The COVID-19 pandemic placed complex and heavy demands on healthcare systems worldwide. In Oman, the first two cases of COVID-19 infection were detected on February 24, 2020. Within 10 weeks, there were almost 3000 laboratory confirmed cases.1 As the human and material resources stretched thin, hospitals were driven to innovate. Coordinated communication and sustained collaboration are known to preserve healthcare capacity to meet community needs during pandemics, where there is pressure for organizations to react faster than normal.2 Accordingly, teams encompassing both interprofessional and interdisciplinary members became the principal tool for effective planning and execution at hospitals.
There is evidence that using lean systematic methods in health care organizations—where problems are defined, processes understood, and value streams mapped, and thereby an optimal patient pathway is adopted—can boost performance, enhance patient experience, increase employee engagement, and reduce waste and costs.3,4 Agile approach based on teamwork also improves the efficiency of healthcare organizations.5 Such an approach need not follow prescriptive practices or set tools, although they do employ some organizational frameworks such as strategic directives to plan work.6 Documentation in the forms of workflow algorithms or standard operating procedures are created as part of the innate process of collaborating, promoting sustainability but with the initial intent on facilitating communication.4,6 This allows the internal work processes to speed up to deliver more value, allows care to be more adaptive and responsive to new knowledge and more effective in adopting new technologies.6 The agile approach values human communication and feedback, producing results in small units with flexibility. Agile strategy as described by Kotter7 is designed to function within a traditional organizational hierarchy, where accelerator teams require the flexibility and agility of a network [Figure 1].
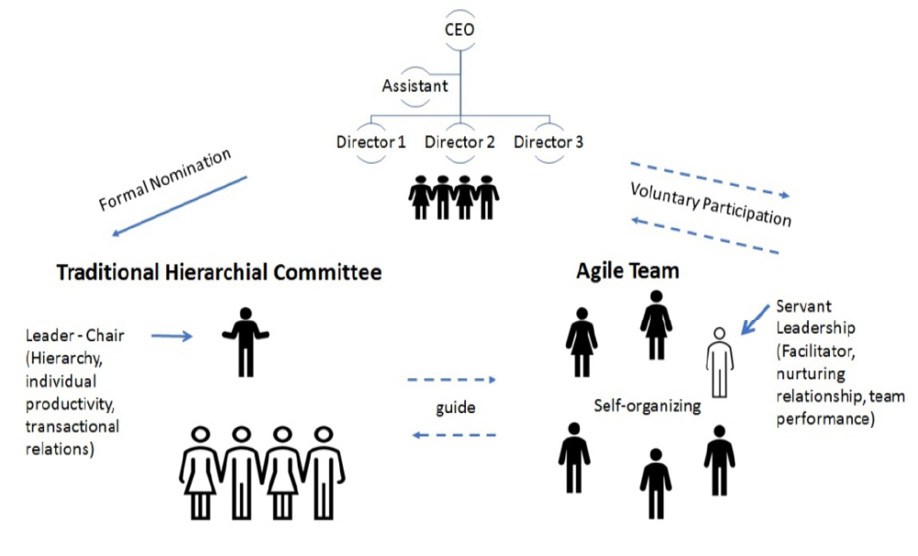
Figure 1: Traditional hierarchical committee versus agile team and their relationship.
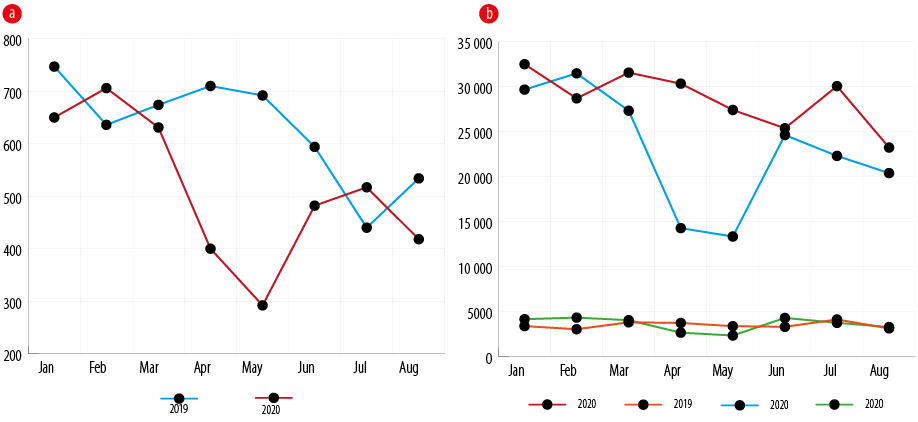
Figure 2: Impact of COVID-19 pandemic on hospital elective services in 2020 compared with 2019. (a) Day care and (b) outpatient.
Methods
With 1,056 beds, the Royal Hospital is the largest tertiary care hospital under Oman’s Ministry of Health. It is a referral center offering specialized healthcare (free of cost for Omani nationals). During the COVID-19 pandemic, the hospital faced extraordinary challenges being assigned to care for an unprecedented inflow of patients including those who required critical care.
To manage the pressure, the hospital administration formally established an initial five-member project management team (PMT) to facilitate the improvement projects within the hospital. The PMT reported biweekly to the hospital’s director general. Under the PMT, multiple agile teams were formed with 6–12 members each. Each agile team contributed within the context of its core specialty. The PMT maintained weekly track of progress and facilitated meetings with the agile team leaders. The members each agile team was recruited by the agile team leader from among the personnel who had the heart and mind to be voluntarily involved in the initiative. At least one member was required to be experienced in leading projects or trained in process improvement (e.g., lean methods). All agile teams formed internal WhatsApp® groups for virtual communication. The team leaders established their own WhatsApp groups to facilitate inter-departmental communication.
The first project dealt with the resumption of elective services. The PMT acted as the core project team to direct and facilitate the engagement between the subsidiary agile teams [Figure 1]. Each agile team contributed within their core specialty to formulate the hospital’s service resumption guidelines. For example, the guideline for surgery service resumption was contributed by a surgery agile team member. The ambulatory care service resumption had a clinician and a nurse involved in ambulatory care. The process of guideline development and implementation was initiated informally on April 2020 and formally on May 2020. However, due to the then little-known nature of the pandemic and the constant flow of new specialty driven information, guideline modifications and implementation continued to evolve for most services until September 2020.
Results
Project 1: Elective service resumption during COVID-19 pandemic
The contribution of the PMT and the agile teams are illustrated in Figure 2, using two teams, the outpatient team and day care utilization team, as examples. The graphs illustrate a comparison between services in 2019 versus 2020, with an apparent dip related to the suspension of the elective services early in the pandemic from March to May 2020. Guidelines were produced and distributed within the hospital to standardize the approach to elective services resumption,7 and shared at a national level to be utilized by other hospitals. Agile approach created flexibility in progress outside formal lines and
formal nominations.
Project 2: Telemedicine clinics during COVID-19 pandemic
Prior to the COVID-19 pandemic, telemedicine use was established in some departments of the hospital through various platforms such as WhatsApp® and Zoom® in addition to email and telephone. The project management team focused on integrating telemedicine clinics into the hospital’s Health Information System (Al Shifa®), while the agile teams actively sought and offered services through online and face to face platforms. During the 2020–2021 Covid-19 pandemic, the use of telemedicine increased [Figure 3]. As the hospital’s telemedicine services gain more public acceptance, new facilities such as interdepartmental collaboration are expected to be added.8
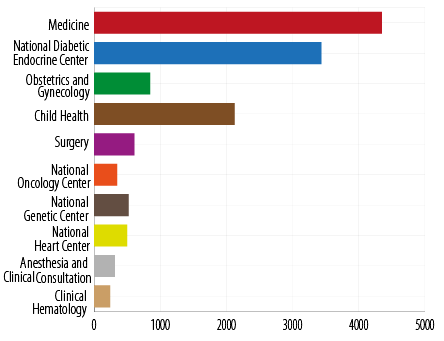
Figure 3: Telemedicine clinic consultation per department during COVID-19 pandemic.
Discussion
We have provided two examples of how the lean and agile approaches can be operationalized within a tertiary healthcare environment. Lean management introduced structured methods to improve performance and processes in which teams work together to eliminate unnecessary steps that were previously executed separately and were vulnerable to delays.
Meanwhile, the agile approach introduces enhancements such as cross-functional teams, which follow the same underlying philosophy as the lean but with more flexibility and smaller work progress goals.7,9 Agile organizations are fast, resilient, adaptable, and are theoretically suited to respond to shocks such as the COVID-19 pandemic.2 The implementation of the lean and agile methods provided practical insights into these management tools and helped us improve the quality of care during the crisis months of the pandemic.10 Our experience was shared with the International Hospital Federation in November 2020 which resulted in the recognition of the Royal Hospital for being “Beyond the call of duty for COVID-19 organizations”.11 Nevertheless, there were challenges such as delays due to COVID-19 infections among members of a few teams.
Conclusion
Early in 2020, the huge inflow of patients affected by the COVID-19 pandemic created an urgent need to upgrade the efficiency and streamline inter-personnel collaboration within the Royal Hospital. It was decided to adopt agile team approach using lean methods. The newly formed agile teams successfully brought together clinical and non-clinical personnel across disciplines and departments to generate a streamlined collaborative system that promoted efficient, effective, and high-quality patient care. The success of this initiative suggests its suitability for healthcare settings elsewhere.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
Acknowledgements
We would like to thank the Royal Hospital teams who participated in this study.
references
- 1. Khamis F, Al-Zakwani I, Al Naamani H, Al Lawati S, Pandak N, Omar MB, et al. Clinical characteristics and outcomes of the first 63 adult patients hospitalized with COVID-19: an experience from Oman. J Infect Public Health 2020 Jul;13(7):906-913.
- 2. Natale JE, Boehmer J, Blumberg DA, Dimitriades C, Hirose S, Kair LR, et al. Interprofessional/interdisciplinary teamwork during the early COVID-19 pandemic: experience from a children’s hospital within an academic health center. J Interprof Care 2020 Sep-Oct;34(5):682-686.
- 3. Tolf S, Nyström ME, Tishelman C, Brommels M, Hansson J. Agile, a guiding principle for health care improvement? Int J Health Care Qual Assur 2015;28(5):468-493.
- 4. Cohen RI. Lean methodology in health care. Chest 2018 Dec;154(6):1448-1454.
- 5. Shakhman LM, Al Omari O, Arulappan J, Wynaden D. Interprofessional education and collaboration: strategies for implementation. Oman Med J 2020 Jul;35(4):e160.
- 6. Ni M, Borsci S, Walne S, Mclister AP, Buckle P, Barlow JG, et al. The lean and agile multi-dimensional process (LAMP) - a new framework for rapid and iterative evidence generation to support health-care technology design and development. Expert Rev Med Devices 2020 Apr;17(4):277-288.
- 7. Kotter J.P. Harvard Business Review (USA), November 2012, Vol. 90 No. 11, Start page: 45, No. of pages: 11.
- 8. Al Kuwaiti A, Al Muhanna FA, Al Amri S. Implementation of digital health technology at academic medical centers in Saudi Arabia. Oman Med J 2018 Sep;33(5):367-373.
- 9. Han J, Zhu L, Wang Y, Zeng Z, Zhang S. Resumption of daily services in a gastroenterology department in Guangzhou, China, in the wake of COVID-19. Lancet Gastroenterol Hepatol 2020 Jul;5(7):645-646.
- 10. Williams SJ. Improving healthcare operations: the application of lean, agile and leagility in care pathway design. Springer; 2017 Jan 16.
- 11. International Hospital Federation. [cited 2021 May 23]. Available from: https://www.ihf-fih.org/beyond-the-call-of-duty-for-covid-19/organizations/.