Superior vena cava (SVC) syndrome is a relatively common clinical condition. However, SVC syndrome as the presenting feature of systemic lupus erythematosus (SLE) is very uncommon. It is even rarer in SLE in the absence of antiphospholipid syndrome (APS). Thrombosis as a clinical manifestation of SLE accounts for 15% of cases. Among them, venous thrombosis accounts for 10%, while the rest is due to arterial thrombosis.1 We report a rare and interesting case of SVC thrombosis due to SLE without APS.
Case report
A 20-years-old married woman was admitted to the Department of General Medicine at RG Kar Medical College, Kolkata, in 2018 with the complaint of recent onset swelling of face and neck accompanied by polyarthralgia and constitutional symptoms for two weeks. There was no chest pain, cough, or hemoptysis; but she was mildly short of breath. There was no history of photosensitivity, rash, oral ulcers, alopecia, oliguria, hematuria, or Raynaud’s phenomenon. She had no history of any spontaneous pregnancy loss, nor did she use any oral contraception.
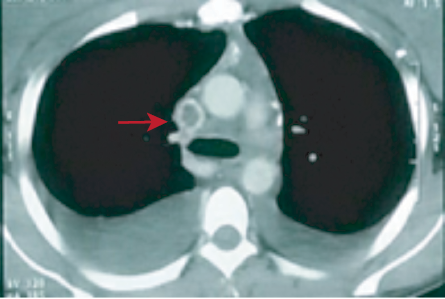
Figure 1: Contrast-enhanced computed tomography thorax showing superior vena cava thrombus.
Table 1: Summary of relevant laboratory investigations.
|
Hemoglobin |
12.9 |
12–16 g/dL |
|
WBC |
7800 |
4000–11 000/μL |
|
Platelet count |
2.9 |
1.5–4.5 lakh/ μL |
|
Creatinine |
96 |
59–104 umol/L |
|
ESR |
42 |
< 20 mm
(first hour) |
|
CRP |
0.7 |
Up to 0.8 mg/dL |
|
Serum protein |
7 |
6.6–8.3 g/dL |
|
Serum LDH |
204 |
< 248 U/L |
|
PT |
11 (INR-1) |
11 seconds |
|
APTT |
36 |
30–40 seconds |
|
Urine ACR |
24 |
< 30 |
|
Pleural fluid protein |
4.9 |
1–2 g/dL |
|
ANA(Hep2 method) |
Positive 1:320 titer speckled pattern |
- |
|
Anti-ribosomal P |
+++ |
0 Negative |
| |
|
(+) Borderline |
| |
|
+ Positive |
| |
|
++Positive |
| |
|
+++Strongly positive |
|
Complement C3 |
26 mg/dL |
90–180 mg/dL |
|
Anti-beta2-glycoprotein and antiphospholipid antibody |
Negative |
|
WBC: white blood cells; ESR: erythrocyte sedimentation rate;
CRP: C-reactive protein; LDH: lactate dehydrogenase; PT: prothrombin time; INR: international normalized ratio; APTT: activated partial thromboplastin time; ACR: albumin-creatinine ratio; ANA: antinuclear antibody;
DCT: direct Coombs test.
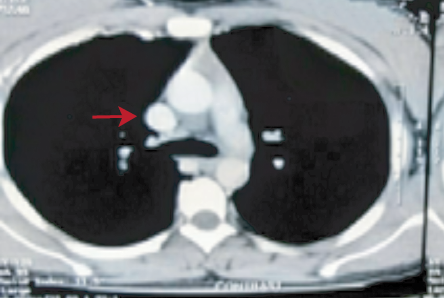
Figure 2: Contrast-enhanced computed tomography thorax showing resolution of thrombus after successful treatment.
On examination, she was pale and had generalized lymphadenopathy involving the cervical, axillary, and inguinal areas. Face and anterior part of neck appeared swollen with non-pulsatile and raised jugular venous pressure. Her temperature was mildly raised (37.6 °C) with tachycardia but no tachypnea. Respiratory system examination revealed bilateral dull percussion notes along with diminished breath sounds in both lung bases. Her liver and spleen were non-palpable, and the rest of the systemic examinations were within normal limits. Blood counts, renal function tests, and liver function tests were normal. Erythrocyte sedimentation rate was mildly raised with normal C-reactive protein. Prothrombin time and activated partial thromboplastin time were normal. Urine examination showed normal albumin-creatinine ratio without any active sediments. Bilateral exudative pleural effusion was present with a normal level of adenosine deaminase and negative nucleic acid amplification tests for Mycobacterium tuberculosis. Lymph node biopsy showed features of reactive hyperplasia. Contrast-enhanced computed tomography of the thorax revealed SVC thrombus with bilateral pleural effusion [Figure 1].
Transthoracic echocardiography showed a thrombus extending from the SVC to the right atrium. Antinuclear antibody (ANA) was positive in 1:320 titer (Hep2 method) with a speckled pattern. Extractable nuclear antigen profile was suggestive of strongly positive anti-ribosomal P antibody.
Complement C3 level was low. Direct Coomb test was positive. Anti-beta2-glycoprotein and antiphospholipid antibodies were negative. A summary of the results of her laboratory tests is shown in Table 1.
Based on the clinical and laboratory findings, the patient was diagnosed with SLE with SVC thrombosis. She was treated with oral steroids (prednisolone 1 mg/kg body weight), hydroxychloroquine, and subcutaneous low molecular weight heparin with oral anticoagulant. Complete resolution of intracardiac and SVC thrombus was documented within two weeks with significant improvement in her symptoms [Figure 2]. The patient is still being followed-up in our outpatient department. She is on oral anticoagulant with regular monitoring of prothrombin time and markers of lupus flare.
Discussion
SLE is a prothrombotic condition, and several factors in the form of platelet hyperfunction, lupus nephritis, elevated homocysteine, the presence of antiphospholipid antibodies, and high disease activity are thought to be responsible.2,3 Inflammation is the main risk factor for venous thrombosis in SLE without APS by affecting multiple steps of blood coagulation like initiation, propagation, and regulation.4 Inflammation can also initiate thrombosis by different mechanisms like the expression of tissue factors, decreasing the fibrinolytic activity by upregulating the production of plasminogen activator inhibitor, downregulation of thrombomodulin, and a decrease of protein S. Activation of the complement factors along with an increase in proinflammatory cytokines occur in active lupus which can aggravate thrombosis.5 Independent risk factors like elevated plasma homocysteine level lead to atherosclerosis, arterial, and venous thrombosis.6 Diabetes mellitus, hypertension, and dyslipidemia are seen in SLE patients, along with glucocorticoids, which are commonly used for the management, play a key role in the formation of thrombosis, as elaborated in numerous studies.7
Malignancy is the most common cause (responsible for > 90% of the cases) of SVC syndrome. A few cases of SVC syndrome have been reported in association with connective tissue disorders or vasculitis. SVC thrombosis is an uncommon but well-recognized manifestation of Behçet’s disease.8 Behçet’s disease has also been reported to be associated with narrowing of SVC lumen due to vasculopathy without thrombosis.9 SVC syndrome due to intravascular thrombosis has been reported in a patient with rheumatoid arthritis (RA) without APS indicating that RA itself may be the cause of hypercoagulable state in that case.10 A case of SVC syndrome in a patient of SLE with longstanding classic RA was reported where the etiology was external compression of SVC by mediastinal lymphadenopathy.11 A similar case was also reported by Kingetsu et al,12 SVC syndrome (caused by thrombosis) as a presenting feature of SLE is comparatively rare and whatever few cases are reported to date are all cases of lupus associated with APS.13,14 A case of SLE associated with anticardiolipin antibodies presenting as SVC syndrome has been reported previously.13 The 19-year-old woman described in this report had thrombotic occlusion of SVC, which successfully responded to immunosuppressives and intravenous thrombolytics. Similarly, another case of asymptomatic SVC thrombosis as a manifestation of SLE with APS (also known as secondary APS) in a 34-year-old woman with recurrent spontaneous abortions and hemolytic anemia has been reported.14 This patient had no overt signs of SVC obstruction due to the development of collateral vessels. Moreover, SVC thrombosis has also been reported in association with drug-induced lupus with circulating anticoagulants.15 Primary APS has been reported to be associated with SVC thrombosis in the literature.16–18
However, our case of SVC syndrome as a presenting feature of SLE without associated APS is probably the first case globally.
Conclusion
SVC obstruction due to thrombosis, as a presenting feature in a young female with SLE, is relatively rare. It does not always indicate associated APS, as SLE itself is a highly prothrombotic state. Connective tissue disorders have a wide spectrum of presentations and protean manifestations. Hence, a high degree of suspicion is required while evaluating these cases. SVC obstruction is not an uncommon clinical entity, but the determination of the underlying pathophysiology and adjusting the therapy accordingly may be challenging at times.
Disclosure
The authors declared no conflicts of interest. Written informed consent was obtained from the patient and her kin.
references
- 1. Hahn BH. Systemic lupus erythematosus. Harrison’s principles of internal medicine. 20th ed. 2018. p. 2515-2520.
- 2. Sallai KK, Nagy E, Bodó I, Mohl A, Gergely P. Thrombosis risk in systemic lupus erythematosus: the role of thrombophilic risk factors. Scand J Rheumatol 2007 May-Jun;36(3):198-205.
- 3. Dhar JP, Andersen J, Essenmacher L, Ager J, Bentley G, Sokol RJ. Thrombophilic patterns of coagulation factors in lupus. Lupus 2009 Apr;18(5):400-406.
- 4. Sailer T, Vormittag R, Pabinger I, Vukovich T, Lehr S, Quehenberger P, et al. Inflammation in patients with lupus anticoagulant and implications for thrombosis. J Rheumatol 2005 Mar;32(3):462-468.
- 5. Frieri M. Accelerated atherosclerosis in systemic lupus erythematosus: role of proinflammatory cytokines and therapeutic approaches. Curr Allergy Asthma Rep 2012 Feb;12(1):25-32.
- 6. den Heijer M, Keijzer MB. Hyperhomocysteinemia as a risk factor for venous thrombosis. Clin Chem Lab Med 2001 Aug;39(8):710-713.
- 7. Calvo-Alén J, Toloza SM, Fernández M, Bastian HM, Fessler BJ, Roseman JM, et al; LUMINA Study Group. Systemic lupus erythematosus in a multiethnic US cohort (LUMINA). XXV. Smoking, older age, disease activity, lupus anticoagulant, and glucocorticoid dose as risk factors for the occurrence of venous thrombosis in lupus patients. Arthritis Rheum 2005 Jul;52(7):2060-2068.
- 8. Sarr SA, Fall PD, Mboup MC, Dia K, Bodian M, Jobe M. Superior vena cava syndrome revealing a Behçet’s disease. Thromb J2015;13(1):7.
- 9. de Paiva TFJr, Ribeiro HB, Campanholo CB, Gonçalves CR, Terigoe DY, de Souza BD. Behçet’s disease associated with superior vena cava syndrome without thrombosis.Clin Rheumatol 2007 May;26(5):804-806.
- 10. Pramila D, Jayeeta B, Dinesh D. Superior vena cava syndrome due to intravascular thrombosis in a patient with rheumatoid arthritis without antiphospholipid antibody syndrome: is rheumatoid arthritis a separate hypercoagulable state?. Russian Open Medical Journal 2014;3(1).
- 11. van den Brink H, Vroom TM, van de Laar MA, van Soesbergen RM, van der Korst JK. Superior vena cava syndrome caused by systemic lupus erythematosus in a patient with longstanding rheumatoid arthritis. J Rheumatol 1990 Feb;17(2):240-243.
- 12. Kingetsu I, Kurosaka D, Hashimoto N, Tajima N. [A case of systemic lupus erythematosus associated with superior vena cava syndrome]. Nihon Rinsho Meneki Gakkai Kaishi 2000 Jun;23(3):192-199.
- 13. Erdem Y, Haznedaroğlu IC, Oymak O, Yalçin AU, Yasavul Ü, Turgan Ç, et al. Systemic lupus erythematosus presenting as superior vena cava syndrome associated with anticardiolipin antibodies. Clin Appl Thromb Hemost 1996;2(4):289-291.
- 14. Bansal P, Agrawal C, Bansal R. Asymptomatic superior vena cava thrombosis as a manifestation of secondary antiphospholipid syndrome in a female presenting with anemia and bad obstetric history. Indian Journal of Medical Specialities 2017;8(1):45-47.
- 15. Steen VD, Ramsey-Goldman R. Phenothiazine-induced systemic lupus erythematosus with superior vena cava syndrome: case report and review of the literature. Arthritis & Rheumatism: Official Journal of the American College of Rheumatology 1988;31(7):923-926.
- 16. Hegazi MO, Mourou M, Hassanien OA. Antiphospholipid syndrome presenting with superior vena cava thrombosis.Iran J Immunol 2009 Jun;6(2):103-106.
- 17. Alcazar-Ramirez JD, Fernández-Nebro A, Abarca M, Salgado F, De Haro-Liger M, Rodríguez-Andreu J, et al. Central vein thrombosis in the antiphospholipid syndrome. Lupus 1997;6(6):549-551.
- 18. Biernacka-Zielinska M, Lipinska J, Szymanska-Kaluza J, Stanczyk J, Smolewska E. Recurrent arterial and venous thrombosis in a 16-year-old boy in the course of primary antiphospholipid syndrome despite treatment with low-molecular-weight heparin: a case report. J Med Case Rep 2013 Aug;7:221.