Repetitive masticatory muscle activity characterized by clenching or grinding of teeth or bracing or thrusting of the mandible, while awake or asleep, either voluntarily or involuntarily, may be defined as bruxism.1 There are several consequences of bruxism such as temporomandibular joint (TMJ) disorders and periodontal deterioration due to occlusal trauma.2 Also reported are tooth wear, chipping of teeth and prostheses, masticatory muscle pain, and sensitive teeth.3 The etiology is multifactorial and still an unsolved question.4 The most dominant sign related to bruxism is tooth wear.5 A number of studies have reported positive association between tooth wear and bruxism.6–8
Bruxism is of particular concern to dental profession due to its side effects on the oral and maxillofacial area. Studies have differed in their estimation of the prevalence of bruxism.9–12 Bruxism is attributed to multiple factors among which stress could be on the top, even though an explicit causal relationship has not been established. Several studies have reported an association between anxiety and depression with bruxism.7–10 The stress experienced in the work environment has been shown to be related to bruxism.11
Military fighter pilots’ unique working environment exposes them to high occupational stress that might give rise to a variety of health problems.12,13 Current knowledge of the relationship between bruxism and occupational stress is based on inadequate data. A few investigations elsewhere among pilots have found moderate to high prevalence (30%–70%) of parafunctional muscle activity, represented as bruxism.12,13 It is also important to investigate whether military pilots have health consequences associated with occupational stress. Thus, the aim of the research was to assess the prevalence of bruxism and occupational stress among the Saudi Arabian fighter pilots.
Methods
The subjects of this cross-sectional study in Saudi Arabia were a group of fighter pilots who were compared to a control group of non-pilot officers. For convenience, the participants were recruited among the Saudi Arabian Air Force officers who were visiting the Aviation Medical Clinic in Dhahran, Saudi Arabia for routine medical and dental examination. The sample size was calculated using the following assumptions: alpha error = 5%, study power = 90%, estimated bruxism prevalence in fighter pilots = 65%,12,13 and null percent = 50%. The minimum required sample size to assess bruxism prevalence was calculated to be 110 (http://www.stat.ubc.ca/~rollin/tats/ssize/b1. html). The fighter pilot officers and non-pilot (airfield operations, ground control, logistic, and law enforcement) officers who met the following inclusion criteria were enrolled in the study: (a) have at least 21 teeth, (b) no psychological or psychiatric issues, and (c) be in a good general health as confirmed by the attending physician at the aeromedical center. Those with history of chronic systemic diseases or did not sign the informed consent were excluded. The study was approved by the Ethics and Research Committee at the College of Dentistry, Imam Abdulrahman Bin Faisal University, and permitted by the Aero Medical Center in King Abdul Aziz Air Base in Dhahran, Ministry of Defense, Saudi Arabia.
Two dentists were trained on clinical assessment of tooth wear using the tooth wear severity index. Calibrating the dentists as per the tooth wear severity index was essential for reliability of the study results. The calibration session was conducted by the bench-maker examiner, an experienced dentist considered the ‘gold standard.’ For training purposes, both dentists examined a group of 10 regular dental patients for tooth wear. A Kappa > 0.75 of inter-examiner reliability was achieved before the launch of the main study, with the two dentists achieving intra-examiner reliabilities of 77% and 82%, respectively.
The data collection was carried out between February 2018 and May 2019 as follows: both dentists invited prospective subjects who satisfied the inclusion criteria to participate in the study; those who consented were requested to complete self-administered questionnaires; each subject’s clinical data was also collected. Since the study included both pilots and non-pilots, the subject recruitment was conducted in two phases: first inducting pilots till the required sample size was reached (N = 110), followed by the same number of non-pilots (the control group).
While waiting for their dental examinations, the subjects completed a short version of Karasek’s questionnaire comprising 11 questions.14 It is a well-known validated tool to assess occupational stress and has been used in numerous studies.6,10,15 In the current study, two scales were used, namely: demand scale with 5 items and control scale with 6 items. The responses were scored in Likert scale format using numerical values: ‘often/very high’ = 4; ‘sometimes/high’= 3; ‘seldom/low’ = 2; ‘never/almost never/very low’ = 1. The score range for demand was 5–20 and 6–24 for control. Higher scores in each category indicated higher demand/higher control. Following the theory of the Job Demand-Control model,16 a median split of total sample or subsample job-specific scale values was used to construct four combinations of demand and control, where each participant is placed in one of the following quadrants: low strain (low demand + high control), active (high demand + high control), passive (low demand + low control), and high strain (high demand + low control), as illustrated in Figure 1.15 Those subjects falling in the high strain quadrant were considered under stress in this study. The questionnaire also included demographic information and basic health-related questions including queries on smoking and bruxism. Regarding bruxism, the participants were asked to monitor and record in a two-week diary, whether they ground their teeth, clenched teeth together or braced their jaw during daytime and while sleeping at night.
The tooth wear severity index as described by Pullinger and Seligman was used in this study where the condition of each tooth was scored as follows: 0 = no facet; 1 = slight facet; 2 = noticeable flattening with the normal planes of contour; 3 = flattening of cusps or grooves; and 4 = total loss of contour and dentinal exposure when identifiable. Subjects whose overall tooth wear severity scores of 0–2 were considered having ‘low tooth wear’ and those with severity scores of 3 or 4 as having
‘severe tooth wear’.16
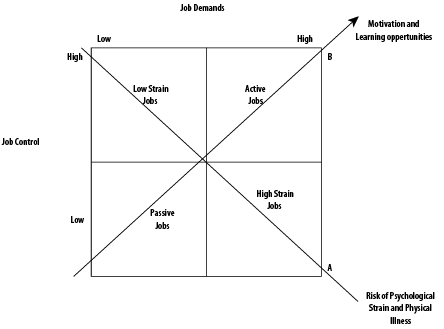
Figure 1: Job Demand-Control Model (based on: Karasek et al., 1998).15
The clinical features of both awake and asleep bruxism included the presence of masticatory muscle hypertrophy as well as indentations on the tongue or lip and/or a linea alba on the inner cheek. Others included damage to the dental hard tissues (cracked teeth), repetitive failures of restorative work or prosthodontic constructions, or mechanical wear of the teeth (attrition).
The assessment of bruxism was confirmed using the non-instrumental approach of the International Consensus on the Assessment of Bruxism that included both clinical examination and self-report of diurnal or nocturnal bruxism.1,4
The data was entered in Microsoft Excel 2010 and transferred to IBM SPSS version 22 for statistical analysis. The descriptive statistics included frequency distributions with percentages for categorical variables, as well as means and standard deviations (SD) for continuous variables. For the bivariate analysis, variables with more than two levels, such as control and demand, were dichotomized into two groups to develop the Job Demand-Control model. The differences between pilots and non-pilots for bruxism, occupational stress, and combined bruxism and high stress were compared using chi square test. This was followed by a univariate and multivariate logistic regression test with bruxism as the dependent variable controlling for confounding factors such as occupational stress (low vs. high), type of occupation (pilot vs. non-pilot), and smoking status. Demographic variables such as age and work experience were not included in the logistic regression test to avoid collinearity in the results. p < 0.050 was considered statistically significant.
Table 1: Sociodemographic and health characteristics of the study subjects.
|
Continuous, M (SD) |
|
|
|
|
Age, years |
28.0 (5.0) |
31.6 (7.0) |
29.8 (6.3) |
|
Tooth wear |
2.3 (1.1) |
2.1 (0.8) |
2.2 (0.9) |
|
Categorical |
|
|
|
|
Work experience, years |
|
|
|
|
≤ 5 |
54 (49.1) |
58 (52.7) |
112 (50.9) |
|
> 5 |
56 (50.9) |
52 (47.3) |
108 (49.1) |
|
Smoking |
|
|
|
|
Yes |
44 (40.0) |
46 (41.8) |
90 (40.9) |
|
No |
66 (60.0) |
64 (58.2) |
130 (59.1) |
|
Degree of tooth wear |
|
|
|
|
Grade 1 |
36 (32.7) |
28 (25.5) |
64 (29.1) |
|
Grade 2 |
16 (14.5) |
48 (43.6) |
64 (29.1) |
|
Grade 3 |
44 (40.0) |
32 (29.1) |
76 (34.5) |
|
Grade 4 |
14 (12.7) |
2 (1.8) |
16 (7.3) |
|
History of Bruxism |
|
|
|
|
Bruxer |
62 (56.4) |
40 (36.4) |
102 (46.4) |
M: mean; SD: standard deviation.
Table 2: Job Demand-Control Model for the study subjects.
|
Pilot |
|
|
|
|
High |
14 (12.7) |
26 (23.6) |
40 (36.4) |
|
Low |
20 (18.2) |
50 (45.5) |
70 (63.6) |
|
Total |
34 (30.9) |
76 (69.1) |
110 (100) |
|
Non-Pilot |
|
|
|
|
High |
34 (30.9) |
18 (16.4) |
52 (47.3) |
|
Low |
28 (25.5) |
30 (27.3) |
58 (52.7) |
|
Total |
62 (56.4) |
48 (43.6) |
110 (100) |
|
All |
|
|
|
|
High |
48 (21.8) |
44 (20.0) |
92 (41.8) |
|
Low |
48 (21.8) |
80 (36.4) |
128 (58.2) |
Results
The final sample (N = 220) consisted of 110 pilots and 110 nonpilots. The participation rate was 33.0% for pilots and 58.0% for non-pilots, with a combined participation rate of 45.5%. The participants’ average age was 29.8±6.3 years, pilots being slightly younger than non-pilots (28.0±5.0 years versus 31.6±7.0 years). Nearly half of the pilots (49.1%) and 52.7% non-pilots had ≤ 5 years working experience, while the remainder (50.9% pilots and 47.3% of non-pilots) had > 5 years experienced. Smokers comprised 40.0% of the pilots and 41.8% of the non-pilots. The overall mean (SD) tooth wear (according to the index used) was 2.2±0.9 (2.3±1.1 for pilots and 2.1±0.8 for non-pilots). As for the degree of tooth wear, 40.0% pilots were recorded as grade 3, while 43.6% non-pilots were recorded as grade 2. History of bruxism was present in 46.4% of the total sample, with higher prevalence among pilots than non-pilots (56.4% and 36.4%, respectively) [Table 1].
The participants’ occupational stress was assessed using their responses to the questionnaire. The stress experienced was classified as per the Job Demand-Control Model [Table 2]. Participants who experienced high demand but had low control were considered to be under stress. According to the model, 45.5% pilots were identified as having occupational stress compared to only 27.3% non-pilots.
Pilots also exhibited more bruxism than non-pilots (52.7% vs. 30.9%). Pilots who experienced both the conditions (high occupational stress and bruxism) were more than thrice the number of non-pilots (23.6% vs. 7.3%) [Table 3].
Logistic regression analysis with the status of bruxism as the dependent variable is presented in Table 4. There was a significant association between bruxism and type of occupation (pilot vs. non-pilot) controlling for occupational stress and smoking in both the univariate and multivariate logistic regression tests: (OR) = 2.5, 95% confidence interval (CI): 1.1–5.4; p = 0.016 and OR = 2.6, 95% CI: 1.2.–5.8; p = 0.020), respectively.
Table 3: The relationship between occupational stress, bruxism, and combined bruxism and high stress with occupation (pilot vs. non-pilot).
|
Stress |
|
|
|
|
|
Low stress |
60 (54.5) |
80 (72.7) |
2.2 (1.0–4.9) |
0.037* |
|
High stress |
50 (45.5) |
30 (27.3) |
|
|
|
Bruxism |
|
|
|
|
|
Non-bruxer |
52 (47.3) |
76 (69.1) |
2.5 (1.1–5.4) |
0.016* |
|
Bruxer |
58 (52.7) |
34 (30.9) |
|
|
|
Bruxism and high stress |
|
|
|
|
|
Absent |
84 (76.4) |
102 (92.7) |
3.9 (1.7–9.2) |
0.001* |
OR: odds ratio; CI: confidence intervals.
aReference group; *Significant at p < 0.050.
Table 4: Univariate and multivariate logistic regression analysis with the status of bruxism as the
dependent variable.
|
Occupational Stress |
|
|
|
|
|
High stress |
1.0 (0.5–2.3) |
0.535 |
1.1 (0.5–2.6) |
0.763 |
|
Low stressa |
|
|
|
|
|
Occupation |
|
|
|
|
|
Pilot |
2.5 (1.1–5.4) |
0.016* |
2.6 (1.2–5.8) |
0.020* |
|
Non-pilota |
|
|
|
|
|
Smoking |
|
|
|
|
|
Yes |
1.4 (0.7–3.0) |
0.254 |
1.4 (0.7–3.2) |
0.364 |
OR: odds ratio; CI: confidence intervals; aReference group; *Significant at p < 0.050.
Discussion
This is the first study that explores the prevalence of bruxism and occupational stress in Saudi Arabian military pilots. Bruxism was found in 52.7% pilots, which is within the range of 30.4%–69% prevalence reported among military pilots in other international studies.12,13,17,18 When compared with other populations with different occupations associated with stress, the prevalence of bruxism ranged from 50% to 60%.10,11,19,20 In the current study, the prevalence of bruxism was 36.4% among non-pilot officers. Some global studies found 20%–30% prevalence in the general population irrespective of occupation.21,22 The wide variations in the prevalence of bruxism between studies might be explained by differences in study design such as the choice of bruxism index, method of calibration of examiners, participant demography and other variables. It is also relevant to mention here that several of these international epidemiological studies assessed bruxism as a deteriorating oral condition without taking into account the confounding effect of occupational stress.
The use of the Job Content Questionnaire in this study helped assess the occupational stress levels in the study subjects. High job demand and low job control jointly will lead to job strain as shown by the Job Demand-Control model,15 which is widely used in epidemiological research on occupational stress.23,24 In this study, pilots experienced more stress than non-pilots (45.5% vs. 27.3%). Several cardiovascular risk factors such as blood pressure, heart rate, body mass index, serum total cholesterol levels, and cigarette smoking are also associated with job strain in workers.25,26 The Job Demand–Control model also helped identify the primary causes of job strain to be administrative factors and the work atmosphere.27
The Job Demand–Control model is also used to assess the relationship between psychological job demand and general fatigue, as well as reduced activity.28 Therefore, occupational stress should not be ignored, due to its association with poor health and fatigue.
The present study also shed light on the combined effect of occupational stress and bruxism in the same individual. High occupational stress with bruxism was present in 23.6% pilots and 7.3% non-pilots. Pilots also were more than thrice as likely to have high occupational stress with bruxism than non-pilots. The results of this study are consistent with those from other studies that addressed the association between occupational stress and bruxism in pilots.12,13,17,18 Negative consequences of stress have been observed also among certain other categories of pilots. Bauer et al,27 studied the effect of occupational stress on helicopter emergency service pilots from four European countries while Barbarewicz et al,28 investigated psychophysical stress among maritime pilots in Germany. In both studies, the side effects of occupational stress included general health and psychological problems including clenching of teeth and possible bruxism. The association between occupational stress and bruxism has also been observed in different professions and nationalities using different occupational stress instruments.11,20
Given the clear evidence from this study and from other studies elsewhere on the relationship between occupational stress and bruxism, there is urgent need to prevent or reduce occupational stress. There are several initiatives the pilots themselves can take. As studies show, muscular activity associated with bruxism is largely involuntary whether one is awake or asleep. One way of mitigating the habit is to train fighter pilots to have conscious awareness of their body’s responses to stress including the tendency for vigorous clenching. Mindfulness meditation and relaxation exercises may help improve body awareness, reduce overall stress with consequent reduction in the involuntary muscular activity characteristic of bruxism. In some cases, occlusal splints or mouth guards can be custom-manufactured and placed to prevent physical contact between the occlusal surfaces; thus, minimizing tooth wear.5,13,17
This study faced a major obstacle during the data collection phase due to low participation rate, (33.0%) of military pilots, who had little time away from their military duties to spare the considerable time required to participate in the study. Thus, it became necessary to extend the data collection period across several months. These recruitment difficulties might have introduced a selection bias. It is also important to mention that there were no previous dental records for comparison purposes to assess the chronological progress of bruxism in the subjects. Another limitation was the cross-sectional nature of the study, which made it difficult to establish causal relationship between occupational stress and bruxism. A drawback of using questionnaires for data collection is that respondents might underreport or overreport occupational stress due to recall bias. Therefore, the findings of this study should be interpreted carefully before generalizing them to pilot population in non-military organizations. Further studies that address the above limitations are warranted.
Conclusion
Within the limitations of this study, the pilots in this study demonstrated significantly higher occupational stress and bruxism than the non-pilots. The pilots were more than three times as likely to have both stress and bruxism compared to non-pilots. Further investigations are necessary to examine a possible causal relationship between occupational stress and bruxism. It is necessary to establish basic programs for the treatment and control of occupational stress and treat pathologies that may compromise the military performance of pilots of the Saudi Arabian Air Force.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
references
- 1. Lobbezoo F, Ahlberg J, Glaros AG, Kato T, Koyano K, Lavigne GJ, et al. Bruxism defined and graded: an international consensus. J Oral Rehabil 2013 Jan;40(1):2-4.
- 2. Manfredini D, Lobbezoo F. Relationship between bruxism and temporomandibular disorders: a systematic review of literature from 1998 to 2008. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010 Jun;109(6):e26-e50.
- 3. Alves AC, Alchieri JC, Barbosa GA. Bruxism. Masticatory implications and anxiety. Acta Odontol Latinoam 2013;26(1):15-22.
- 4. Lobbezoo F, Ahlberg J, Raphael KG, Wetselaar P, Glaros AG, Kato T, et al. International consensus on the assessment of bruxism: Report of a work in progress. J Oral Rehabil 2018 Nov;45(11):837-844.
- 5. Goldstein G, DeSantis L, Goodacre C. Bruxism: best evidence consensus statement. J Prosthodont 2021 Apr;30(S1):91-101.
- 6. Ahlberg J, Lobbezoo F, Ahlberg K, Manfredini D, Hublin C, Sinisalo J, et al. Self-reported bruxism mirrors anxiety and stress in adults. Med Oral Patol Oral Cir Bucal 2013 Jan;18(1):e7-e11.
- 7. van Selms M, Kroon J, Tuomilehto H, Peltomaa M, Savolainen A, Manfredini D, et al. Self-reported sleep bruxism among Finnish symphony orchestra musicians: Associations with perceived sleep-related problems and psychological stress. Cranio 2020 Nov;(Nov):1-8.
- 8. Kuhn M, Türp JC. Risk factors for bruxism. Swiss Dent J 2018 Feb;128(2):118-124.
- 9. Polmann H, Réus JC, Massignan C, Serra-Negra JM, Dick BD, Flores-Mir C, et al. Association between sleep bruxism and stress symptoms in adults: A systematic review and meta-analysis. J Oral Rehabil 2021 May;48(5):621-631.
- 10. Carvalho AL, Cury AA, Garcia RC. Prevalence of bruxism and emotional stress and the association between them in Brazilian police officers. Braz Oral Res 2008 Jan-Mar;22(1):31-35.
- 11. Nakata A, Takahashi M, Ikeda T, Hojou M, Araki S. Perceived psychosocial job stress and sleep bruxism among male and female workers. Community Dent Oral Epidemiol 2008 Jun;36(3):201-209.
- 12. Lurie O, Zadik Y, Einy S, Tarrasch R, Raviv G, Goldstein L. Bruxism in military pilots and non-pilots: tooth wear and psychological stress. Aviat Space Environ Med 2007 Feb;78(2):137-139.
- 13. Yu Q, Liu Y, Chen X, Chen D, Xie L, Hong X, et al. Prevalence and associated factors for temporomandibular disorders in Chinese civilian pilots. Int Arch Occup Environ Health 2015 Oct;88(7):905-911.
- 14. Karasek R, Theorell T. Healthy work: stress, productivity, and the reconstruction of working life. Basic Book, New York; 1990.
- 15. Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol 1998 Oct;3(4):322-355.
- 16. Pullinger AG, Seligman DA. The degree to which attrition characterizes differentiated patient groups of temporomandibular disorders. J Orofac Pain 1993;7(2):196-208.
- 17. Marín M, Rodríguez Y, Gamboa E, Ríos J, Rosas J, Mayta-Tovalino F. Level of work stress and factors associated with bruxism in the military crew of the Peruvian Air Force. Med J Armed Forces India 2019 Jul;75(3):297-302.
- 18. Kaushik SK, Madan R, Gambhir A, Prasanth T. Aviation stress and dental attrition. Int J Aerosp Med 2009;53(1):6-10.
- 19. Alajbeg IZ, Zuvela A, Tarle Z. Risk factors for bruxism among Croatian navy employees. J Oral Rehabil 2012 Sep;39(9):668-676.
- 20. Rao SK, Bhat M, David J. Work, stress, and diurnal bruxism: a pilot study among information technology professionals in Bangalore City, India. Int J Dent 2011;2011:650489.
- 21. Winocur E, Uziel N, Lisha T, Goldsmith C, Eli I. Self-reported bruxism - associations with perceived stress, motivation for control, dental anxiety and gagging. J Oral Rehabil 2011 Jan;38(1):3-11.
- 22. Sutin AR, Terracciano A, Ferrucci L, Costa PT Jr. Teeth grinding: is emotional stability related to bruxism? J Res Pers 2010 Jun;44(3):402-405.
- 23. Poorabdian S, Mirlohi AH, Habibi E, Shakerian M. Association between job strain (high demand-low control) and cardiovascular disease risk factors among petrochemical industry workers. Int J Occup Med Environ Health 2013 Aug;26(4):555-562.
- 24. Durand AC, Bompard C, Sportiello J, Michelet P, Gentile S. Stress and burnout among professionals working in the emergency department in a French university hospital: Prevalence and associated factors. Work 2019;63(1):57-67.
- 25. Jalilian H, Shouroki FK, Azmoon H, Rostamabadi A, Choobineh A. Relationship between job stress and fatigue based on job demand-control-support model in hospital nurses. Int J Prev Med 2019 May;10:56.
- 26. Abu Farha R, Alefishat E. Shift work and the risk of cardiovascular diseases and metabolic syndrome among Jordanian employees. Oman Med J 2018 May;33(3):235-242.
- 27. Bauer H, Herbig B. Occupational stress in helicopter emergency service pilots from 4 European countries. Air Med J 2019 Mar - Apr;38(2):82-94.
- 28. Barbarewicz F, Jensen HJ, Harth V, Oldenburg M. Psychophysical stress and strain of maritime pilots in Germany. A cross-sectional study. PLoS One 2019 Aug;14(8):e0221269.