Peptic ulcer perforation (PUP) is a life-threatening surgical condition that occurs in 2–20% of peptic ulcer disease patients and may increase mortality by up to 24–30%.1,2 Giant PUP is a perforation ≥ 2 cm, resulting in extensive tissue loss and severe tissue inflammation of the gastric or duodenal wall.3,4 These effects may preclude the ulcer from healing following surgical repair and lead to increased postoperative morbidities (such as bile leakage and intraabdominal collection) and mortality.5,6
Open surgical repair by simple interrupted sutures for closure of the perforation combined with a free omentum patch sutured on top of the repair (omentopexy) is a technique described by Graham that has become a standard treatment for PUP.7 However, omentopexy repair in giant perforated ulcers is associated with an increased risk of omental patch failure, resulting in higher overall morbidity than in smaller perforations.8
Antrectomy with vagotomy should be considered in managing giant ulcer perforations to secure the perforation and achieve maximum healing. Nevertheless, the effectiveness of this technique may be limited by the following features: (1) greater morbidity (50–60%) and mortality (10-fold increase) than the simple closure technique; (2) many surgeons practicing today has limited experience with the procedure; and (3) nearly all giant PUP patients are critically ill, putting them at a higher surgical risk.9–11
Karanjia first described the omental plugging technique in 1993, a simple procedure with a short operating time and learning curve. This technique appears to be appropriate in critically ill patients as an effective treatment for PUPs > 2 cm.12,13
Several studies report that omental plugging is associated with lower morbidity but has no benefit on mortality compared to the omentopexy technique. Still, these findings are limited since most such studies are non-randomized and include small sample sizes. We conducted a meta-analysis to compare postoperative outcomes, including mortality and postoperative complications, between omental plugging and the omentopexy technique in the management of giant PUP.
Methods
Electronic literature searches were performed on PubMed, Embase, Google Scholar, and the Cochrane database. The search terms ‘giant peptic ulcer’, ‘peptic ulcer perforation’, ‘omentopexy’, and ‘omental plug’ were used to identify all English-language studies published through to December 2020 all relevant studies. Meta-analysis was performed according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) 2020 statement, a guideline for reporting systematic reviews.14 The protocol of this meta-analysis was registered on PROSPERO (CRD42021258704).
The study inclusion criteria were as follows: (1) studies published in English; (2) PUP proven by the clinical and radiologic diagnosis; (3) clarification of giant PUP as gastric or duodenal ulcer perforation size ≥ 2 cm; (4) studies which compare outcomes of surgical treatment techniques between omental plug and omentopexy group; and (5) outcomes must evaluate perioperative mortality and postoperative complication rate.
Omental plug is defined as the pedicle of the greater omentum that was transfixed with 3–4 sutures that pass through the perforation inside the lumen. The sutures are tied to pull the omental pedicle into the lumen forming an effective plug for closure of the perforation site.15
Another omental plugging technique is described as the free edge of the greater omentum, which is transfixed by 1–0 or 2–0 rapid absorbable sutures to the tip of a nasogastric tube that passes through the perforation site. The tube is then withdrawn until 5–6 cm of the omentum occludes the perforation. An additional 5–6 interrupted stitches are taken between the omentum and serosa of the healthy duodenum/or stomach.
The omentopexy group is defined by the perforation site being repaired by three interrupted Lembert sutures with 2–0 polyglactin or silk using a patch of omentum pedicle to reinforce the suture line (Graham’s patch). This procedure was modified by passing the suture between the perforation’s edges and tying it to close the perforation, then introducing the pedicle of omentum between these sutures and tying them again with a pedicle of omentum between knots over the perforation (Modified Graham’s patch).7
The postoperative mortality rate is defined as a death that occurred during the 30-day postoperative period. Finally, the postoperative complication is an overall postoperative complication, wound infection, respiratory tract infection, intraabdominal collection, and bile leakage.
The exclusion criteria were as follows: (1) non-English language articles; (2) review articles or case reports; (3) studies involving pediatric patients (aged < 15 years); and (4) non-comparative studies. The Newcastle-Ottawa scale was used to assess the quality of the studies included in the meta-analysis, which evaluates case selection methods, research design to account for comparative variables, and methods for assessing outcomes. The maximum possible score is nine points which represents the highest methodological quality.16
The two reviewers independently extracted the following information from the selected studies: author names, country of origin, year of publication, study design, number of patients, patient characteristics, surgical treatment methods, and postoperative outcomes. Extracted data were cross-checked to reach a consensus and entered into a computerized spreadsheet for analysis.
Meta-analysis was performed using Review Manager software, version 5.4.1, which was provided by the Cochrane Collaboration (Nordic Cochrane Center, Cochrane Collaboration, Copenhagen, Denmark). Cochrane’s chi-square-based Q-statistic test was applied to assess between-study heterogeneity. An I2 statistic was used to test for heterogeneity between the included studies (p < 0.05 is considered for significant heterogeneity).
The patients’ postoperative mortality and complication rates were analyzed using the Mantel-Haenszel method to generate a pooled odds ratio (OR) with 95% CIs) to compare the mortality and postoperative complications between the omental plug and omentopexy groups. OR was considered statistically significant at the p < 0.05 level and the 95% CI did not include the value 1.
The fixed-effect model was adopted to calculate ORs. However, where significant evidence of heterogeneity was detected, the random-effected model is used to access a weighted average of the effects reported in different studies to calculate levels of association. Publication bias was assessed by visual examination of a funnel plot, while asymmetry was formally assessed using both Egger’s linear regression test and the rank correlation test (Begg’s test).
Results
The initial search identified 175 potential articles. After screening, eight articles (four prospective non-randomized studies, three prospective randomized studies, and one retrospective study) that matched the research criteria were deemed suitable for inclusion in the meta-analysis.17–24 The PRISMA diagram used in the search process is shown in Figure 1.

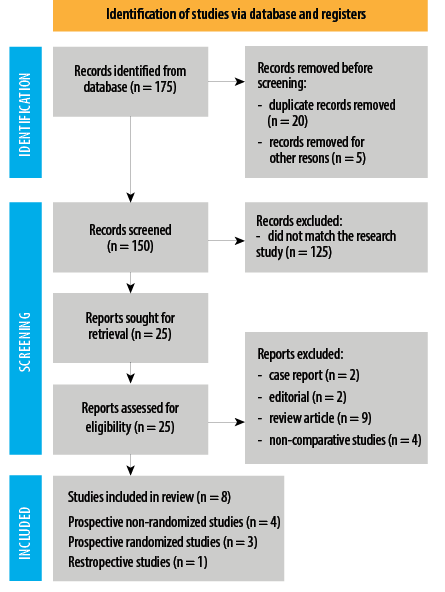 Figure 1: Selection process of studies for inclusion in the meta-analysis.
Figure 1: Selection process of studies for inclusion in the meta-analysis.
Table 1: Characteristics of the eight studies included in the meta-analysis regarding the association between omental plug and omentopexy with the postoperative outcomes.
|
Kumar et al,17
|
2020
|
India
|
Prospective non-randomized
|
15–80
|
12
|
Male = 10
Female = 2
|
- Clinical
- Laboratory
- Plain film abdomen
|
N/A
|
25:75
|
6:6
|
a, b, c, d, e, g, j, k
|
7
|
|
Sabhnani et al,18
|
2016
|
India
|
Prospective non-randomized
|
15–80
|
33
|
Male = 27
Female = 6
|
- Clinical
- Laboratory
- Plain film abdomen
|
42%
|
30:70
|
15:18
|
a, b, c, d, e, g, h, i
|
7
|
|
Mukhopadhyay et al,19
|
2011
|
India
|
Prospective non-randomized
|
33–73
|
23
|
N/A
|
- Clinical
- Laboratory
- Plain film abdomen
|
26%
|
N/A
|
10:13
|
a, c, d, f, g, h, i, j
|
6
|
|
Parihar et al,20
|
2016
|
India
|
Prospective non-randomized
|
20–80
|
30
|
Male = 28
Female = 2
|
- Clinical
- Plain film abdomen
|
N/A
|
N/A
|
15:15
|
a, b, c, g, h, i, j
|
6
|
|
Kumar et al,21
|
2020
|
India
|
Prospective randomized controlled study
|
20–67
|
60
|
Male = 49
Female = 11
|
- Clinical
- Laboratory
- Plain film abdomen
|
N/A
|
N/A
|
30:30
|
a, b, g, i
|
7
|
|
Gujar et al,22
|
2014
|
India
|
Retrospective study
|
49.78
(mean)
|
36
|
Male = 29
Female = 7
|
- Clinical
- Laboratory
- Plain film abdomen
|
58.4%
|
100% Duodenal ulcer
|
18:18
|
a, b, g, h, i, j
|
6
|
|
Datta et al,23
|
2015
|
India
|
Prospective randomized controlled study
|
26–57
|
73
|
Male = 73
|
- Clinical
- Laboratory
- Plain film abdomen
|
N/A
|
100% Duodenal ulcer
|
35:38
|
a, b, g, h, i
|
7
|
|
Jani et al,24
|
2006
|
India
|
Prospective randomized controlled study
|
16–66
|
100
|
Male = 89
Female = 11
|
- Clinical
- Laboratory
- Plain film abdomen
|
N/A
|
100% Duodenal ulcer
|
50:50
|
a, b, c, f, g, h, i, j
|
7
|
a: age; b: sex; c: fluid resuscitation; d: intravenous antibiotic; e: history of peptic ulcer; f: timing to surgery; g: postoperative complication; h: length of stay; i: mortality; j: comorbidities; N/A: not available.
The two reviewers showed 100% agreement with the final dataset. The pooled studies included 367 patients, which were used to investigate the association between the omental plug and omentopexy with the postoperative complication and mortality rate.
Omental plug was performed in 179 patients (48.8%), and omentopexy was performed in 188 patients (51.2%). The Newcastle-Ottawa scale found that all the studies included in the meta-analysis were moderate to good quality (6–7 stars). The characteristics of the eight included studies are shown in Table 1. The primary purpose of this study was to compare the postoperative mortality rate between the omental plug and omentopexy groups. Eight studies involving 367 patients reported the association between each surgical technique with mortality as an outcome.17–24 The overall mortality rate was 12.3% (45/367), in which the postoperative mortality in the omental plug and omentopexy groups were 6.7% (12/179) and 17.6% (33/188), respectively.
The pooled analysis demonstrated that the postoperative mortality rate in the omental plug group was significantly lower than in the omentopexy group (OR = 0.35, 95% CI: 0.17–0.69, p = 0.003). There was no significant heterogeneity between studies (I2 = 0%, p = 1.00). The pooled analysis also represents an absolute risk difference of 0.12 and a number need to treat of 8.3.
A forest plot displaying the association between omental plug and omentopexy with postoperative mortality is illustrated in Figure 2. No evidence of publication bias was observed by either Egger’s test (p = 0.052) or the rank correlation test (p = 0.216). Figure 3 presents a funnel plot of the meta-analysis with a symmetrical distribution.

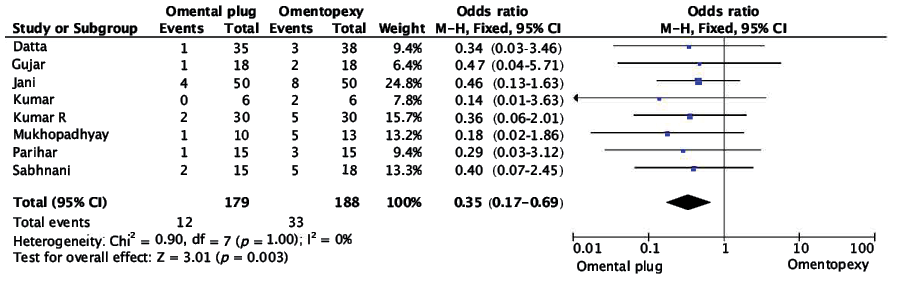 Figure 2: Forest plot of the association between omental plug and omentopexy with perioperative mortality.
Figure 2: Forest plot of the association between omental plug and omentopexy with perioperative mortality.
Eight studies reported an association between postoperative complications and surgical treatment techniques.17–24 The overall postoperative complication rate was 30.2% (54/179) and 69.8% (105/188) in the omental plug and omentopexy groups, respectively. The pool analysis demonstrates that the overall postoperative rate was significantly higher in the omentopexy group (OR = 0.29, 95% CI: 0.18–0.47, p < 0.0001). The pooled analysis represents an absolute risk difference of 0.26 and a number need to treat of 3.8 without evidence of heterogeneity between studies (I2 = 0%, p = 0.69). Evidence of publication bias was not observed by both Egger’s test (p = 0.276) and the rank correlation test (p = 0.322).
Wound infection occurred in 14.7% (19/129) of patients in the omental plug group compared to 21.0% (29/138) in the omentopexy group. The pooled analysis of seven studies17–23 demonstrated no significant difference in the wound infection rate between each surgical treatment group (OR = 0.66, 95% CI: 0.35–1.26, p = 0.21). The pooled analysis represented an absolute risk difference of 0.07, and a number need to treat of 14.3. There was no significant heterogeneity between studies (I2 = 0%, p = 0.94) and no evidence of publication bias was observed by both Egger’s test (p = 0.532) and the rank correlation test (p = 0.453).
The respiratory tract infection rate was 12.4% (16/129) in the omental plug group compared to 17.4% (24/138) in the omentopexy group. The pooled analysis of seven studies17–23 demonstrated no significant difference in the respiratory tract infection rate between each surgical treatment group (OR = 0.68, 95% CI: 0.34–1.36, p = 0.28). The pooled analysis represented an absolute risk difference of 0.05, and a number need to treat of 20. No evidence of heterogeneity (I2 = 0%, p = 1.00) or publication bias was observed in this analysis (Egger’s test [p = 0.336] and rank correlation test [p = 0.710]).
The pooled analysis from seven studies17–23 demonstrated that the incidence of the intraabdominal collection was not significantly different in both surgical treatment groups (6.2% and 9.4% in the omental plug and omentopexy group), OR = 0.68, 95% CI: 0.28–1.64, p = 0.39. The pooled analysis represented an absolute risk difference of 0.03, and number need to treat of 33.3.
There was no evidence of either heterogeneity (I2 = 0%, p = 0.96) or publication bias in this analysis (Egger’s test [p = 0.262] and rank correlation test [p = 0.176]).
The final analysis was conducted from seven studies17–19,21–24 to evaluate the association between the incidence of bile leakage and surgical treatment techniques. The pooled analysis demonstrated that the bile leakage rate in the omental plug group was significantly lower than the omentopexy group (1.8% vs. 15%), OR = 0.18, 95% CI: 0.07–0.46, p = 0.0003. The pooled analysis represented an absolute risk difference of 0.13, and a number need to treat of 7.7. There was also no evidence of heterogeneity (I2 = 0%, p = 0.89) and publication bias observed in this analysis (Egger’s test [p = 0.127] and rank correlation test [p = 0.881]). A forest plot displaying the association between omental plug and omentopexy with postoperative complication is illustrated in Figure 4.

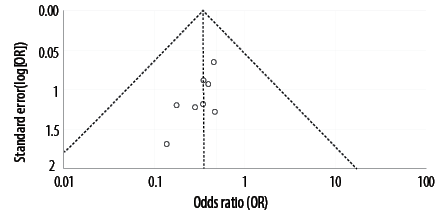 Figure 3: Funnel plot of the association between omental plug and omentopexy with perioperative mortality.
Figure 3: Funnel plot of the association between omental plug and omentopexy with perioperative mortality.

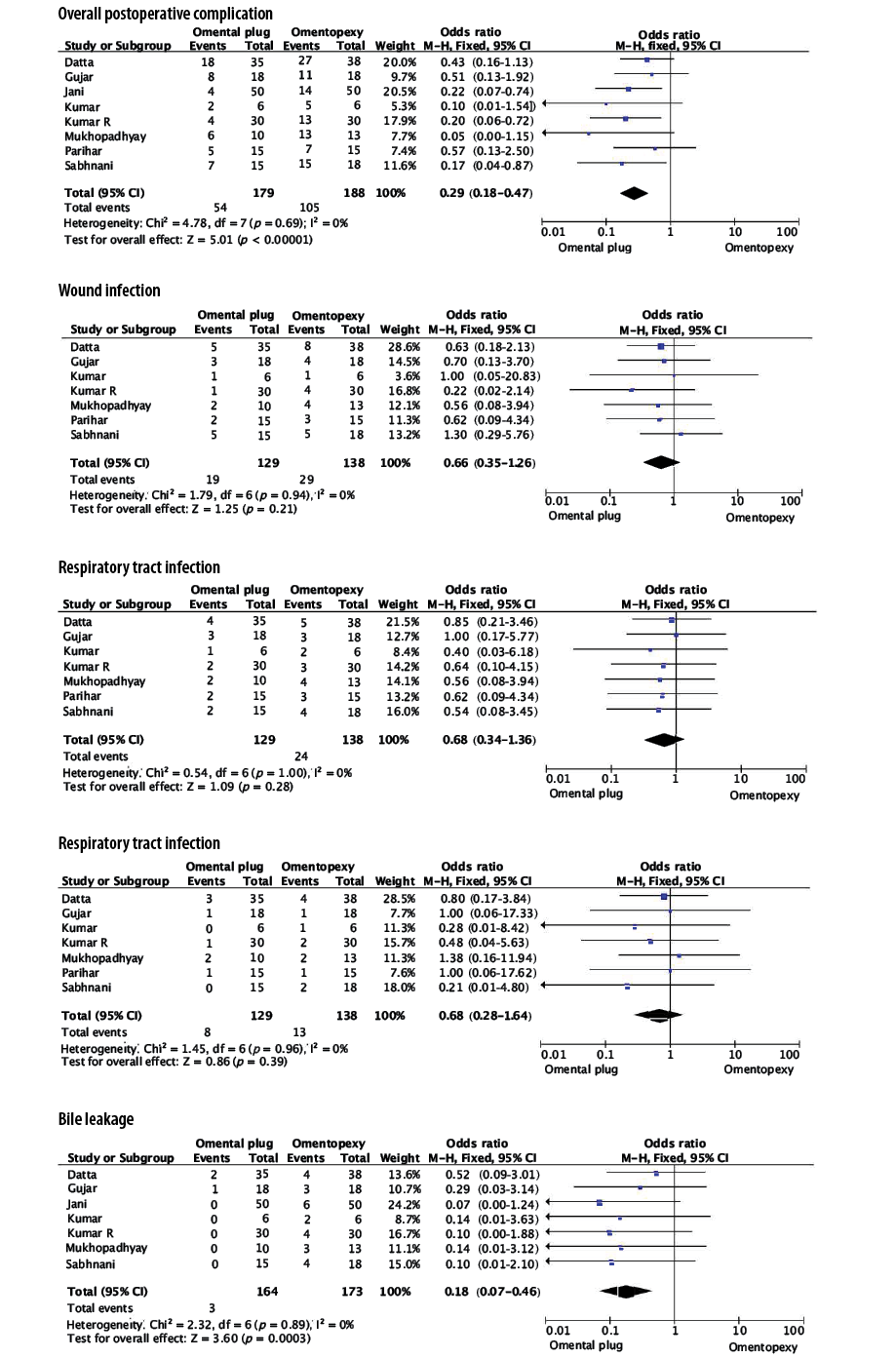 Figure 4: Forest plot of the association between omental plug and omentopexy with the perioperative complications.
Figure 4: Forest plot of the association between omental plug and omentopexy with the perioperative complications.
Discussion
The literature reports an incidence of giant peptic ulcers of about 14% and 2.4% for gastric and duodenal ulcers, which have a high risk of developing catastrophic perforation (3.2–9%).24,25 Giant perforations are difficult to repair due to severe tissue inflammation concomitant with a high intraluminal pressure that disrupts the suture line, causing bile leakage, generalized peritonitis, and bursting of the abdomen, resulting in 26.6–48.2% mortality rate.26,27
The omentum is an intraperitoneal organ with large adipose tissue that provides biological properties, including neovascularization, hemostasis, and tissue healing. Thus, omentum has been applied in gastrointestinal surgery to wrap around the sites of the gastroduodenal perforation to promote fibrosis and regeneration of the duodenal wall to prevent leakage.28,29
The incidence of omental flap failure for omentopexy in giant ulcer perforation is reported to be 12%.24 Thus, the omental plugging technique has been developed to improve surgical outcomes. This technique is simple and does not require a level of surgical expertise that may be unavailable in an emergency. The World Society of Emergency Surgery guideline for managing perforated and bleeding peptic ulcers suggested an omental plugging technique as a surgical option in the management of giant duodenal ulcer perforation.30
The pooled results indicate that omental plugging is associated with a significant reduction in the overall complications (30.2% vs. 69.8%). Subgroup analysis of the postoperative complication outcome was conducted to clarify this technique’s effectiveness, and it was established that the omental plugging group had a lower incidence of bile leakage than the omentopexy group (1.8% vs. 15%).
The omentopexy group seemed to have a greater incidence of respiratory tract infection, wound infection, and intraabdominal collection. However, no significant difference in surgical site infection rates was found between the surgical technique groups. The pooled analysis in this study revealed that the incidence of surgical site infection was < 20%, which could be attributed to the fact that all of the patients received a broad-spectrum antibiotic before surgery, and almost all of the patients would have emergency surgery within 24 hours of the onset of the symptom. These findings correspond with the results of several previous studies.19,21,31 Another study reported that respiratory tract and wound infections were the most common postoperative problems, occurring in > 24% of patients.32
The main purpose of the meta-analysis was to investigate the association between mortality and surgical techniques. Because of leakage, the pancreatic enzyme and bile initiate the autodigestion process, a consequence of uncontrolled intraabdominal infection and septicemia, leading to patient mortality.33,34 The omental plugging group had a significantly lower risk of postoperative mortality (6.7% vs. 17.6%), which could be attributable to the fact that the omental plug was demonstrated to benefit occlusion and to seal the perforated site, resulting in a lower rate of bile leakage.
Our results are somewhat limited due to the risk of publication bias. For instance, most included studies were retrospective or non-randomized studies and were limited to English language publications. Additionally, most of the patients in this analysis were from Asian countries and did not represent a global clinicopathological association between postoperative outcomes and surgical techniques.
Even though all of the research analyzed was conducted in India, statistical analysis and funnel plot distribution did not reveal significant evidence of publication bias. The fact that the major etiologies of PUP are similar worldwide due to the high prevalence of H. pylori infection and the use of non-steroidal anti-inflammatory drugs may help clarify this finding.35,36
Additionally, the results are somewhat complicated by the risk heterogeneity attributed to differences in the time from diagnosis to operation, which vary from one hour to > 48 hours. Also, patients in some studies presented with septic shock, and four of the included studies only reported outcomes for perforated duodenal ulcers. Yet the evidence of heterogeneity between studies was not observed in this meta-analysis.
Given that this research focused exclusively on studies where omental plugging or omentopexy was performed with the open surgical technique, it may be beneficial for future studies to examine the association between minimal access surgery in combination with the laparoscopic and endoscopic assisted in the management of giant peptic ulcer by omental plugging technique,37 which could help improve treatment outcomes.
Conclusion
Giant perforation is a catastrophic complication of peptic ulcer disease that is difficult to repair and associated with substantial morbidity and mortality. Omental plugging is associated with fewer overall surgical complications and bile leakage rates than the omentopexy technique, which results in improved patient survival. This procedure is a safe surgical treatment option for PUPs > 2 cm.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
reference
- 1. Bertleff MJ, Lange JF. Perforated peptic ulcer disease: a review of history and treatment. Dig Surg 2010 Aug;27(3):161-169.
- 2. Wang A, Yerxa J, Agarwal S, Turner MC, Schroder V, Youngwirth LM, et al. Surgical management of peptic ulcer disease. Curr Probl Surg 2020 Feb;57(2):100728.
- 3. Feliciano DV, Bitondo CG, Burch JM, Mattox KL, Jordan GL Jr, DeBakey ME. Emergency management of perforated peptic ulcers in the elderly patient. Am J Surg 1984 Dec;148(6):764-767.
- 4. Hennessy E. Perforated peptic ulcer: mortality and morbidity in 603 cases. Aust N Z J Surg 1969 Feb;38(3):243-252.
- 5. Karanjia ND, Shanahan DJ, Knight MJ. Omental patching of a large perforated duodenal ulcer: a new method. Br J Surg 1993 Jan;80(1):65.
- 6. Chaudhary A, Bose SM, Gupta NM, Wig JD, Khanna SK. Giant perforations of duodenal ulcer. Indian J Gastroenterol 1991 Jan;10(1):14-15.
- 7. Graham RR. The treatment of perforated duodenal ulcers. Surg Gynecol Obstet 1937;64:235-238.
- 8. Gupta S, Kaushik R, Sharma R, Attri A. The management of large perforations of duodenal ulcers. BMC Surg 2005;5:15.
- 9. Sachdeva AK, Zaren HA, Sigel B. Surgical treatment of peptic ulcer disease. Med Clin North Am 1991 Jul;75(4):999-1012.
- 10. Hill AG. Management of perforated duodenal ulcer. In: Holzheimer RG, Mannick JA, editors. Surgical treatment: evidence-based and problem-oriented. Munich: Zuckschwerdt; 2001 [cited 2021 April 1]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK6926/.
- 11. Harbison SP, Dempsey DT. Peptic ulcer disease. Curr Probl Surg 2005 Jun;42(6):346-454.
- 12. Karanjia ND, Shanahan DJ, Knight MJ. Omental patching of a large perforated duodenal ulcer: a new method. Br J Surg 1993 Jan;80(1):65.
- 13. Raj BR, Subbu K, Manoharan G. Omental plug closure of large duodenal defects–an experimental study. Trop Gastroenterol 1997 Oct-Dec;18(4):180-182.
- 14. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg 2021 ;88:105906.
- 15. Sharma D, Saxena A, Rahman H, Raina VK, Kapoor JP. ‘Free omental plug’: a nostalgic look at an old and dependable technique for giant peptic perforations. Dig Surg 2000;17(3):216-218.
- 16. Wells G, Shea B, O’Connell D, Peterson J, Welth V, Losos M, et al. The Newcastle- Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses, Ottawa Health Research Institute, Ottawa (ON); 2010.
- 17. Kumar R, Kiran S, Hariaudh S. Giant peptic ulcer perforation- omentopexy versus omental plugging: a comparative study. Int Surg J 2020;7(3):787-790.
- 18. Sabhnani G, Tomar S. Giant peptic ulcer perforation: omentopexy versus omental plugging - a study. IAIM 2016;3(11):78-82.
- 19. Mukhopadhyay M, Banerjee C, Sarkar S, Roy D, Rahman QM. Comparative study between omentopexy and omental plugging in treatment of giant peptic perforation. Indian J Surg 2011 Oct;73(5):341-345.
- 20. Parihar S, Mathur PN, Joshi CP. Evaluation of large duodenal ulcer perforation with special reference to omentopexy and omental plugging. Int Surg J 2016;3(3):1229-1233.
- 21. Kumar R, Walia JS, Attri A, Singh S, Goyal S. Closure of peptic ulcer perforation by Grahm’s patch with omentopexy versus plugging with omentopexy. International Journal of Surgery and Medicine 2020;6(6):1-5.
- 22. Gujar N, Garag SP, Mudhol SA, Karnul AA, Sachin S. Comparative study between omentopexy and omental plugging for giant duodenal ulcer perforation. Int J Curr Res 2014;6(5):6852-6855.
- 23. Datta PK, Das AK, Mondal D. A comparative study between omentopexy and omental plugging in treatment of duodenal ulcer perforation. J Evol Med Dent Sci 2015;4(87):15153-15158.
- 24. Jani K, Saxena AK, Vaghasia R. Omental plugging for large-sized duodenal peptic perforations: a prospective randomized study of 100 patients. South Med J 2006 May;99(5):467-471.
- 25. Csendes A, Becker P, Valenzuela J, Braghetto I, Csendes P. [Clinical characteristics of patients with multiple or giant peptic ulcers]. Rev Med Chil 1991 Jan;119(1):38-44.
- 26. Hussain Z, Malik SM. Surgical outcome of large and giant duodenal ulcers perforations. JK Science 2015;17(3):131-134.
- 27. Maghsoudi H, Ghaffari A. Generalized peritonitis requiring re-operation after leakage of omental patch repair of perforated peptic ulcer. Saudi J Gastroenterol 2011 Mar-Apr;17(2):124-128.
- 28. Di Nicola V. Omentum a powerful biological source in regenerative surgery. Regen Ther 2019 Aug;11:182-191.
- 29. Madiba TE, Nair R, Mulaudzi TV, Thomson SR. Perforated gastric ulcer–reappraisal of surgical options. S Afr J Surg 2005 Aug;43(3):58-60.
- 30. Tarasconi A, Coccolini F, Biffl WL, Tomasoni M, Ansaloni L, Picetti E, et al. Perforated and bleeding peptic ulcer: WSES guidelines. World J Emerg Surg 2020 Jan;15:3.
- 31. Mondal D, Mukherjee A. A randomized comparative study between omentopexy and omental plugging in treatment of duodenal perforation. Int Surg J 2019;6(10):3662-3666.
- 32. Hastings N, MacHida R. Perforated peptic ulcer: results after simple surgical closure. Am J Surg 1961 Aug;102:136-142.
- 33. Walley BD, Goco I. Duodenal patch grafting. Am J Surg 1980 Nov;140(5):706-708.
- 34. Testini M, Portincasa P, Piccinni G, Lissidini G, Pellegrini F, Greco L. Significant factors associated with fatal outcome in emergency open surgery for perforated peptic ulcer. World J Gastroenterol 2003 Oct;9(10):2338-2340.
- 35. Al-Saeed A. Gastrointestinal and cardiovascular risk of nonsteroidal anti-inflammatory drugs. Oman Med J 2011 Nov;26(6):385-391.
- 36. Wang A, Yerxa J, Agarwal S, Turner MC, Schroder V, Youngwirth LM, et al. Surgical management of peptic ulcer disease. Curr Probl Surg 2020 Feb;57(2):100728.
- 37. Pescatore P, Halkic N, Calmes JM, Blum A, Gillet M. Combined laparoscopic-endoscopic method using an omental plug for therapy of gastroduodenal ulcer perforation. Gastrointest Endosc 1998 Oct;48(4):411-414.