Hyperthyroidism is a rare but potentially serious condition in childhood. Its reported incidence in postpubertal children is 0.9 per 100 000.1 Graves’ disease is the most common cause of hyperthyroidism in children, accounting for more than 95% of the cases. Clinical manifestations of hyperthyroidism are highly variable. Thyroid storm is an extreme manifestation of hyperthyroidism and a medical emergency.2 Thyroid storm as an initial manifestation is rare, especially in children, among whom its diagnosis is usually very challenging.3 Thyroid storm can manifest anytime in underlying hyperthyroidism. Though manifestations of thyrotoxicosis are typical, a high index of suspicion of possible thyroid storm should be kept regarding any patient who presents with systemic decompensation.
We report here a case of an adolescent girl who presented with left-sided pneumonia with empyema and had tachyarrhythmia, which on further evaluation turned out to be thyroid storm.
Case Report
A 16-year-old female, presented in the emergency department with complaints of fever, cough, and chest pain for 15 days and progressive breathing difficulty for 12 days. On examination, she was conscious, had fever, tachypnea (respiratory rate = 38/minute) with chest retraction, tachycardia (heart rate (HR) = 128/minute), and raised BP = 147/87 mmHg). On the respiratory system examination, chest movement was found decreased, accompanied by dull percussion notes. There was reduced air entry on left interscapular, infrascapular, and infra-axillary areas. A chest x-ray showed massive left-sided pleural effusion with mediastinal shift to the right [Figure 1a]. Ultrasound chest revealed moderate to severe effusion with loculation and thick septation on the left side. A diagnosis of left-sided pneumonia with empyema was made. She was started on intravenous antibiotics (amoxycillin and clavulanic acid) and an intercostal drainage (ICD) tube was inserted. Intrapleural urokinase 40 000 IU in 40 mL of normal saline was delivered as per the British Thoracic Society guideline.4
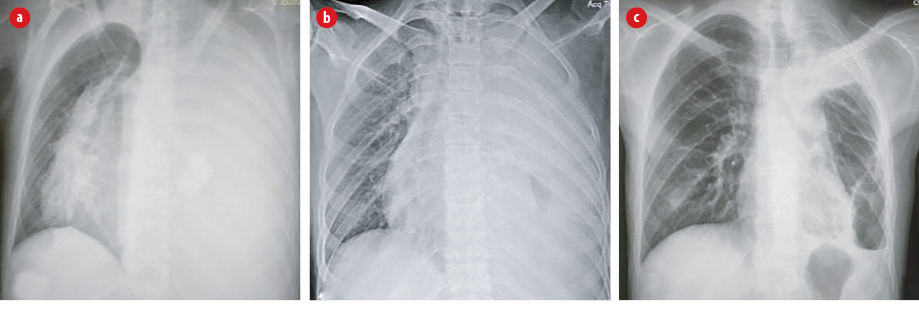
Figure 1: Chest x-ray posteroanterior view. (a) Complete white-out of left hemithorax with mediastinal shift to the right; (b) dense opacity in left hemithorax with some aeration; and (c) six weeks post-surgery, showing marked improvement with an air pocket in the left lower lobe.
During the emergency stay, the patient had persistent tachycardia, which was out of proportion to fever (HR 148/min, temperature 37.80C) with irregular rhythm and wide pulse pressure. An electrocardiogram showed atrial fibrillation. She was also found to have exophthalmos, tremors of outstretched hand and a thyroid swelling in the neck. She was evaluated for other causes of tachyarrhythmia as per Pediatric Advanced Life Support guidelines which included 6H (hypovolemia, hypoxia, acidosis, hypoglycemia, hypo/hyperkalemia, and hypothermia) and 5T (pneumothorax, tamponade, trauma, thromboembolism, and exposure to toxins),5 but there was no evidence of any of these. A possibility of hyperthyroidism was considered and investigated. The thyroid profile revealed very high levels of free T3 (FT3) and FT4 with very low thyroid-stimulating hormone (TSH) (FT3: 27.8 pg/mL, FT4: 7.16 ng/dL, and TSH < 0.004 mIU/L). The Burch-Wartofsky score was 65, scores ≥ 45 being ‘highly suggestive’ of thyroid storm.6 A working diagnosis of hyperthyroidism with thyroid storm was made and the patient was started on propranolol (20 mg every six hours) and methimazole (0.5 mg/kg/day in two divided doses). She showed significant clinical improvement in tachyarrhythmia in the next 48 hours.
Meanwhile, she continued to have fever and breathing difficulty; therefore, the antibiotic was upgraded (piperacillin + vancomycin). On repeat chest imaging dense opacity was seen in the left hemithorax with some aeration [Figure 1b]. Chest ultrasound revealed plenty of pus with thick septa despite the six doses of intrapleural urokinase. After pediatric surgery consultation she underwent video-assisted thoracoscopic surgery. Following the procedure there was a significant clinical and radiological improvement [Figure 1c]. A repeat thyroid profile at two weeks also showed improvement in thyroid function (FT3: 8.46 pg/mL, FT4: 4.17 ng/dL, and TSH < 0.004 mIU/L). In due course, the ICD tube was removed and the patient was discharged on anti-thyroid medications and oral antibiotics with a plan to complete a total six weeks course of antibiotics. On follow-up at six weeks, she had gained adequate weight, and there was no recurrence of the symptoms. In addition, the patient did not show any adverse effects attributable to propranolol and methimazole.
Discussion
Graves’ disease is the most common cause (> 95%) of hyperthyroidism in children.2 Thyroid storm is considered as an extreme manifestation of hyperthyroidism. It is a life-threatening condition, with a mortality rate of 8%–25%.3 There is evidence that any acute illness, such as stroke, surgery, infection, or trauma, can precipitate a thyroid storm.7 In a case reported by Yuan et al, 8 a thyroid storm was precipitated by organophosphorus poisoning. Aslan et al,9 reveals how a respiratory syncytial virus infection triggered a thyroid storm in a patient with an underlying undiagnosed Grave’s disease. Underland et al,10 reported a case of a 5-year-old child with streptococcal pharyngitis who subsequently developed cardiomyopathy and post-streptococcal glomerulonephritis with thyroid storm. In the same case, Burch-Wartofsky score was 70, which led them to also use β2 blocker and methimazole for acute management.10 Recently, Ladd et al,3 reported a case of thyroid storm in a two years and nine months old child who presented with febrile seizure, persistent tachycardia, and wide pulse pressure.
Pneumonia with empyema thoracis seemed to be a precipitating factor in the present case. The role of infections in triggering thyroid storm is not well elucidated; however, the postulated mechanism is as follows: infection decreases the serum binding of T3 and T4 which leads to increase FT3 and FT4 levels, ultimately resulting in thyroid storm.7 Thyroid storm could be an initial presentation of underlying hyperthyroidism.2,7
There are many clinical scoring tools in practice that help predict an underlying thyroid storm. The most used one is Burch-Wartofsky criteria, where a score ≥ 45 is ‘highly suggestive’ of thyroid storm; 25–44 is ‘suggestive;’ score < 25 means a thyroid storm is ‘unlikely.6 Guidelines from the American Thyroid Association and the American Association of Clinical Endocrinologists suggest a multimodality treatment approach with close monitoring in an intensive care unit.11
The treatment options include antithyroid medications (methimazole and propylthiouracil), β-adrenergic blocker (propranolol, atenolol, metoprolol, nadolol, or esmolol), inorganic iodine solutions, radioiodine (I-131) therapy, other drugs (corticosteroid, lithium carbonate, cholestyramine, rituximab), and surgical treatment.12 In the present case, methimazole was started as it is considered as the first line of therapy in children along with propranolol, which shows significant clinical and biochemical improvement in the course of two weeks.
Conclusion
Thyroid storm can be an initial presentation of underlying hyperthyroidism in children, and it could be precipitated by infection as pneumonia with empyema as in the present case. Since it is a life-threatening condition, a high degree of suspicion and early institution of therapy is vital.
Disclosure
The authors declare no conflicts of interest. Parents' consent was taken.
references
- 1. Williamson S, Greene SA. Incidence of thyrotoxicosis in childhood: a national population based study in the UK and Ireland. Clin Endocrinol (Oxf) 2010 Mar;72(3):358-363.
- 2. Srinivasan S, Misra M. Hyperthyroidism in children. Pediatr Rev 2015 Jun;36(6):239-248.
- 3. Ladd JM, Sabsabi B, von Oettingen JE. Thyroid Storm in a Toddler Presenting as a Febrile Seizure. Pediatrics 2020 Feb;145(2):e20191920.
- 4. Balfour-Lynn IM, Abrahamson E, Cohen G, Hartley J, King S, Parikh D, et al; Paediatric Pleural Diseases Subcommittee of the BTS Standards of Care Committee. BTS guidelines for the management of pleural infection in children. Thorax 2005 Feb;60(Suppl 1):i1-i21.
- 5. de Caen AR, Berg MD, Chameides L, Gooden CK, Hickey RW, Scott HF, et al. Part 12: Pediatric Advanced Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015 Nov;132(18)(Suppl 2):S526-S542.
- 6. Burch HB, Wartofsky L. Life-threatening thyrotoxicosis. Thyroid storm. Endocrinol Metab Clin North Am 1993 Jun;22(2):263-277.
- 7. Akamizu T, Satoh T, Isozaki O, Suzuki A, Wakino S, Iburi T, et al; Japan Thyroid Association. Diagnostic criteria, clinical features, and incidence of thyroid storm based on nationwide surveys. Thyroid 2012 Jul;22(7):661-679.
- 8. Yuan YD, Seak CJ, Lin CC, Lin LJ. Thyroid storm precipitated by organophosphate intoxication. Am J Emerg Med 2007 Sep;25(7):861.e1-861.e3.
- 9. Aslan IR, Baca EA, Charlton RW, Rosenthal SM. Respiratory syncytial virus infection as a precipitant of thyroid storm in a previously undiagnosed case of graves’ disease in a prepubertal girl. Int J Pediatr Endocrinol 2011;2011:138903.
- 10. Underland LJ, Villeda GA, Pal A, Lam L. A Case of Thyroid Storm Associated with Cardiomyopathy and Poststreptococcal Glomerulonephritis. Case Rep Pediatr 2016;2016:7192359.
- 11. Ross DS, Burch HB, Cooper DS, Greenlee MC, Laurberg P, Maia AL, et al. 2016 American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis. Thyroid 2016 Oct;26(10):1343-1421.
- 12. Minamitani K, Sato H, Ohye H, Harada S, Arisaka O; Committee on Pharmaceutical Affairs, Japanese Society for Pediatric Endocrinology, and the Pediatric Thyroid Disease Committee, Japan Thyroid Association (Taskforce for the Revision of the Guidelines for the Treatment of Childhood-Onset Graves’ Disease). Guidelines for the treatment of childhood-onset Graves’ disease in Japan, 2016. Clin Pediatr Endocrinol 2017;26(2):29-62.