Acute myeloid leukemia (AML) is the second most common type of acute leukemia in pediatric population. It is characterized by the proliferation of immature myeloid cells and the consequent bone marrow failure. AML patients can develop extramedullary lesions, most commonly in the meninges, testicles, and orbits. Proptosis as an initial presenting sign of AML is very rare compared to various other signs and symptoms these patients can develop. We report a case of AML in a six-year-old girl in whom the disease primarily presented as unilateral proptosis.
Case Report
A six-year-old girl was referred from the local health center to our ophthalmology clinic after being investigated for hyperthyroidism, for evaluation of progressive, painless proptosis of the right eye for a one-week duration. She looked pale and her parents reported easy fatigability, despite having no loss of appetite or recent weight change. There was no history of recent or recurrent fever, night sweats, symptoms of upper respiratory tract infection, abdominal pain, changes in bowel habits, urinary symptoms, abnormal movements, loss of consciousness, skin rashes, or bruises. The significant events in her medical history were eczema, allergic rhinitis, and chronic otitis media with effusion causing conductive hearing impairment.
.png)
.png) Figure 1: Photo of the patient showing proptosis of the right eye.
Figure 1: Photo of the patient showing proptosis of the right eye.
.png)
.png) Figure 2: Bone marrow aspiration slide
Figure 2: Bone marrow aspiration slide
showing myeloblasts.

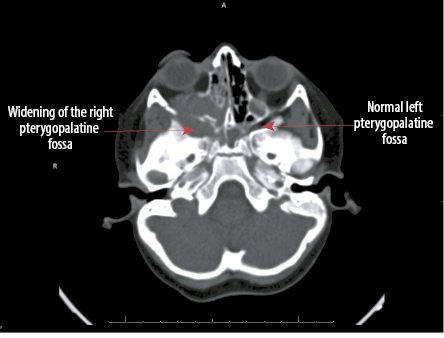 Figure 3: Cranial CT scan of the patient showing widening of the right pterygopalatine fossa.
Figure 3: Cranial CT scan of the patient showing widening of the right pterygopalatine fossa.
General physical examination revealed a tired, pale-looking child, but no organomegaly or lymphadenopathy was detected. Ophthalmic evaluation revealed visual acuity of 6/6 in each eye. Proptosis in the right eye had mild limitation of abduction [Figure 1]. There was no periocular discoloration. Both pupils reacted normally to light. Color vision and visual field could not assess due to poor cooperation. Anterior segment examination was unremarkable. Ophthalmoscopy revealed hyperemic discs in both eyes. The rest of the fundus examination was normal.
The child was admitted for further evaluation. Initial blood investigation revealed hemoglobin of 6.5 g/dL (11.0–14.5), platelet count of 28 × 109/L (150–450), and white cell counts of 21 × 109/L (2.4–9.5).
Peripheral blood smear showed normocytic, normochromic red cells with few elliptocytes, and numerous pleomorphic, medium to large circulating blast cells, some with bilobed nucleus, and fine granulation. Neutrophils were dysplastic and shifted to the left. Auer rods were not seen [Figure 2]. Uric acid, renal and liver function tests, bone profile, and cerebrospinal fluid analysis were all reported to be normal. Lactate dehydrogenase was 500 U/L (120–500). Chromosomal analysis by fluorescence in situ hybridization showed inversion 16 which is a favorable cytogenetic abnormality.
Ultrasound abdomen, electrocardiogram, and echocardiography were normal. A computed tomographic (CT) scan of the brain and orbits revealed features of an infiltrative process involving the right maxillary and ethmoid sinuses with extension to the infratemporal fossa inferiorly and into the orbit with possible intraoral and intracranial extension [Figure 3]. The visual evoked potential test yielded normal response.
Examination of bone marrow aspirate revealed replacement of trilineage hematopoiesis with abnormal blast population with features matching those seen in the peripheral blood smear. Residual granulocytes were dysplastic and showed hypogranulation and hypolobation. Eosinophils were prominent. Residual erythropoiesis was normoblastic. Hemophagocytic activity was noted in the background [Figure 2].
A diagnosis of AML was made based on above findings. The patient received packed red blood cells and platelet transfusion to correct the significant anemia and thrombocytopenia and then was started on the AAML 1031 standard chemotherapy arm treatment protocol in April 2019 and completed four cycles of the protocol by December 2019. Mutation of the FLT3-ITD gene is found in approximately 10% of pediatric AML. Poor outcome is associated with higher initial total leukocytic counts and higher induction failure rates.1 Our patient has an initial white blood cell count of < 50 × 109/L and she went into complete remission after course 1 of chemotherapy.
The patient tolerated the chemotherapy cycles with no major side effects except for three episodes of febrile neutropenia. These were managed with intravenous tazobactam/piperacillin. Even though her blood cultures did not indicate any infection during severe neutropenia episodes, she was given antifungal prophylaxis with voriconazole.
Discussion
AML can present with ocular symptoms due to direct leukemic infiltration of ocular tissue. At the time of diagnosis of acute leukemia, half of the children demonstrate ocular involvement, most commonly due to alterations of hematologic parameters (low hemoglobin, low platelets, and hyperviscosity states) which present as vitreous, retinal, or choroidal hemorrhages.2
Ophthalmic manifestations of leukemia can be extraocular and intraocular. Among the extraocular manifestations, subconjunctival hemorrhages, conjunctival chemosis, lid edema, and extraocular muscle restriction are the most common presentations in descending order.3
Orbital involvement as an initial manifestation of AML is uncommon. Most cases present with unilateral proptosis, though some may have bilateral orbital involvement as an initial manifestation.4 Proptosis occurs mainly because of the accumulation of orbital leukemic infiltrates in the orbit and the orbital muscles, venous blockage, or retrobulbar hemorrhage. Proptosis secondary to diffuse infiltration of the lacrimal gland and infiltration of individual extraocular muscles has also been reported.5
Proptosis might occur due to granulocytic sarcoma which is an extramedullary accumulation of infiltrating leukemic cells. Granulocytic sarcoma is a rare manifestation of AML seen in approximately 3% of cases. The suggested theory behind granulocytic sarcoma is that the cancerous cells originate in the bone marrow and then migrate through the Haversian canals to collect in the subperiosteal and form soft-tissue masses, most commonly in the skull, orbits, paranasal sinuses, sacrum, spine, sternum, and ribs. However, granulocytic sarcoma presenting as an orbital mass in AML is very rare.6
In pediatric patients, the differential diagnosis of acute proptosis includes a wide range of disorders including orbital dermoids, orbital cellulitis, orbital hemangiomas, lymphangiomas, orbital varices, those triggered by inflammation (such as thyroid eye disease and nonspecific orbital inflammation), and other neoplastic tumors like retinoblastoma, rhabdomyosarcoma, metastatic neuroblastoma, and Langerhans cell histiocytosis. Among these various causes, proptosis due to orbital myeloid granulocytic sarcoma appears to be such a rare entity accounting for only one in 250 cases in previous reports.7
The presence of orbital involvement is associated with a higher frequency of bone marrow relapses and central nervous system involvement, leading to lower survival rates compared to AML patients without orbital lesions.8
As we write this report, eleven months have elapsed since our patient’s chemotherapy protocol was completed. Since she has favorable cytogenetics and no matched donor, she was not given a bone marrow transplant. No major complications have been noted on follow-ups.
Conclusion
AML should be kept in mind as differential diagnosis when presented with rapidly growing unilateral or bilateral proptosis in a child. If AML is suspected, radiological imaging, peripheral blood smear, and subsequent bone marrow biopsy should be performed.
Disclosures
The authors declared no conflicts of interest. Written consent was obtained from the parents of the child to publish her photograph for research purposes.
references
- 1. Moritake H, Tanaka S, Miyamura T, Nakayama H, Shiba N, Shimada A, et al. The outcomes of relapsed acute myeloid leukemia in children: results from the Japanese Pediatric Leukemia/Lymphoma Study Group AML-05R study. Pediatr Blood Cancer 2021 Jan;68(1):e28736.
- 2. abu el-Asrar AM, al-Momen AK, Kangave D, Harakati MS, Ajarim DS. Correlation of fundus lesions and hematologic findings in leukemic retinopathy. Eur J Ophthalmol 1996 Apr-Jun;6(2):167-172.
- 3. Dhasmana R, Prakash A, Gupta N, Verma SK. Ocular manifestations in leukemia and myeloproliferative disorders and their association with hematological parameters. Ann Afr Med 2016 Jul-Sep;15(3):97-103.
- 4. Rajput D, Naval R, Yadav K, Tungaria A, Behari S. Bilateral proptosis and bitemporal swelling: a rare manifestation of acute myeloid leukemia. J Pediatr Neurosci 2010 Jan;5(1):68-71.
- 5. Consul BN, Kulshrestha OP, Mehrotra AS. Bilateral proptosis in acute myeloid leukaemia. Br J Ophthalmol 1967 Jan;51(1):65-67.
- 6. Stockl FA, Dolmetsch AM, Saornil MA, Font RL, Burnier MN Jr. Orbital granulocytic sarcoma. Br J Ophthalmol 1997 Dec;81(12):1084-1088.
- 7. Shields JA, Bakewell B, Augsburger JJ, Donoso LA, Bernardino V. Space-occupying orbital masses in children. A review of 250 consecutive biopsies. Ophthalmology 1986 Mar;93(3):379-384.
- 8. V Russo, I U Scott, G Querques, A Stella, A Barone, N Delle Noci. Orbital and ocular manifestations of acute childhood leukemia: clinical and statistical analysis of 180 patients. Eur J Ophthalmol 2008;18(4):619-623.