Surgically induced necrotizing scleritis (SINS) is a rare but serious complication of ocular surgeries. It presents as a localized area of scleral inflammation next to the site of previous surgical incisions.1,2 It may occur at variable onset following different anterior or posterior segment surgeries including pterygium, trabeculectomy, cataract extraction penetrating keratoplasty, and vitrectomy.1,2 The use of mitomycin C, adjunctive irradiation, or excessive cauterization during surgery can lead to scleral necrosis and melting. Therefore, it is essential to exclude these etiologies before confirming the diagnosis.3–5 Noticeably, scleritis develops more frequently after multiple surgical procedures rather than a single surgery; this supports the suggestion that tissue injury releases or alters an antigen leading to a hypersensitivity reaction.6
The development of necrotizing scleritis following ocular surgeries can be the first manifestation of systemic autoimmune vasculitis. Thus, early diagnosis and management of necrotizing scleritis and the underlying etiology may improve ocular and systemic prognoses.7
Case report
A 49-year-old male patient, not known to have any medical diseases, presented with bilateral pterygium for five years, asking for cosmetic excision. Nothing was remarkable in the history, and the ophthalmic examination was within normal limits apart from bilateral pterygium involving up to 4 mm on both corneas nasally (type II pterygium). He underwent bilateral pterygium excision with conjunctival autografts in the same procedure under topical anesthesia (oxybuprocaine hydrochloride 0.4% eye drops). Two free conjunctival grafts were measured properly and harvested from the superotemporal bulbar conjunctiva of the same eye without underlying tenon to cover the exposed sclera in each eye. A gentle cauterization with bipolar forceps was applied without mitomycin C or adjunctive radiation, and 8-0 vicryl absorbable sutures were used to stabilize the grafts in both eyes. The next day, the patient was prescribed combined tobramycin/dexamethasone eye ointment qid.
Two weeks later, the patient complained of pain, blurry vision, and hypersensitivity to light in both eyes. His examination revealed a best-corrected visual acuity (BCVA) of 20/32 in both eyes (baseline BCVA was 20/20 in both eyes) along with bilateral ischemic and melted conjunctival grafts and underlying nasal sclera in association with conjunctival hyperemia [Figure 1a]. There was no intraocular inflammation, and the bed of harvested grafts showed no signs of inflammation in both eyes.

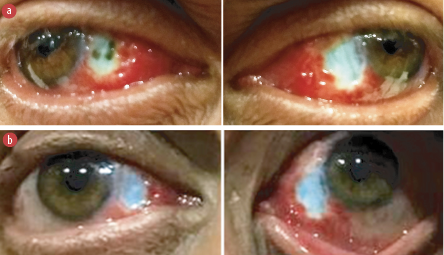 Figure 1: (a) Two weeks after the surgery. Shows bilateral melted conjunctival graft, melted nasal sclera with loss of vascularization (ischemia), and severe conjunctival hyperemia nasally. (b) Four days after the initiation of treatment.
Figure 1: (a) Two weeks after the surgery. Shows bilateral melted conjunctival graft, melted nasal sclera with loss of vascularization (ischemia), and severe conjunctival hyperemia nasally. (b) Four days after the initiation of treatment.
Infectious etiology was ruled out with negative gram stain and scleral scrapings, which showed no bacterial growth. Although the patient refused to perform rheumatological consultation at the time of presentation, the diagnosis of SINS was the provisional diagnosis according to the sequence of events and the examination. We stopped the previous treatment and commenced him on oral prednisolone (1 mg/kg) tapered over six weeks besides topical tobramycin ointment qid, topical Ketorolac tid, and lubricant eye drops (preservative-free and contains hyaluronic acid 0.18%) q.2h.
Three days later, he reported improvement of his symptoms and the examination revealed bilateral thickening of scleral bed with mild conjunctival hyperemia. We conducted close follow-ups and noticed a progressive improvement [Figure 1b and Figure 2]. At the end of the sixth week, his condition resolved entirely and remained stable over the last 18 months [Figure 3]. More than 18 months after the first presentation, the patient agreed to perform the investigations, which revealed negative results for serum rheumatoid factor, antinuclear antibody, perinuclear anti-neutrophil cytoplasmic antibodies, and cytoplasmic anti-neutrophil cytoplasmic antibodies.

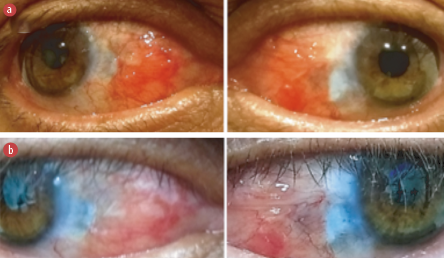 Figure 2: (a) Two weeks after the initiation of treatment shows healed and revascularized scleral bed in both eyes. (b) Four weeks after the initiation of treatment.
Figure 2: (a) Two weeks after the initiation of treatment shows healed and revascularized scleral bed in both eyes. (b) Four weeks after the initiation of treatment.

 Figure 3: Eighteen months from the onset of surgically induced necrotizing scleritis shows complete healing in both eyes.
Figure 3: Eighteen months from the onset of surgically induced necrotizing scleritis shows complete healing in both eyes.
Discussion
SINS may present for the first time after uneventful ocular surgery with a variable latent period that varies from one day to 40 years.1 The area of scleral melt develops adjacent to the surgical wound site with a possibility of the entire involvement of the anterior segment.1,2 Besides, it may be the first manifestation of systemic autoimmune disease.7 Autoimmunity or hypersensitivity is the etiological factor behind the development of SINS. This is attributed to the results of immunofluorescence techniques that show immune complexes in and around the walls of episcleral vessel and successful treatment with systemic immunosuppressive regimes.6 A review revealed that serological markers for connective tissue diseases are not present in about 38% of patients with SINS.1 Also, a clinicopathologic study reported that about 10% of patients who presented with SINS did not have any systemic autoimmune diseases.7
Scleral necrosis and melting are infrequent sequelae of ocular surgery with potentially devastating ocular consequences.1 This may appear after pterygium excision because of mitomycin C or adjunctive irradiation, leading to a delay in wound healing.2,4,5 Further, excessive cauterization is another cause of ischemic scleral necrosis.3 Since none of these etiologies were implicated in scleral melting and necrosis in our case, SINS was the most probable diagnosis.
Surgical trauma can trigger the immune complex-mediated vasculitis in a predisposed patient. At the site of trauma or injury, circulating immune complexes accumulate in the episcleral vessels and perforate scleral vessels leading to scleral destruction via inflammatory microangiopathy.7,8
Necrotizing scleritis with signs of adjacent inflammation carries a worse visual prognosis and a high risk of complications, particularly scleral thinning.9 It is characterized by a localized patch or area of scleritis with severe acute congestion. Inevitably, if left untreated it will progress to a patch of yellowish/grey sclera with a complete loss of scleral tissue. Thus, scleral edema with an overlying or nearby area of avascular episcleral tissue is strongly indicative and should be managed aggressively and promptly to prevent scleral necrosis and consequent perforation, especially in the early stages.9
Medical treatment of SINS includes immunosuppressive agents with oral steroids, methylprednisolone, and cyclophosphamide. Recently, tacrolimus has been used in patients not responding to cyclophosphamide or azathioprine.10–12 If the disease progress despite adequate medical treatment, surgical replacement of devitalized tissue such as corneal tissue grafts, tectonic scleral patch, and amniotic membrane grafts should be considered.11–13
In our case, the patient presented with SINS approximately two weeks after pterygium excision with ischemia and melting of both conjunctival graft and underlying sclera. Fortunately, he has responded well over six weeks of medical treatment. A few similar cases of SINS after pterygium excision with conjunctival autograft have been reported.11,14,15
Conclusion
SINS is a rare complication of ocular surgeries. It must be considered in the differential diagnosis of scleral inflammation and melting following such procedures only after excluding other causes. Prompt management is essential to prevent ocular and systemic devastating sequelae.
Disclosure
The authors declared no conflicts of interest. Written consent was obtained from the patient.
references
- 1. O’Donoghue E, Lightman S, Tuft S, Watson P. Surgically induced necrotising sclerokeratitis (SINS)–precipitating factors and response to treatment. Br J Ophthalmol 1992 Jan;76(1):17-21.
- 2. Galanopoulos A, Snibson G, O’Day J. Necrotising anterior scleritis after pterygium surgery. Aust N Z J Ophthalmol 1994 Aug;22(3):167-173.
- 3. Alsagoff Z, Tan DT, Chee SP. Necrotising scleritis after bare sclera excision of pterygium. Br J Ophthalmol 2000 Sep;84(9):1050-1052.
- 4. MacKenzie FD, Hirst LW, Kynaston B, Bain C. Recurrence rate and complications after beta irradiation for pterygia. Ophthalmology 1991 Dec;98(12):1776-1781.
- 5. Rubinfeld RS, Pfister RR, Stein RM, Foster CS, Martin NF, Stoleru S, et al. Serious complications of topical mitomycin-C after pterygium surgery. Ophthalmology 1992 Nov;99(11):1647-1654.
- 6. Fong LP, Sainz de la Maza M, Rice BA, Kupferman AE, Foster CS. Immunopathology of scleritis. Ophthalmology 1991 Apr;98(4):472-479.
- 7. Maza MS, Foster CS. Necrotizing scleritis after ocular surgery. A clinicopathologic study. Ophthalmology 1991 Nov;98(11):1720-1726.
- 8. Maza MS, Tauber J, Foster CS. The Sclera. 2nd ed. New York, Springer; 2012. p. 225.
- 9. Pavesio C, ed. Scleritis. In: Series Ed.: Singh, Arun D. Essentials in ophthalmology. 1st ed. New York, Springer; 2017. p. 22.
- 10. Vagefi MR, Hollander DA, Seitzman GD, Margolis TP. Bilateral surgically induced necrotising scleritis with secondary superinfection. Br J Ophthalmol 2005 Jan;89(1):124-125.
- 11. Sridhar MS, Bansal AK, Rao GN. Surgically induced necrotizing scleritis after pterygium excision and conjunctival autograft. Cornea 2002 Apr;21(3):305-307.
- 12. Young AL, Wong SM, Leung AT, Leung GY, Cheng LL, Lam DS. Successful treatment of surgically induced necrotizing scleritis with tacrolimus. Clin Exp Ophthalmol 2005 Feb;33(1):98-99.
- 13. Ti SE, Tan DT. Tectonic corneal lamellar grafting for severe scleral melting after pterygium surgery. Ophthalmology 2003 Jun;110(6):1126-1136.
- 14. Jain V, Shome D, Natarajan S, Narverkar R. Surgically induced necrotizing scleritis after pterygium surgery with conjunctival autograft. Cornea 2008 Jul;27(6):720-721.
- 15. Yamazoe K, Shimazaki-Den S, Otaka I, Hotta K, Shimazaki J. Surgically induced necrotizing scleritis after primary pterygium surgery with conjunctival autograft. Clin Ophthalmol 2011;5:1609-1611.