|
Abstract
Objectives: To assess the results of transit time flowmetry (TTF) on a consecutive group of coronary artery bypass grafting (CABG) patients at Queen Alia Heart Institute.
Methods: Intraoperative flow measurements of a consecutive group of 436 CABG patients. The flow pattern for each coronary artery system was assessed including mean flows, pulsatility index (PI) and the need for revision.
Results: A total of 1394 grafts in 436 patients were assessed (3.2 grafts per patient), wherein 100 grafts showed inadequate flowmetry results (7.2%); most of which were in the circumflex and right coronary artery systems with a percentage of 9.4% and the least in the LAD system with a percentage of 4.4%. The mean flow of grafts to the LAD system was 33.4±5.3 mL/min with a PI of 2.4±0.4; while the mean for grafts to the circumflex artery systemwas 35.1±7.2 mL/min with a PI of 3.5±0.7. The mean for theright coronary artery was 38.4±5.9 mL/min with a PI of 2.6±0.6. Revisions occurred in five patients (1.1%). Suboptimal grafts to the LAD system exhibited a flow of 14.1±7.4 mL/min with a PI of 6.9±1.7. While for the circumflex system a flow of 5.5±3.6 mL/min was reported with a PI of 10.4±7.8; and for the right coronary system a flow of 7.2±5.3 mL/min with a PI of 9.1±5.7 was reported.
Conclusion: Grafts to the LAD system showed the best flowmetry results compared to grafts to the circumflex and right coronary systems. A proportion of poor grafts were revised.
Keywords: Transit Time Flowmetry; CABG; Outcomes.
Introduction
Coronary Artery Bypass Grafting (CABG) is the commonest cardiac surgical operation. Outcomes for CABG have gradually been improving due to quality control measures.1 One of the most critical quality control measures in CABG patients is the assessment of graft patency. A simple method to achieve this is transit time flowmetry (TTF), in which two piezoelectric crystals transmitting ultrasound through the blood vessel towards a reflector on the other side of the vessel, then volume flow is calculated by measuring the difference between transit times upstream and downstream in the blood vessel.2 Transit time flowmetry measures mean flows, diastolic filling (DF), and pulsatility index (PI). PI is calculated using the following formula:
PI = (maximum volumetric peak flow – minimum volumetric peak flow
mean volumetric flow.
This study aims to take a real time snap shot of the flow characteristics in consecutive cases of coronary artery bypass surgery patients as well as the adequacy of the flow characteristics of fashioned grafts. The study primarily aims to determine the flows in different coronary artery systems and the incidence of suboptimal flows.
Methods
This study was conducted at the Queen Alia Heart Institute (QAHI) in Amman, Jordan, where a consecutive group of 436 patients undergoing CABG had their flowmetry assessed using a transit time flowmetry machine (MediStim VQ-1101, MediStim; Oslo, Norway). This study was initially conceived as a quality control audit activity in which all CABG patients operated by surgeons in this large cardiac surgery unit (>2000 open heart cases annually) had their flowmetry checked and documented over a five-month period between August 2008 and January 2009. Each patient had their flowmetry results printed. One copy was left in the patient’s clinical notes, while a second copy was collected for analysis for this study. The study involved calculating the mean flow measurements for each coronary system as well as the Pulsatility Index. The study also collected data on the prevalence of suboptimal results. The flows that were considered adequate were ≥20 mL/min for RCA grafts and ≥15 mL/min for left sided grafts. Adequate diastolic filling was accepted above 50% with Pulsatility Index of <5.3
Results
There were a total of 1394 coronary grafts in 436 patients. Table 1 shows the proportion of suboptimal grafts. A total of 1394 grafts in 436 patients were assessed (3.2 grafts per patient), which showed inadequate flow in 100 grafts (7.2%). The left anterior descending (LAD) system which includes, the diagonal coronary artery and ramus intermedius in addition to the LAD, had a total of 602 grafts with suboptimal flow occurring in 28 grafts (4.4%). The circumflex system had 385 grafts with suboptimal flows in 40 grafts (9.4%).
Table 1: Proportion of suboptimal grafts.
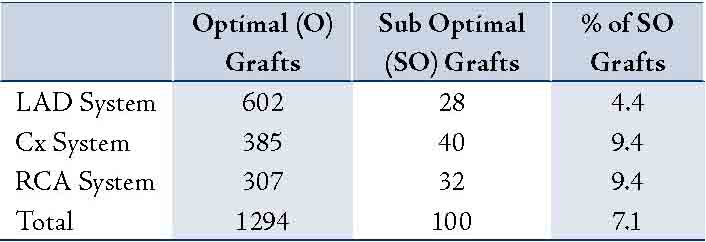
LAD: Left Anterior Descending Artery; Cx: Circumflex Coronary Artery; RCA: Right Coronary Artery.
The right coronary artery (RCA) system had 307 grafts of which 32 were suboptimal (9.4%). Table 2 summarizes the results of the mean flows and PI of grafts deemed adequate in the different coronary systems. The mean flow of grafts for the LAD system was 33.4±5.3 mL/min with a PI of 2.4±0.4. While for the circumflex coronary artery system, a flow of 35.1±7.2 mL/min with a PI of 3.5±0.7 was observed and a flow of 38.4±5.9 mL/min with a PI of 2.6±0.6 was reported for the right coronary artery. Table 3 illustrates the results of flows in suboptimal grafts.
Table 2: Mean flows and PI.
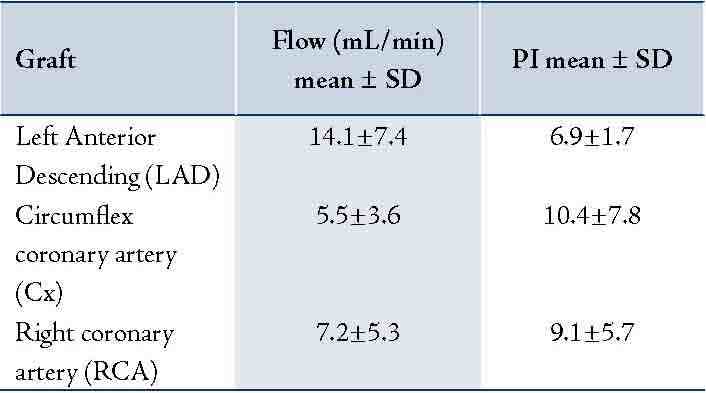
Table 3: Flow and PI in suboptimal grafts
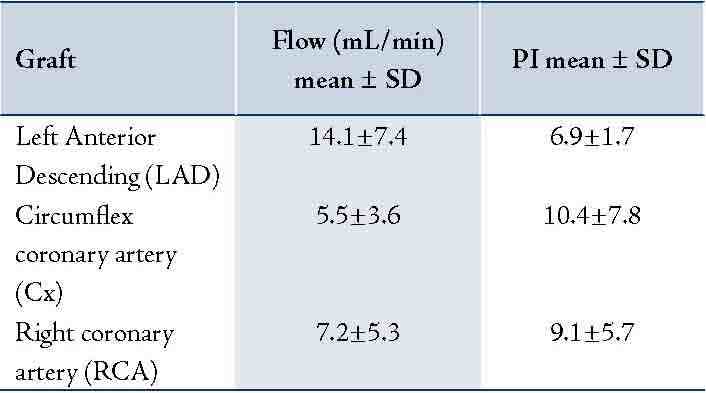
Suboptimal grafts to the LAD system exhibited a flow of 14.1±7.4 mL/min with a PI of 6.9±1.7, a flow of 5.5±3.6 mL/min with a PI of 10.4±7.8 for the circumflex system, and for the right coronary system a flow of 7.2±5.3 mL/min with a PI of 9.1±5.7.
Discussion
Due to the seriousness of the consequences of having inadequate graft flow in patients undergoing CABG, intraoperative graft assessment was introduced. Currently, transit time flowmetry is the commonest intraoperative method of graft assessment. This technology is convenient, valid and reproducible in clinical practice.3 It has to be stated that with regards to quality control measures in CABG, intraoperative angiography is the gold standard, but because of logistical difficulties in obtaining this in many hospitals, transit time flowmetry (TTF) gained popularity and remains a quick examination with readily obtainable results.
In this study, there was a 7.2% failure rate which is comparable to published data. D'Ancona reported on a large series of transit time flowmetry-checked grafts and detected a 9.9% failure rate. Out of 32 grafts revised, six (19%) were found to be obstructed, nine (28%) showed minimal stenosis, 12 (37%) had some problem in the native coronary vessel, and in five cases (16%), there was a kinked conduit or an artery dissection.4
While Di Giammarco reported on 304 grafts in 157 patients submitted to intraoperative TTF and postoperative angiography at a mean follow-up of 6.7±4.8 months from the operation.5 They found that peak flow, mean graft flow (MGF), and PI were independent predictors of graft failure. They also found that mean graft flow (MGF) <15 mL/min and PI >3 were more accurate predictors for short-term negative outcomes. In addition, they reported that more than 50% of failing grafts in their experience had to be considered as functional occlusion with the feature of low MGF with very high PI.5
It has to be stated that there is evidence to suggest that transit time flowmetry technology is not 100% fail safe as there are issues with sensitivity and specificity.6 In a study on 261 grafts, it was found that early angiography demonstrated a 5.4% occluded grafts despite having adequate intraoperative flowmetry results.7 One of the factors the authors found that had contributed to late occlusion was flow in the native coronary artery.7 These grafts were patent at the time of surgery; but at midterm angiography, a proportion were found to be occluded.
In another study looking at angiography after CABG, at midterm, it was found that one of the main reasons for graft failure was anastomosing a graft to a mildly stenosed coronary artery. These grafts have adequate intraoperative flowmetry results but fail in the medium term due to significant competitive native coronary blood flow.8 There is evidence to suggest that the best predictor of early graft failure is a high PI,7 whereas late graft failure is associated with low mean flows primarily.8,9
Concerning mid and late term graft patency prediction and clinical outcomes, there is limited evidence to suggest that patients could benefit from this intraoperative method, but this may change once results of long term studies are reported in the future. With regards to revisions, only 1% of grafts in this study were revised solely on the basis of flowmetry results.
There is a wide variation in the literature with regards to the proportion of grafts needing revisions.9 It seems that more grafts that were done off pump needed revisions compared to grafts performed on cardiopulmonary bypass.10 In this current study, all grafts were performed on cardiopulmonary bypass.
This study which was conceived as an audit exercise and provides a snapshot of the current practice in a large cardiac surgical unit in Jordan. The universal use of flowmetry in all patients is believed not only to improve outcomes in the patients undergoing surgery at this time but also as a teaching tool for all surgeons, and especially surgeons in training. As for the limitations of the study, this is an observational study and therefore it was not randomized with the inherent risks associated. Although the study included all newcomer CABG cases, there is no fail proof mechanism to assure that all grafts performed had their flowmetry checked and printed.
Conclusion
Grafts to the LAD system showed the least percentage of poor flowmetry results while grafts to the circumflex and right coronary artery exhibited the most. A small proportion of patients had revisions of the grafts solely based on their flowmetry results.
Acknowledgements
I wish to thank my colleagues in Cardiac Surgery at Queen Alia Heart Institute (QAHI) as well operating room staff for their help in the collection of data for this study. No conflicts of interest to declare on the materials presented in this manuscript whether financial or personnel.
References
1. Beldi G, Bosshard A, Hess OM, Althaus U, Walpoth BH. Transit time flow measurement: experimental validation and comparison of three different systems. Ann Thorac Surg 2000;70:212-217.
2. Håvard B. Nordgaard, Nicola Vitale, Rafael Astudillo, Attilio Renzulli, Pål Romundstad, Rune Haaverstad. Pulsatility index variations using two different transit time flow meters in coronary artery bypass surgery. Eur J Cardiothorac Surg 2010;37:1063-1067.
3. Hassanein W, Albert AA, Arnrich B, Walter J, Ennker IC, Rosendahl U, Bauer S, Ennker J. Intra-operative transit time flow measurement: Off-pump versus on-pump coronary artery bypass. Ann Thorac Surg 2005;80:2155-2161.
4. D'Ancona G, Karamanoukian HL, Salerno TA, Schmid S, Bergsland J. Flow measurement in coronary surgery. The Heart Surgery Forum 1999;2:121-124.
5. Di Giammarco G, Pano M, Cirmeni S, Pelini P, Vitolla G, Di Mauro M. Predictive value of intraoperative transit-time flow measurement for short-term graft patency in coronary surgery. J Thorac Cardiovasc Surg 2006;132:468-474.
6. D'Ancona G, Karamanoukian HL, Ricci M, Schmid S, Bergsland J, Salerno TA. Graft revision after transit time flow measurement in off-pump coronary artery bypass grafting. Eur J Cardio Thorac Surg 2000;17:287-293.
7. Tokuda Y, Song MH, Oshima H, Usui A, Ueda Y. Predicting midterm coronary artery bypass graft failure by intraoperative transit time flow measurement. Ann Thorac Surg 2008;86:532-536.
8. Manabe S, Fukui T, Shimokawa T, et al. Increased graft occlusion or string sign in composite arterial grafting for mildly stenosed target vessels Ann Thorac Surg 2010;89:683-687.
9. Kieser TM, Rose S, Kowalewski R, Belenkie I. Transit time flow predicts outcomes in coronary artery bypass graft patients: a series of 1000 consecutive arterial grafts. Eur J Cardiothorac Surg, August 2010;38(2):155-162.
10. Sugimura Y, Toyama M, Katoh M, Kotani M, Kato Y, Hisamoto K. Outcome of composite arterial Kotani M, Kato Y, Hisamoto K. Outcome of composite arterial Y-grafts in off pump coronary artery bypass. Asian Cardiovasc Thorac Ann, 2011;19(2):119-122.
|