ABO blood group is known to be the most important blood group in transfusion medicine. The presence of A antigen, B antigen as well as H antigen (O as amorph) on the red blood cells are controlled by few genes (i.e. the FUT1 (H) gene, ABO gene, and FUT2 (SE) gene). Bombay phenotype was first described in 1952 in Bombay (now known as Mumbai), India. Only about 4 per million of the world population presented with Bombay (Oh) phenotype.1 Classical Bombay individual is known to have no H antigen, A antigen, or B antigen on the red blood cells and are non-secretors. Para-Bombay, or H-deficient phenotype is another classification under Bombay phenotype. Individuals with this phenotype may carry small amounts of H antigens on the red blood cells or the red blood cells can be devoid of the H antigen. Those antibodies present in para-Bombay individual may be different when compared to the classical Bombay phenotype.
Case report
A 31-year-old with no known medical illness primigravida presented to a teaching hospital in the East Coast of Malaysia for premature delivery at 25 weeks gestation. Her antenatal follow-up was labelled as group O Rh D positive, where the blood grouping was done using an automated gel card and no antibody screening was performed. She delivered a premature baby girl via spontaneous vertex delivery. She had retained the placenta during delivery and manual removal of placenta was performed. Estimated blood loss was 500 mL. Her hemoglobin (Hb) dropped from 11 g/dL predelivery to 10.3 g/dL postdelivery. No blood was required for the mother.
Table 1: Tests performed for identification of mother’s blood group in an East Coast
tertiary hospital.
|
Forward grouping1 |
|
Anti-A |
0 |
O Rh D positive |
|
Anti-B |
0 |
|
|
Anti-A,B |
0 |
|
|
Anti-D |
4+ |
|
|
Reverse grouping2 |
|
|
|
A cells |
4+ |
Presence of extra antibodies |
|
B cells |
4+ |
|
|
O cells |
2+ |
|
|
Antibody screening |
1+ (all 3 panels)
Autocontrol: negative |
|
|
Antibody identification (11 panels) |
|
Normal panels |
0 |
Antibody only detected in enzyme- enhanced panels |
Note: reaction for all tests ranged from 0 (no reaction) to 4+ (strongest reaction).
1Forward grouping: testing of known serum (anti-A, anti-B, anti-A,B, and anti-D) with patient’s red cells.
2Reverse grouping: testing of patient’s serum with known cells (A cells, B cells, and O cells).
The newborn was intubated in the neonatal intensive care unit. On day six of life, the baby became tachycardic and desaturated with Hb of 11.1 g/dL. The baby was grouped as O Rh D positive in forward grouping. Blood crossmatching was performed using mother’s serum. There was an ABO discrepancy discovered in the mother’s blood grouping result [Table 1]. The father’s blood group is A Rh D positive. This is non-consanguineous marriage. Due to the urgent need transfusion, baby’s blood was used for crossmatching instead of the mother’s sample as the discrepancy was not yet resolved. At that point of time, it was suspected that the mother might be para-Bombay. In view of post-partum and mother’s Hb level (10.3 g/dL) was insufficient for blood donation, the mother’s blood was not used. Group O packed cells were found to be compatible with the baby’s sample. However, baby’s Hb did not pick up (12 g/dL at day 11 of life) despite transfusing 15 mL group O red cells twice (baby’s weight was 900 gram), with no other bleeding sources observed. It was suspected that the baby might be para-Bombay. If the baby was group O, we were concerned that the alloantibodies (anti-H) may have been passively transferred to the baby. Even though the anti-H is generally immunoglobulin (Ig) M, taking into consideration baby’s premature condition and the nature of antibody is not known, decision was made to supply Bombay or para-Bombay blood group to the baby. The case was referred to National Blood Centre (NBC) as the main reference laboratory and urgent search of Bombay blood.
Mother’s blood sample and saliva sample were sent to NBC for further investigation [Table 2]. The mother was concluded as para-Bombay A with anti-IH. Due to the rarity of para-Bombay A and urgency of blood needed for her baby, leucodepleted and irradiated Bombay blood was supplied. Further testing for blood group confirmation of the baby will be done after the baby is one year old [Figure 1].
Table 2: Tests performed for identification of mother’s blood group in the National Blood Centre.
|
Forward grouping1 |
|
Anti-A |
0 |
O Rh D positive |
|
Anti-B |
0 |
|
|
Anti-A,B |
0 |
|
|
Anti-D |
4+ |
|
|
Anti-H |
0 |
H antigen negative |
|
Reverse grouping2 |
|
A cells |
4+ |
Presence of extra antibodies |
|
B cells |
4+ |
|
|
O cells |
4+ |
|
|
Direct antiglobulin test |
0 |
|
|
Antibody screening |
0 |
|
|
Antibody identification (11 panels) |
|
|
|
Normal panels |
0 (for all 11 panels) |
Antibody only detected in enzyme-enhanced panels |
|
Enzyme-enhanced panels |
Panagglutination (1+)
(for all 11 panels) |
|
Absorption elution test |
|
A cell |
3+ |
A and H antigen present on patient’s red cells |
|
B cell |
0 |
|
|
O cell |
2+ |
|
|
Secretor status (saliva test) |
|
A cells |
0 |
A and H substance present in saliva |
|
B cells |
4+ |
|
|
O cells |
0 |
|
|
Additional tests |
|
Adult O cells |
4+ |
Antibody reacting with I antigen |
Note: reaction for all tests ranged from 0 (no reaction) to 4+ (strongest reaction).
1Forward grouping: testing of known serum (anti-A, anti-B, anti-A,B, and anti-D) with patient’s red cells.
2Reverse grouping: testing of patient’s serum with known cells (A cells, B cells, and O cells).
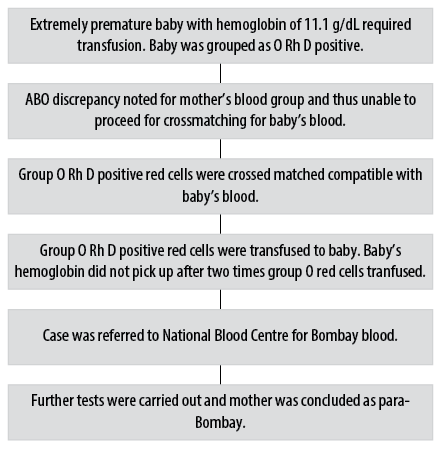
Figure 1: Flow of case summary.
Discussion
Bombay phenotype is a rare phenotype, present in about 4 per million of the human population. Some population in Mumbai may have higher incidence of 1 in 10 000.1 These cases were also reported in other countries such as Taiwan and Thailand.2,3 In Malaysia, there were cases of Bombay phenotype donors recruited into our National Registry for Rare Blood Donors Database.4
Para-Bombay is a rare RBC phenotype and only limited cases are reported worldwide. The reported ratio of para-Bombay to Bombay phenotype was 1:15.5 The weak or no reaction in forward grouping made the ABO grouping challenging in identifying the para-Bombay phenotype. In this case, the mother was grouped as O using manual method, which did not include O cell in reverse grouping during antenatal follow-up. The mother’s blood was incompatible with group O red cells. It showed the significance of anti-IH in this patient. If urgent blood is needed, the mother might be transfused with Safe O, where it may cause extensive hemolysis in this patient.
The anti-IH present in para-Bombay individuals can be weak or undetectable during screening. The antibody screening was negative in NBC but weak positive in the tertiary hospital. Given the contradicting screening outcomes, it was difficult to identify the exact antibody when urgent blood was needed during delivery with retained placenta. This also hindered the blood supply for the premature baby. Direct antiglobulin test (DAT) of the baby was negative and thus Intravenous (IV) Ig was not recommended. IVIg should be recommended for DAT positive infants.6 Group O packed cells were crossmatched and found to be incompatible with the mother’s blood. Further crossmatching using baby’s serum was performed because anti-H/anti-IH were usually IgM and could not permeate through placenta. However, the baby in this case had reduced Hb level post group O packed cells transfusion, which could be due to the prematurity of the baby. Alternatively, the anti-IH may consist certain amount of IgG that were being transferred through placenta to the baby but was not picked up during crossmatching with group O packed cells. Passive antibody may occur in second trimester and can cause hemolysis in baby.6 Due to the rarity of para-Bombay and uncertainty of baby’s blood group, Bombay blood was transfused to this baby. In the NBC, Bombay blood is available in frozen stock. However, in view of the baby’s condition, Bombay donor was contacted to obtain compatible fresh Bombay blood after crossmatching with mother’s serum. This highlighted the importance of rare donor registry in the management of transfusion for rare blood phenotype patient.4,6,7
Review of literature concerning blood transfusion among para-Bombay individuals showed that group O cells were well tolerated with appropriated Hb increment and hematocrit respond.8,9 More recent review showed no increased risk of hemolytic disease of fetus and newborn (HDFN).10 Anti-IH tended to give stronger reaction than anti-H in indirect globulin test.11 In this case report, the baby required transfusion due to extreme prematurity and its associated complications. However, HDFN could not be excluded completely in this baby.
The procedure of ABO grouping for pregnant mother during booking currently is not standardized, depending on different centers. Current setting only includes ABO and Rh grouping12 but no antibody screening. Red cell antibody may develop after exposure to blood transfusion, pregnancy, and transplant. Antibody screening can be added into antenatal booking procedure to detect unexpected antibodies earlier during pregnancy and subsequently facilitate the process of blood supply. Early recognition of rare phenotype is important to ensure appropriate blood management for the pregnant mother. Family screening can be done to identify compatible blood in advance for rare blood phenotype.7 Optimization of Hb level antenatally and a well delivery plan should be provided for para-Bombay mothers. Additionally, we recommend autologous blood donation for frozen stock during early pregnancy. Pediatrician should be informed in advance of para-Bombay delivery, so that they can standby for emergency delivery and resuscitation if HDFN occurred.
Conclusion
Para-Bombay A is an extremely rare phenotype which usually mislabeled as O when O cells were absent in reverse grouping. Additional tests may be required during antenatal follow-up to prevent complications during delivery or emergency.
Disclosure
The authors declared no conflicts of interest. Before drafting of the case report, the purpose of the case report was explained in detail and informed consent was obtained from the patient, where anonymity is ensured.
Acknowledgements
We would like to thank the Director General of Health Malaysia for his permission to publish this article. We thanked Dr. Noryati Abu Amin, Director of National Blood Centre (NBC), Malaysia for her administrative support of this work. We would like to thank Dr. Rapiaah Mustaffa for referring this case to NBC. Thanks to all the transfusion medicine specialists, medical officers, and immunohematology staff in NBC. We appreciate the assistance by all the staff in the Department of Hematology and Transfusion Medicine Unit, School of Medical Sciences, Universiti Sains Malaysia.
references
- 1. Dean L. Blood groups and red cells antigens. National Center for Biotechnology Information (US); 2005.
- 2. Lin-Chu M, Broadberry RE, Tsai SJ. Incidence of ABO subgroups in Chinese in Taiwan. Transfusion 1987a Jan-Feb;27(1):114-115.
- 3. Lin-Chu M, Broadberry RE, Tsai SJ, Chiou PW. The para-Bombay phenotype in Chinese persons. Transfusion 1987b Sep-Oct;27(5):388-390.
- 4. Ahmad NH, Musa RH, Muniandi G, Yaakob NA, Yusoff WN, Choo R, et al. Rare donor registry in National Blood Centre. Poster presented at: 24th regional congress of the International Society of Blood Transfusion in conjunction with the 6th Malaysian national transfusion medicine conference; 2013 December 1-4; Kuala Lumpur, Malaysia.
- Bhatia HM, Sathe MS. Incidence of “Bombay” (Oh) phenotype and weaker variants of A and B antigen in Bombay (India). Vox Sang 1974;27(6):524-532.
- Shastry S, Lewis LE, Bhat SS. A rare case of haemolytic disease of newborn with Bombay phenotype mother. Asian J Transfus Sci 2013 Jul;7(2):153-155.
- Bhattacharya S, Makar Y, Laycock RA, Gooch A, Poole J, Hadley A. Outcome of consecutive pregnancies in a patient with Bombay (Oh) blood group. Transfus Med 2002 Dec;12(6):379-382.
- Light J, Wenk RE, Greenwell P. “Unclassifiable” weak A blood group and deficient H phenotype (Hm) in one pedigree: variants of A and H types in a family. Clin Genet 1987 Jan;31(1):7-12.
- 9. Shih MC, Jen IM, Hwang DH, Lee MT, Shu CW. Blood transfusion in patients with the paraBombay phenotype-2 case reports. Annual Meeting of Hematology Society ROC and Chinese Society of Blood Transfusion;1988. p. 31.
- Bullock T, Win N, Jackson B, Sivarajan S, Penny J, Mir N. Bombay phenotype (Oh ) and high-titer anti-H in pregnancy: two case reports and a review of the literature. Transfusion 2018 Dec;58(12):2766-2772.
- 11. Lin-Chu M, Broadberry RE. Blood transfusion in the para-Bombay phenotype. Br J Haematol 1990 Aug;75(4):568-572.
- 12. Family Health Development Division, Ministry of Health Malaysia. Perinatal Care Manual 3rd edition. [cited 2020 May]. Available from: http://fh.moh.gov.my/v3/index.php/component/jdownloads/download/18-sektor-kesihatan-ibu/224-perinatal-care-manual-3rd-edition-2013.