Coronavirus disease-2019 (COVID-19) is caused by novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which targets the respiratory system. COVID-19 started in China in December 2019 and was declared a pandemic by the World Health Organization (WHO) on 11 March 2020.1 The incubation period is five to six days, and the symptoms are mainly fever, cough, shortness of breath, or loss of smell. The main reported risk factors include age > 65 years or having comorbid conditions such as diabetes mellitus, ischemic heart disease, hypertension, chronic lung disease, and immunosuppression.2,3
Pulmonary tuberculosis (TB) is one of the oldest diseases.4 Mycobacterium tuberculosis is the most common cause of TB worldwide. TB is a contagious disease, and 90% of individuals will develop latent TB after infection.5 Diabetes mellitus, immunosuppression, underlying chronic lung diseases, and HIV are among the risk factors to develop active TB disease.6
During the COVID-19 pandemic, several respiratory pathogens coinfections were reported, including bacterial and fungal pathogens. About 50% of the patients who died from COVID-19 had secondary respiratory infections.7 A multination study found that 49 patients had TB and COVID-19 coinfection, 85% of the patients had active TB, and 18% of the cohort had a diagnosis of TB and COVID-19 in the same period.8 A report from Italy cited 20 cases of TB and COVID-19 coinfection; 95% had pulmonary TB, and one patient had disseminated TB.9 A recent report from Qatar of six cases with COVID-19 and TB coinfection reported all cases in middle-aged men. None of the patients had a known history of direct exposure to TB; however, all were of south-Asian descent where TB is endemic. All had pulmonary TB, and one had pulmonary and pleural TB.10 Here, we report two cases of pulmonary TB and COVID-19 coinfection in Oman. To the best of our knowledge, there is only one prior published case report in the Middle East and North Africa region.10
Case reports
Case one
A 56-year-old Omani man who is an active smoker and known to have hypertension and diabetes mellitus presented with a three-month history of productive cough with whitish sputum for which he did not seek any medical attention. The patient developed a high-grade fever associated with a sore throat, flu-like symptoms, and headache three days before admission. He had no hemoptysis, shortness of breath, chest discomfort, weight loss or night sweats, and no travel history or contact with sick patients.
On physical examination, the patient was febrile with a temperature of 39.2 ºC and tachypneic with a respiratory rate of 26 breaths/min. His heart rate was ranging between 80–90 beats/min, and his blood pressure was normal. He did not have any palpable cervical or axillary lymphadenopathy. His chest examination revealed bilateral equal air entry with bronchial breathing in the right upper lung.
The chest X-ray showed a thick wall cavitary lesion in the right upper lung zone associated with surrounding innumerable nodular opacities. In addition, in the right lower lung zone there was ill-defined airspace opacity with a subtle nodularity. Findings were highly suggestive of pulmonary TB [Figure 1].
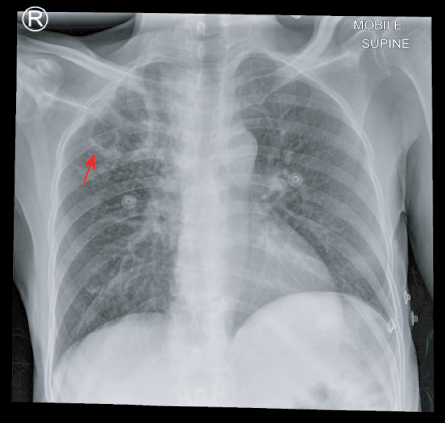
Figure 1: Frontal chest X-ray of the lung showing a thick wall cavitary lesion (red arrow) in the right upper zone associated with surrounding innumerable 1–2 mm nodular opacities. In addition, there is ill-defined airspace opacity with a subtle nodule in the right lower zone.

Figure 2: Frontal chest X-ray showing a diffuse nodular pattern along with airspace opacities involving all the right lung. In addition, there is left upper lung zone airspace opacity along with subtle nodularity.
The patient was empirically treated as per the national clinical management for COVID-19 guideline with ceftriaxone, clarithromycin, and oseltamivir. Nasopharyngeal SARS-CoV-2 polymerase chain reaction (PCR test, sputum for M. tuberculosis PCR (MTB/RIF GeneXpert Cepheid-PCR), and sputum for TB cultures were all performed and tested positive. The patient’s white blood cell count was 7.2 × 109/L (2.2–10), absolute neutrophil count was 4.3 × 109/L (1–5), and absolute lymphocytes count was 1.8 × 109/L (1.2–4). His C-reactive protein (CRP) level was 63.5 mg/L (< 30), erythrocyte sedimentation rate (ESR) was > 130 mm/h (2–25), lactate dehydrogenase level was 128 iU/L (120–246), ferritin level was 514 ug/L (48–708), and cross-linked D-dimer level was 0.44 mg/L (0.1–0.5). He was started on hydroxychloroquine and lopinavir/ritonavir and anti-TB treatment with isoniazid, rifampicin, ethambutol, and pyrazinamide. The patient improved, and he was discharged home to continue anti-TB treatment.
Case two
A 42-years-old non-smoker expatriate man, not known to have any medical background, presented with cough, chest pain, and shortness of breath for three months associated with 4 kg weight loss for which he did not seek any medical treatment. The patient developed a high-grade fever of 39 ºC three days before admission. He had no recent travel outside the country or contact with sick patients. On presentation to the emergency department, he was desaturating on room air with an oxygen saturation (SpO2) of < 90%, that increased to > 95% with 2L of oxygen. He was hypotensive with a blood pressure of 85/50 mmHg. He had dry mucous membranes, and his capillary refill was > 3 sec. His chest examination revealed bilateral coarse crackles greater on the right side. The patient had a negative SARS-CoV-2 PCR test in a local health center. The patient was started on ceftriaxone, clarithromycin, and oseltamivir empirically due to high suspicion of COVID-19 infection.
His chest X-ray showed a diffuse nodular pattern along with airspace opacities involving all the right lung zone. In addition, there was a left upper lung zone airspace opacity along with subtle nodularity involving the left mid-lung zone, findings suggestive of pulmonary TB along with coexisting infection [Figure 2].
The patient’s white blood cells count was 8.1 × 109/L (2.2–10), absolute neutrophils count was 6.5 × 109/L (1–5) initially. He had lymphopenia of 0.5 × 109/L (1.2–4), CRP was 194 mg/L (< 30), and ESR was > 85 mm/h (2–25). A repeat nasopharyngeal SARS-CoV-2 PCR was performed and sputum was collected for MTB/RIF GeneXpert Cepheid-PCR and TB cultures. All were positive. His ferritin level was high at 1170 ug/L (48–708) along with lactate dehydrogenase of 352 iU/L (120–246) and D-dimer of 11.44 mg/L (0.1–0.5). The patient was treated with hydroxychloroquine and anti-TB medications. The patient’s condition improved, and he was discharged home to continue anti-TB treatment.
Discussion
COVID-19 is caused by a novel coronavirus, belonging to the genus Betacoronavirus, and can transmit through human-to-human contact.11 In humans, coronaviruses can cause various respiratory illnesses ranging from the common cold to severe pneumonia, such as SARS-CoV and Middle East respiratory syndrome (MERS). There are few case reports of coinfections between SARS-CoV and MERS-CoV,12–14 and a report from Iran of influenza A virus coinfection.15
We are reporting two cases of COVID-19 and pulmonary TB coinfection. To the best of our knowledge, there are very few reports worldwide. The first reported cases were from China, two of their patients were treated for active TB years before having COVID-19, and now they presented with reactivation of TB. One patient was not treated for TB for > 50 years.16 In the Philippines, 1% of the patients infected with COVID-19 had coinfection with TB, and patients with TB had 2.17 times higher risk of death when compared to those without TB. Additionally, those with TB and COVID-19 coinfection had 25% less risk of recovery than patients without TB.17 In South Africa, around 2128 patients had TB and COVID-19 coinfection out of 22 308 studied. They found that having TB gave a worse outcome compared to non-TB patients.18
In this case report, the first patient was a chronic smoker and was hypertensive and diabetic; all of those could increase the risk of TB. Since his symptoms started in the period when COVID-19 infection started in Oman, his findings are more likely to be coinfection rather than co-incidence. Despite being free of medical background, the other patient was from an area with a high TB burden; hence, it is more likely that he had reactivation
and coinfection.
In 2018, the annual incident rate of TB in Oman was < 5.9 cases per 100 000 population, and 60% of the yearly cases were from non-national citizens.19 It was noted as well from previous MERS-CoV and SARS-CoV that TB and those infections might augment each other and cause immunosuppression,12,20 which might be similar to what happens in SARS-CoV-2. Patients with pulmonary TB may be more susceptible to develop SARS-CoV-2 infection as both could impair the immune system, and this synergism may cause a very severe clinical picture. The authors of one study claimed that pulmonary TB is a major risk factor for COVID-19 infection.21 One of the pathophysiological mechanisms postulated for COVID-19 infection is cytokine storm, and these cytokines play an important role in TB host resistance.22 Another pathophysiological mechanism is that lung damage caused by TB increases the body’s susceptibility to getting other airborne infections such as COVID-19.23
Future studies should look at the impact of TB and COVID-19 coinfection in terms of morbidity and mortality. Furthermore, studies are needed to develop strategies and plans to contain the coinfection and prevent the further spread of both diseases.
Conclusion
COVID-19 is a newly emerged infection that can coexist with other pulmonary infections. M. tuberculosis is a pathogen that can coexist with COVID-19 infection and requires a high clinical suspicion when the chest radiograph suggests pulmonary TB. Early recognition of TB would result in the initiation of appropriate infection control measures and anti-TB therapy. Furthermore, screening all patients admitted with SARS-CoV-2 infection for TB would be important to define the role of COVID-19 in the reactivation of TB. Finally, clearly documented diagnostic and management algorithms should be implemented to improve the outcome from the coinfection.
Disclosure
The authors declared no conflicts of interest. The patient gave consent to publish this case report.
references
- 1. Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun 2020 May;109:102433.
- 2. Khamis F, Al-Zakwani I, Al Naamani H, Al Lawati S, Pandak N, Omar MB, et al. Clinical characteristics and outcomes of the first 63 adult patients hospitalized with COVID-19: An experience from Oman. J Infect Public Health 2020 Jul;13(7):906-913.
- 3. Gandhi RT, Lynch JB, Del Rio C. Mild or Moderate Covid-19. N Engl J Med 2020 Oct;383(18):1757-1766.
- 4. Global tuberculosis report 2018. Geneva: World Health Organization; 2018.
- 5. Yezli S, Memish ZA. Tuberculosis in Saudi Arabia: prevalence and antimicrobial resistance. J Chemother 2012 Feb;24(1):1-5.
- 6. Narasimhan P, Wood J, Macintyre CR, Mathai D. Risk factors for tuberculosis. Pulm Med 2013;2013:828939.
- 7. Cox MJ, Loman N, Bogaert D, O’Grady J. Co-infections: potentially lethal and unexplored in COVID-19. Lancet Microbe 2020 May;1(1):e11.
- 8. Tadolini M, Codecasa LR, García-García J-M, Blanc FX, Borisov S, Alffenaar JW, et al. Active tuberculosis, sequelae and COVID-19 co-infection: first cohort of 49 cases. Eur Respir J 2020 Jul;56(1):2001398 .
- 9. Stochino C, Villa S, Zucchi P, Parravicini P, Gori A, Raviglione MC. Clinical characteristics of COVID-19 and active tuberculosis co-infection in an Italian reference hospital. Eur Respir J 2020 Jul;56(1):2001708.
- 10. Yousaf Z, Khan AA, Chaudhary HA, Mushtaq K, Parengal J, Aboukamar M, et al. Cavitary pulmonary tuberculosis with COVID-19 coinfection. IDCases 2020;22:e00973.
- 11. Shereen MA, Khan S, Kazmi A, Bashir N, Siddique R. COVID-19 infection: Origin, transmission, and characteristics of human coronaviruses. J Adv Res 2020 Mar;24:91-98.
- 12. Alfaraj SH, Al-Tawfiq JA, Altuwaijri TA, Memish ZA. Middle East respiratory syndrome coronavirus and pulmonary tuberculosis coinfection: implications for infection control. Intervirology 2017;60(1-2):53-55.
- 13. Liu W, Fontanet A, Zhang PH, Zhan L, Xin ZT, Tang F, et al. Pulmonary tuberculosis and SARS, China. Emerg Infect Dis 2006 Apr;12(4):707-709.
- 14. Wong CY, Wong KY, Law TS, Shum TT, Li YK, Pang WK. Tuberculosis in a SARS outbreak. J Chin Med Assoc 2004 Nov;67(11):579-582.
- 15. Khodamoradi Z, Moghadami M, Lotfi M. Co-infection of coronavirus disease 2019 and Influenza A: a report from Iran. Arch Iran Med 2020 Apr;23(4):239-243.
- 16. He G, Wu J, Shi J, Dai J, Gamber M, Jiang X, et al. COVID-19 in tuberculosis patients: A report of three cases. J Med Virol 2020 Oct;92(10):1802-1806.
- 17. Motta I, Centis R, D’Ambrosio L, García-García JM, Goletti D, Gualano G, et al. Tuberculosis, COVID-19 and migrants: Preliminary analysis of deaths occurring in 69 patients from two cohorts. Pulmonology 2020 Jul - Aug;26(4):233-240.
- 18. Davies M-A. HIV and risk of COVID-19 death: a population cohort study from the western cape province, South Africa. MedRxiv 2020;1-21.
- 19. Al Abri S, Kowada A, Yaqoubi F, Al Khalili S, Ndunda N, Petersen E. Cost-effectiveness of IGRA/QFT-Plus for TB screening of migrants in Oman. Int J Infect Dis 2020 Mar;92S:S72-S77 .
- 20. Low JG, Lee CC, Leo YS, Low JG, Lee CC, Leo YS. Severe acute respiratory syndrome and pulmonary tuberculosis. Clin Infect Dis 2004 Jun;38(12):e123-e125.
- 21. Chen Y, Wang Y, Fleming J, Yu Y, Gu Y, Liu C, et al. Active or latent tuberculosis increases susceptibility to COVID-19 and disease severity. MedRxiv preprint 2020. [cited October 2020]. Available from https://www.medrxiv.org/content/10.1101/2020.03.10.20033795v1.full.pdf.
- 22. Crisan-Dabija R, Grigorescu C, Pavel C-A, Artene B, Popa IV, Cernomaz A, et al. Tuberculosis and COVID-19 in 2020: lessons from the past viral outbreaks and possible future outcomes. Can Respir J 2020 Sep;2020:1401053.
- 23. Mousquer GT, Peres A, Fiegenbaum M. Pathology of TB/COVID-19 Co-Infection: The phantom menace. Tuberculosis (Edinb) 2021 Jan;126:102020 .