact of cigarette smoking on human semen parameters and hormones. Hum Reprod 2002 Jun;17(6):1554-1559.
30. Shen HM, Chia SE, Ong CN. Evaluation of oxidative DNA damage in human sperm and its association with male infertility. J Androl 1999 Nov-Dec;20(6):718-723.
31. Kim JG, Parthasarathy S. Oxidation and the spermatozoa. Semin Reprod Endocrinol 1998;16(4):235-239. abstract.
32. Close CE, Roberts PL, Berger RE. Cigarettes, alcohol and marijuana are related to pyospermia in infertile men. J Urol 1990 Oct;144(4):900-903. abstract.
33. Comhaire FH, Mahmoud AM, Depuydt CE, Zalata AA, Christophe AB. Mechanisms and effects of male genital tract infection on sperm quality and fertilizing potential: the andrologist’s viewpoint. Hum Reprod Update 1999 Sep-Oct;5(5):393-398.
|