A 15-year-old boy presented with a painless swelling at the back of his neck for the last two years that progressively increased in size. He denied a history of fever, trauma, or tuberculosis. Local examination revealed a hard, non-tender, globular mass in the right posterior triangle of the neck, deep to the trapezius muscle [Figure 1, a and b]. There was no cervical lymphadenopathy or neurological deficit. All the movements of the neck were normal. Antero-posterior and lateral X-rays of the cervical spine showed a soft tissue mass in the neck with specks of calcification within [Figure 1, c and d]. A computed tomography (CT) scan of the neck revealed the presence of a well-circumscribed, round to oval, predominantly fat attenuation lesion seen in the intermuscular plane of the right cervical paraspinal muscles. Multiple ossified trabeculae were seen scattered within the lesion, predominantly along the periphery. The cervical spine was normal. The vertebral, carotid, and jugular vessels were seen away from the mass [Figure 1, e and f].

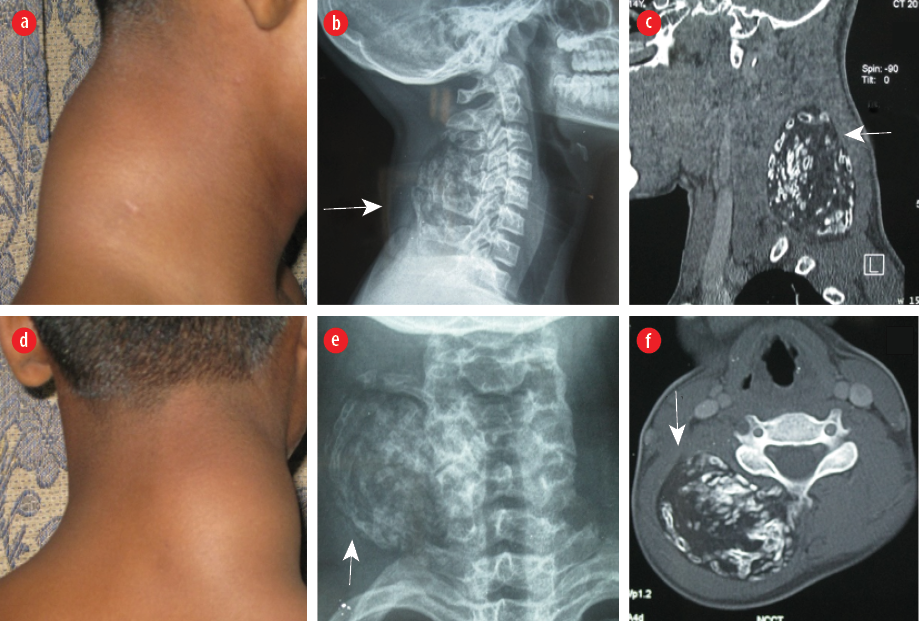 Figure 1: Clinical photograph of a bony hard globular swelling on the nape of the neck (a) side and (b) back view. X-ray of the neck shows peripheral calcifications within a soft tissue mass, marked with solid white arrows, (c) side, and (d) back view. Contrast-enhanced computed tomography sections show an intermuscular predominantly fat attenuation lesion with multiple ossified trabeculae, (e) sagittal and (f) axial plane.
Figure 1: Clinical photograph of a bony hard globular swelling on the nape of the neck (a) side and (b) back view. X-ray of the neck shows peripheral calcifications within a soft tissue mass, marked with solid white arrows, (c) side, and (d) back view. Contrast-enhanced computed tomography sections show an intermuscular predominantly fat attenuation lesion with multiple ossified trabeculae, (e) sagittal and (f) axial plane.
Question
What is the most likely diagnosis?
a. Osteochondroma.
b. Ossifying lipoma.
c. Teratoma.
d. Myositis ossificans.
Answer
b. Ossifying lipoma.
The patient underwent excision of the mass. No disease recurrence was detected on regular surveillance two years post-surgery.
Discussion
Core-cut biopsy suggested the diagnosis of an ossifying lipoma, which was confirmed on histopathological examination after complete excision. Ossifying lipoma is a benign tumor of mesenchymal origin, containing foci of ossification, usually found close to the periosteum of long bones or the spine (parosteal).1 It is a rare variant of the simple benign lipoma that undergoes osseous metaplasia.2 It is usually solitary and may also be intraosseous or intramuscular.2
The pathogenesis of ossifying lipoma has been theorized to be due to repetitive microtrauma, metabolic changes, and ischemia which lead to metaplasia and the development of the existing tissue into osteoblasts.3 The role of transforming growth factor and the presence of certain chromosomal translocations have also been suggested.4
It is a slow-growing, painless mass in the extremities, or head and neck. The most frequently reported sites of ossifying lipomas are the thigh, close to the femur or the forearm, adjacent to the radius. However, they are also found close to the tibia, humerus, scapula, clavicle, ribs, pelvis, metacarpals, metatarsals, mandible, and skull, as well as the spine, which is less common.2
Imaging features of ossifying lipomas are often pathognomonic. X-rays show calcific foci in the soft tissue mass. On CT scan, the ossifying lipomas are well defined and homogeneous, having identical tissue attenuation with the surrounding normal fat with surrounding layers of calcification. Magnetic resonance imaging (MRI) features of ossifying lipoma include signal intensity identical to that of subcutaneous fat in all pulse sequences, including fat suppression images, with few low signal intensity strands on T1-weighted images.2
Once the plain radiograph shows calcification or ossification, a differential diagnosis of several soft tissue tumors like osteochondroma, lipoma with tumoral calcinosis, myositis ossificans, and teratomas, extraskeletal osteosarcoma may need to be considered.5 Rhabdomyosarcoma, synovial sarcoma, and malignant fibrous histiocytoma may also become calcified. Linear and spiculated calcification and amorphous central calcification are seen in osteosarcomas.5 Stippled and curvilinear calcifications are usually seen in chondroma and chondrosarcoma, which are cartilaginous tumors.5 Peripheral calcification is seen in myositis ossificans and ossifying fibromyxoid tumors.5 A hypointense osseous rim along with other features such as trabeculae, dense fibrosis, and central adipose tissue on MRI is typical of myositis ossificans.5 A well-defined geometric hypodense mass with peripheral calcification in the earlier phases and dense calcification in mature lesions are seen on CT.5 However, it may still be difficult to differentiate an ossifying lipoma based only on imaging. Other differential diagnoses include paraspinal neurogenic tumors such as schwannomas and neurofibromas. Schwannoma appears heterogeneous on imaging, while neurofibroma appears homogeneous or shows a target sign but usually does not have calcification.6 Diffusion-weighted MRI and dynamic contrast enhancement can help in their differentiation.7
The treatment of choice is excision, as a definitive diagnosis can only be made on histopathological examination. Histopathological examination clinches the diagnosis of ossifying lipoma with the appearance of diffuse, mature ossification within fatty tissue. Recurrence after complete excision of the mass has not been reported in the literature.
references
- 1. Guirro P, Saló G, Molina A, Lladó A, Puig-Verdié L, Ramírez-Valencia M. Cervical paravertebral osteolipoma: case report and literature review. Asian Spine J 2015 Apr;9(2):290-294.
- 2. Saksobhavivat N, Jaovisidha S, Sirikulchayanonta V, Nartthanarung A. Parosteal ossifying lipoma of the fibula: a case report with contrast-enhanced MR study and a review of the literature. Singapore Med J 2012 Aug;53(8):e172-e175.
- 3. Yang JS, Kang SH, Cho YJ, Choi HJ. Pure intramuscular osteolipoma. J Korean Neurosurg Soc 2013 Dec;54(6):518-520.
- 4. Myint ZW, Chow RD, Wang L, Chou PM. Ossifying parosteal lipoma of the thoracic spine: a case report and review of literature. J Community Hosp Intern Med Perspect 2015 Feb;5(1):26013.
- 5. Razek AA, Huang BY. Soft tissue tumors of the head and neck: imaging-based review of the WHO classification. Radiographics 2011 Nov-Dec;31(7):1923-1954.
- 6. Abdel Razek AA, Gamaleldin OA, Elsebaie NA. Peripheral nerve sheath tumors of head and neck: imaging-based review of World Health Organization classification. J Comput Assist Tomogr 2020 Nov/Dec;44(6):928-940.
- 7. Razek AA, Ashmalla GA. Assessment of paraspinal neurogenic tumors with diffusion-weighted MR imaging. Eur Spine J 2018 Apr;27(4):841-846.