On 11 March 2020, the World Health Organization (WHO) declared the novel coronavirus disease 2019 (COVID-19) as a pandemic. As of 31 December 2020, a total of 68 602 295 confirmed cases and deaths of 1 564 712 were reported globally.1*
The COVID-19 pandemic continues to pose an unprecedented health threat to countries worldwide.1 At the end of March 2020, COVID-19 had spread across all six member states of the Gulf Cooperation Council (GCC) countries. The first five cases of COVID-19 in the GCC member states were reported in the UAE on 29 January 2020 from travelers arriving from Wuhan City, China. Bahrain, Qatar, Kuwait, and Oman reported their first cases in February and Saudi Arabia in March 2020.1
The epidemiological status of COVID-19 in the GCC member states is noted to be widely varying [Figure 1].1 As of 31 December 2020, the GCC member states had reported a total of 1 086 526 cases with 13 802 deaths.** The COVID-19 infection rates in GCC member states ranged between 996 to 4994 cases per million population, and case fatality rates were between 0.2 and 1.6 as of June 2020.1 In general, the GCC member states have reported lower COVID-19 related mortality given the advanced healthcare system and comprehensive governmental efforts.2
Prior experience of the region in dealing with the Middle East respiratory syndrome-related coronavirus (MERS) in 2012,3 and the experience of dealing with large numbers of pilgrims in Saudi Arabia4 and tourists in the UAE resulted in proactive preparedness efforts to COVID-19 before the first case was officially detected. Across several countries, several public health precautionary measures were implemented in a faster approach, including lockdowns of major cities, complete suspension of flights, university and school closures, banning of social gatherings and sports events, provision of free-of-charge healthcare to patients, and launching of COVID-19 active screening.5 To guide countries in scaling-up operational readiness and response to COVID-19, the WHO published the Strategic Preparedness and Response Plan in February 2020, which identified various activities to assist countries in preparing and responding to COVID-19.4 The immediate activities required for international preparedness and response to the evolving COVID-19 outbreak and set of eight priority areas (pillars) essential for scaling-up country operational readiness and response [Figure 2].6
The plan guided the development and adaptation of national plans. Despite a semi-annual progress report on implementing the Global Strategic Plan in June 2020, there is limited granular information available on the extent of the national plan’s content and implementation, particularly in the Member States of the GCC.
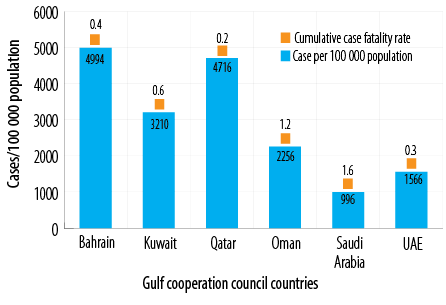
Figure 1: Epidemiology of COVID-19 in Gulf Cooperation Council member states as of the end of December 2020.

Figure 2: World Health Organization strategic response plan for COVID- 19 infection.
We aimed to rapidly review the preparedness and response activities to the COVID-19 outbreak in the GCC member states in the first phase of the pandemic to document lessons learned for improving the ongoing response efforts in preparing for the resurgence or anticipated second and third waves of the pandemic and preparedness for future pandemics.
Methods
A rapid appraisal approach7 was conducted in June 2020. A closed-ended questionnaire whereby primary data was collected through a survey administered to key informants and cross-triangulated with secondary data collected through a review of available published and grey literature by the six-member states.
Data was collected from Bahrain, Kuwait, Oman, Qatar, Saudi Arabia, and the UAE.
The survey was developed according to the WHO Strategic Preparedness and Response Plan and the accompanying Operational Planning Guidelines.8 As such, the following pillars were reviewed: (1) country-level coordination planning and monitoring; (2) risk communication and community engagement; (3) surveillance, rapid response, and case investigation; (4) border points of entry; (5) infection prevention and control strategies; (6) case management; and (7) operational support and logistics. The survey was also modified to include research and innovation to guide decision-making, and implementation of non-pharmaceutical public health interventions. A total of 11 pillars were identified and measured [Table 1]. The survey was administered in June 2020 by key informants (i.e., Ministry of Health professionals or individuals involved in the national committees steering the preparedness and response efforts).
Data was captured in Microsoft Excel, and each activity was scored across a scale of either 1 (present or task completed by the date of data collection) or zero (not done). The total score for each component or pillar was then calculated and converted into a percentage. The resulting data were then compared for each country. A benchmark of 95% was set as a success standard. The data were then compared across the countries.
The study reports on secondary data, and no human subjects were included in terms of the interview or using the patients’ health records; therefore, ethical approval was not required. Moreover, this study follows the Declaration of Helsinki.
Results
The preparedness and response efforts of Bahrain, Saudi Arabia, and UAE were fully compliant with 11 (100%) pillars of the modified strategic response measures. Kuwait, Oman, and Qatar were compliant with 10 of the 11 pillars [Table 1]. The component of conducting COVID-19 related research was the lowest-performing across all the six countries.
Table 1: A modified World Health Organization framework for strategic response plan evaluation and performance against measured criteria across six Gulf Cooperation Council member states.
|
Country-level coordination |
11 |
100 |
100 |
95.0 |
100 |
100 |
100 |
|
Risk communication and community engagement |
12 |
100 |
100 |
100 |
92.0 |
100 |
100 |
|
Surveillance, rapid response, and case investigation- decision-makers and community |
6 |
100 |
100 |
100 |
100 |
100 |
100 |
|
Border points of entry, international travel, and transport |
7 |
100 |
100 |
100 |
100 |
100 |
100 |
|
Infection prevention and control strategies |
14 |
100 |
100 |
100 |
100 |
100 |
100 |
|
Case management |
15 |
100 |
93.0 |
100 |
100 |
100 |
100 |
|
Operational support and logistics |
15 |
100 |
100 |
100 |
100 |
100 |
100 |
|
Conducting research during the COVID-19 pandemic |
9 |
80 |
80 |
80 |
80 |
100 |
80 |
1. Country-level coordination, planning, and monitoring
Strategic and systematic coordination, planning, and monitoring is critical to help mitigate the impact of any public health event, particularly a pandemic, as countries with a national multi-sectoral preparedness and response plan and coordination structure are empowered with the ability to timely respond across national and subnational levels and cautiously tailor the response strategy.
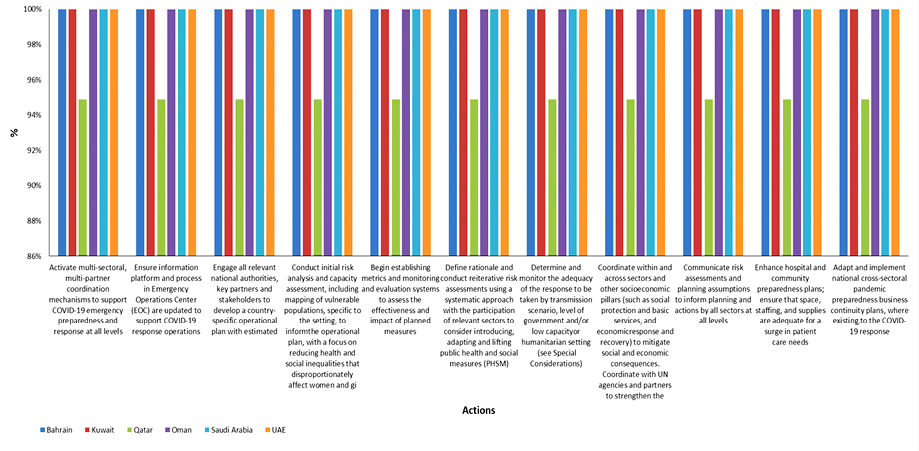
Figure 3: Country-level coordination, planning, and monitoring.
Five countries (Bahrain, Kuwait, Oman, Saudi Arabia, and UAE) achieved 100% in coordination, planning, and monitoring, while Qatar achieved 95.0% [Figure 3]. The elements of the COVID-19 national preparedness and response plan that were activated by all six member states included: designating the roles and responsibilities of different entities to expedite real-time response during events, coordinating communications, surveillance, information, resource allocation, educational activities, and measures to prevent and control further spread of COVID-19. Qatar did not achieve full compliance with the element of engaging all relevant national authorities, key partners, and stakeholders to develop a country-specific operational plan.
2. Risk communication and community engagement
In the absence of effective medical treatment or a vaccine, coordinated clear communication and engagement with citizens on risks and behavioral modification were key countermeasures to the COVID-19 pandemic. Proactive communication, providing clear and actionable information based on community concerns and perceptions, was essential for behavioral changes. All GCC countries had a timely assessment of the risks of COVID-19, and transparent communication messaging was implemented both at national and sub-national levels. A surge and sustainable support from governments to cover the communication needs during the COVID-19 outbreak were unanimously provided. Although at a strategic level, the Minister of Health and the Supreme Committee had regular communication with the community. Oman’s response did not include risk communication team/health professionals at the sub-national level.
3. Surveillance, rapid response, and case investigation
All GCC member states established a daily practice of monitoring COVID-19 cases, mortality, and contact tracing, as well as aggregating weekly and monthly data. The daily hospitalization rate in each institution was monitored. All six GCC member states achieved 100% compliance in terms of mandatory national COVID-19 notification system, reporting templates for public health staff at local/regional and/or national levels, case definitions, and procedures for testing and reporting, a protocol for enhanced surveillance and/or contact tracing to collect detailed information around the first cases and contacts, designating well-trained investigation team for respiratory disease outbreaks, including emerging, establishing guidelines and standard operation procedures, enhancing contact tracing capacity with support from all sectors, stakeholders and community, and creating tools and protocols to follow-up cases and contacts.
4. Points of entry, national-international travel, and transport
All GCC member states, following their preparedness and response plans, adopted and strengthened the following: appointed public health authority for surveillance and disease control purposes at points of entry; reviewed the existing public health emergency contingency plans and adopted them for COVID-19 response, created space for prompt and rapid health assessment, providing isolation and quarantine facilities with sufficient stockpile of personal protective equipment (PPE), and oriented and trained healthcare staff on aspects of proper surveillance, case detection based on case definitions, infection control and prevention measures, quality control and monitoring performance and compliance in all measures, protocols, and guidelines. Furthermore, reinforcement of travel and transportation included planned transportation and ambulance services to designated hospitals, applied passenger/traveler declaration mobile-based applications (i.e., Tarrasud+) for arriving and departing travelers, health education and awareness activities for all travelers, and regular simulation drills at point of entry to test the system response and readiness.
5. Infection prevention and control
All six countries achieved 100% compliance with the infection prevention and control requirements of the strategic response. This included national infection prevention and control programs, which were authorized to coordinate, collect, analyze, and report data on healthcare-associated infections. The program developed and disseminated infection prevention and control guidelines and protocols to all health institutions where suspected and confirmed COVID-19 cases were admitted. Updates based on emerging research and new information shared with the WHO was regularly provided to all health care institutions. Well-equipped isolation rooms/beds were made available in all hospitals with admission service. However, concerning infection prevention and control, monitoring5 both Oman and Kuwait were lacking measurement of cumulative incidence amongst patients, medical and allied staff, and community outreach services.
6. Clinical management and outcome of COVID-19
In the fight against COVID-19, the GCC member states took a multipronged approach for prevention and cure. All member states constituted task force groups and committees involved in developing national technical guidance/protocols for clinical care of COVID-19 patients based on ongoing assessment of new evidence generated by the international community and first responders and reviewed them frequently as the scientific evidence emerged. The guidance provided clinicians with interim advice on timely, effective, safe care, and support to the COVID-19 patients with primary, secondary, and tertiary levels of healthcare. These guidelines were established relatively early in the COVID-19 pandemic. They included case definitions, screening, triage, infection prevention, specimen collection, therapeutic drug options, critical care pathways, referral pathways, telemedicine, emergency medical services, reporting COVID-19 deaths, and monitoring and follow-ups. Additionally, all the activities from developing standard operating practices, procurement therapeutics, sharing clinical care experiences and challenges, training, and dissemination of the guidelines were done concurrently.
Front line clinicians from all member states were brought together under the umbrella of the Gulf Health Council to share expertise and experience and develop the GCC guideline6 for screening, diagnosing, and treating COVID-19 for patients suspected of or confirmed with the infection. The GCC clinical management guideline was approved and endorsed by top leaders in the ministries
of health.
7. Operational support and logistics
Designated focal points were assigned to COVID-19 response in logistics and supply. The assigned focal points linked with all the pillars of the response for supply forecasting and ensured procurement mechanisms are in place in the country for the rapid procurement of additional medical commodities whenever needed.
Each member state had sufficient storage capacity for all commodities, estimated logistics required. Besides, all member states were functioning stock management systems to fast-track the distribution of medical commodities under urgent conditions, as well as available and effective transport and distribution systems for speedy and equitable distribution of emergency commodities.
8. Managing essential health services and systems
Managing essential health services and systems was reported by all respondents. All six member states strengthened healthcare facilities, designated hospitals for treating COVID-19 patients, enforced infection control procedures and visual triage, and monitored the capacity for isolation beds, equipment, human resources, and critical medical supplies. Technical guidelines and operational protocols were prepared and disseminated promptly. National committees, task forces, and Ministries of Health were responsible for activating an emergency command system to coordinate the actions of the relevant responders. Sharing real-time information about the outbreak to the policy and decision-makers, manage resources for lab and infection control requirements (acquisitions, tracking, and monitoring), and monitoring COVID-19 cases in hospitals or communities (household isolation), were implemented in all six countries.
The public healthcare teams were responsible for initiating the epidemiological investigation. These teams investigated the cases, completed the epidemiological investigation in healthcare and community settings using the COVID-19 epidemiological investigation national frameworks, and followed up the cases. Contact tracing and identification were another important part of the system.
9. Application of non-pharmaceutical public health interventions
Upon notification of the first COVID-19 case, the GCC member states have implemented unprecedented non-pharmaceutical public health interventions to control further spread and allow time for restructuring healthcare capacities. All states implemented most of these interventions. These interventions included universal face mask wearing, physical distancing between the general communities, isolation of patients with COVID-19, quarantine of exposed contacts to positive COVID-19 and returned travelers from highly epidemic countries. This was followed by the closure of parks, schools, malls, mosques, and restrictions in social gatherings such as postponement of large public events and mass gatherings like weddings and the restriction of religious mass gatherings, including pilgrimage. Additional interventions commenced, including airport screening, refraining tourist visas, and entry restrictions on either specific nationalities or those with specific recent travel history. Screening of all arrivals, early cases detection, isolation of ill persons, contact tracing, and quarantine of exposed persons were universally implemented. All non-essential commerce businesses were closed. Air, land, and sea borders were closed with travel restrictions deployment between the different regions within the country.
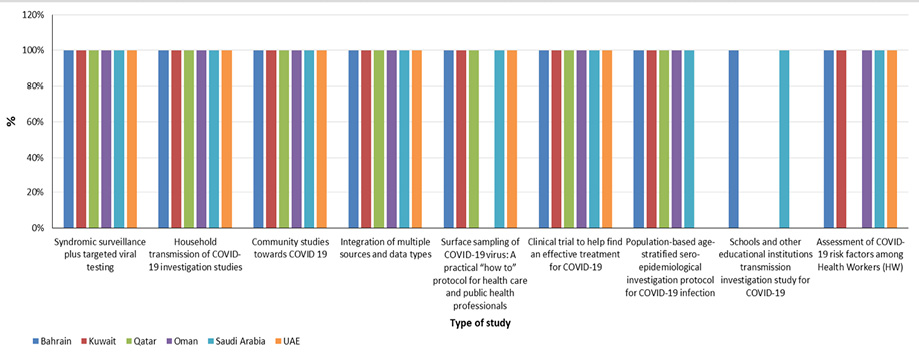
Figure 4: Conducting research during the COVID 19 pandemic.
10. Conducting research and innovation to guide decision-making
While general COVID-19-related research was conducted in the first phase (June 2020), all six GCC member states performed medium based on the WHO research criteria.2 The exception was Saudi Arabia and Bahrain, which achieved 100%, performing community and population-based age-stratified sero-prevalence epidemiological studies, and research into the transmission of COVID-19 within households, schools, and workplaces and clinical trials for effective therapies. Kuwait achieved 88.9% compliance (8/9 elements); while, Qatar, Oman, and the UAE scored 66.7% (6/9 elements). Five out of six countries conducted investigations in schools and other educational institutions on the transmission of COVID-19 [Figure 4].
11. Care for migrants and expatriate workers
Screening, diagnosis, and treatment of COVID-19 among foreign-born (non-citizen) workers, including hospitalization, were nominally free of charge in all six countries, regardless of their administrative position to live in GCC member states. Adequate social protection strategies for foreign-born COVID-19 patients are also being sought.
Discussion
The COVID-19 pandemic is a complex global health crisis that has brought social-economical complications and challenges. The pandemic had a major impact on the livelihoods of citizens and the stability of the economies of the GCC member states. Countries have responded with unprecedented levels of both fiscal and monetary stimuli to counter the impact of this crisis.9
Building on past experiences of responding to the MERS-CoV, the GCC member states initiated a rapid response, an evidence-based approach that was well communicated, and a spirit of partnership and collaboration.10 The GCC member states implemented all pillars of preparedness and response plan established by the WHO as a strategy for combating COVID-19 infection.6 Central to the implementation of the strategic response was strong and decisive leadership displayed across the member states.
Core to an effective response is the coordination of interventions through multi-sectoral engagement, clear roles and responsibilities, decision making, and communication. As demonstrated by the survey, the GCC member states established country teams, conducted a risk assessment, and developed a coordinated multi-sectoral response that was well communicated. As a result of this coordination and the presence of decisive leadership, a range of effective measures was implemented to limit the virus spread, which included but was not limited to travel and movement restrictions (including domestic and international flight restrictions), closure of borders, schools and non-essential businesses, suspension of mass gatherings, partial-to-full lockdowns, and intensive community engagement. The prompt implementation of such measures undoubtedly reduced virus transmission in the region. However, these measures also resulted in significant economic and societal costs. Ultimately, these costs, together with socioeconomic pressure and community fatigue, influenced the public health decisions related to COVID-19 infection, particularly about the relaxation of social measures.
Managing essential health services requires the presence of a resilient health care system and innovation. The six countries in the region continued to provide services while maintaining the highest standards of care for all patients in need of health services. Driven by the coronavirus, the organizations in the region integrated technology to provide these services and monitor and control COVID-19 transmission. This includes telemedicine, fast tracks for medications, apps for tracing confirmed and suspected cases, and apps for daily reporting of health care workers symptoms. Nevertheless, as many patients were affected due to reorganizing care delivery and cutting non-essential services, the capacity for re-delivering ‘regular’ care should be used wisely and each GCC country could establish national task force teams of medical specialists and other care professionals to avoid and prioritize the backlog by proper and timely planning. Besides, it is important to redesign patient pathways to ensure safety for patients and healthcare providers. Further, there is a large group of people with limited digital skills that should not be overlooked. They may be willing and capable of receiving remote support but lack the much-needed digital skills.
The COVID-19 response presents the GCC member states with many opportunities, including creating a common stockpile of PPE and medications under the GCC country office, coordinated joint public procurements, and regulated exports of key medical equipment to ensure a constant supply within the region, coordinating with relevant stakeholders to support priority research activities to close the knowledge gaps, sharing experiences timely, providing support and technical guidance to countries to set-up and activate emergency operation centers at national and subnational levels to better coordinate the response, establishing a regional strong technical support to countries through the country technical support team to provide timely feedback on emerging questions, focusing on coordination and alignment within the public sector and the private sector, and using technology in education and expansion of cash transfers to vulnerable individuals. The GCC member states could invest in shifting care to home and provide as much care as possible remotely. Even when the pandemic is over, telemedicine could be the ‘norm’ as an alternative for outpatient visits and primary care consults. This includes launching apps for preventive services in primary care, mental health care, and delivering care to patients with chronic diseases such as diabetes, hypertension, chronic congestive heart failure, HIV, and the treatment of vulnerable patients that require dialysis or chemotherapy.
As the number of new cases declines and the availability of the vaccine is on the horizon, the approach may require the use of existing resources, structures, and processes creatively and enable their recombination to extend the range of alternative solutions.10
Furthermore, ongoing revising of the national plans to include vaccine introduction and appropriate distribution and the considerations of how the vaccine introduction will affect other response measures (e.g., mask wearing, school opening etc.) is paramount.
Study limitations include findings biased to the information that was available to the researchers at the time. Further information is needed and we recommend countries to conduct comprehensive intra-action reviews and publish them.
ConclusioN
This study provides an overview of the evolution and current status of response activities to mitigate the COVID-19 pandemic in GCC member states. The ongoing pandemic may prove an opportunity to accelerate some reforms that would have otherwise taken longer. Without plans in place for handling future, unexpected public health crises, governments imperil the social and health outcomes of populations and could further exacerbate existing socioeconomic divides. On the other hand, by putting in place the proper organizational structures and procedures to tackle public health crises, the government can promote improved health outcomes, minimize unnecessary spending, quell market uncertainty, and win citizen trust and future compliance in measures enacted by the government to protect the public interest as they pertain to public health.
*As of 22 August 2021, a total of 213 050 725 confirmed cases and deaths of 4 448 352 were reported across the globe.
**As of 22 August 2021, the GCC member states had reported a total of 2 468 377 coronavirus cases with 18 957 deaths.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
Acknowledgements
The authors would like to thank all the workshop participants who were instrumental in the development of the manuscript, namely Magda Al Wahebi.
references
- 1. World Health Organization (WHO). COVID-19 dashboard. 2020 [cited 2020 December 27]. Available from: https://who.sprinklr.com.
- 2. Le NK, Le AV, Brooks JP, Khetpal S, Liauw D, Izurieta R, et al. Impact of government-imposed social distancing measures on COVID-19 morbidity and mortality around the world. Bull World Health Organ 2020;10.
- 3. Al Awaidy ST, Al Maqbali AA, Omer I, Al Mukhaini S, Al Risi MA, Al Maqbali MS, et al. The first clusters of Middle East respiratory syndrome coronavirus in Oman: Time to act. J Infect Public Health 2020 May;13(5):679-686.
- 4. Ridda I, Mansoor S, Briggs R, Gishe J, Aatmn D. Preparedness for mass gathering during Hajj and Umrah handbook of healthcare in Arab World. Springer Nature Switzerland AG; 2019. p. 1-21.
- 5. Durugbo CM, Al-Jayyousi OR, Almahamid SM. Wisdom from Arabian creatives: systematic review of innovation management literature for the Gulf Cooperation Council (GCC) Region. International Journal of Innovation and Technology Management 2020;17(6):2030004 .
- 6. World Health Organization. COVID-19 strategic preparedness and response progress report - 1. 2020 [cited 2020 December 5]. Available from: https://www.who.int/publications/m/item/who-covid-19-preparedness-and-response-progress-report---1-february-to-30-june-2020.
- 7. Koch T, Iliffe S; EVIDEM-ED project. Rapid appraisal of barriers to the diagnosis and management of patients with dementia in primary care: a systematic review. BMC Fam Pract 2010 Jul;11(1):52.
- 8. World Health Organization. Coronavirus disease (COVID-19) technical guidance: the unity studies: early investigation protocols. 2020 [cited 2020 December 5]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/early-investigations.
- 9. Al Saidi AM, Nur FA, Al-Mandhari AS, El Rabbat M, Hafeez A, Abubakar A. Decisive leadership is a necessity in the COVID-19 response. Lancet 2020 Aug;396(10247):295-298.
- 10. Lloyd-Smith M. The COVID-19 pandemic: resilient organisational response to a low-chance, high-impact event. BMJ Leader 2020;4(3):109.