Deep vein thrombosis (DVT) with a reported incidence of 45–117 cases per 100 000 person/years1 is quite common. Some patients have a hereditary thrombophilic tendency. In those with first-time DVT, factor V Leiden and prothrombin G20210A mutations with an incidence of 20–25% and 6–18%, respectively, are the most common.2 Many environmental factors and acquired medical conditions also play a role (e.g., immobility, recent surgery, air travel longer than four hours, cancer, or inflammatory bowel disease). On the other hand, some patients have unprovoked DVT. In some of these seemingly idiopathic cases, interesting remediable anatomical causes can be discovered if pursued further. Here, we present a case report of May-Thurner Syndrome (MTS) to raise awareness.
Case report
A 45-years-old woman was admitted with an unprovoked DVT of the left leg. She presented with one day history of spontaneous pain and swelling of the left leg. The pain was mild to moderate intensity, radiating from the groin to involve the whole left leg. She had no previous history of DVT. She was married for five years but had no children. A right ovarian cyst was discovered during workup for primary infertility. She was scheduled to undergo cystectomy and received a two-week course of norethisterone 5 mg twice daily. She received a shot of intra-articular steroid in her left knee for osteoarthritis three months ago, but was well and active and was not taking any regular medications. There was no family history of DVT.

Figure 1: A CT scan showing thrombus in left common iliac vein (CIV).
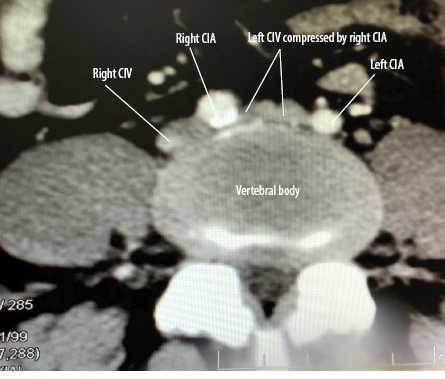
Figure 2: A CT scan axial view showing compression of left common iliac vein (CIV) by the right common iliac artery (CIA) against the vertebral body.
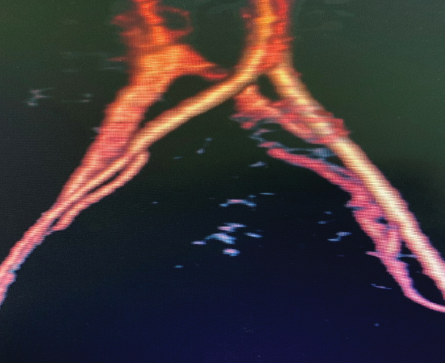
Figure 3: The MRI angiogram depicting thrombosis and compression of left common iliac vein by the right common iliac artery (May-Thurner syndrome).
She was an average-built woman with normal vitals. Her left leg was grossly swollen but not erythematous, hot or tender, with intact distal pulses. The circumference of the calf, 15 cm below the tibial tuberosity, was 42 cm on the left compared to 34 cm on the right. The rest of the physical examination was unremarkable, apart from mild tenderness and a vague feeling of a small soft mass in the right lower abdomen.
Her routine investigations and chest X-ray were normal. The venous Doppler revealed extensive DVT of left common and superficial femoral veins (a misnomer, actually a deep vein). Abdomino-pelvic ultrasound showed a 4.5 × 4.0 cm right ovarian cyst. An abdominal contrast-enhanced computed tomography (CT) scan confirmed a long thrombus involving left femoral and external iliac veins (EIV) extending up to the distal part of the left common iliac vein (CIV), raising suspicion of MTS [Figures 1 and 2]. The right adnexal cyst appeared benign.
Magnetic resonance imaging (MRI) showed compression of the left CIV by the right common iliac artery (CIA) with a subacute venous thrombus distal to the compression [Figure 3].
She was started on a therapeutic dose of enoxaparin and referred to vascular surgery. However, she was managed conservatively as she was doing well. Six months later, a follow-up Doppler showed partial recanalization of common femoral and near-complete recanalization of left EIV and CIV. Later, laparoscopic removal of the right ovarian cyst confirmed a simple serous cyst.
Discussion
MTS, also known as Cockett’s or iliac vein compression syndrome, occurs as result of compression of left CIV by the right CIA against the fifth lumbar vertebrae. Other variants of compression of iliocaval veins by the arterial system also exist.3 The fact that DVT of pelvic veins is five times more common on the left, primarily due to compression by the overlying artery, was known since Virchow’s4 time a century ago. However, May and Thurner were the first to observe that a collagen and elastin spur is formed on the inner wall of the vein due to repeated trauma of chronic pulsation of the overlying right CIA. The spur causes partial obstruction and predisposes to thrombosis.5
Thrombosis in the iliofemoral veins is responsible for approximately 2–23% of cases of DVT in lower limbs.6 About 50–60% of such cases of DVT on the left side are associated with spurs in CIV due to external compression.7
Although MTS is the cause in only 1–5% of patients with lower extremity venous symptoms of swelling or DVT,8 the frequency of MTS anatomy in the asymptomatic population is much higher. A compression of left CIV of > 50% was noticed in 24% of cases in a study in which CT scan of abdomen was done for reasons other than leg symptoms.9
MTS classically presents in young females in their second or third decade10 typically with swelling of the left leg of a few weeks duration, though right-sided and bilateral cases do occur.3,11 About one-third of patients are males.12 DVT is an acute presentation with surgery, pregnancy, and prolonged bed rest described as acute triggers. DVT can occur even during prophylactic anticoagulation.13 Chronic presentations include post-thrombotic syndrome, lower limb swelling, venous claudication, and pelvic congestion in females.14
Though technically challenging, duplex ultrasound of IV is usually performed first, followed by spiral CT or MRI venography, both of which have > 95% sensitivity and specificity for diagnosing MTS15,16 and can, in addition, reveal a pelvic mass. Nevertheless, dehydration and inadequate perfusion of the pelvic veins may affect the diagnostic ability of these imaging modalities.
Conventional venography has long been a gold standard for the diagnosis of MTS,13 but is rarely used now. The use of intravascular ultrasound appears to be superior17 and may obviate the need for venography.
Treatment of MTS depends on the presence or absence of DVT. MTS with minimal or no symptoms may be managed conservatively with compression stockings. However, in those with more severe symptoms of chronic venous insufficiency, relief of stenosis by a stent helps.18 In cases of MTS with iliofemoral DVT, anticoagulation alone leads to complete recanalization in only 20–30% of cases,19 and the incidence of post-thrombotic syndrome or recurrent DVT remains high. However, early catheter-directed thrombolysis or pharmaco-mechanical thrombectomy followed by angioplasty and stent in the stenosed vein is associated with greatly improved results. In a review of 1500 patients with iliac vein stenosis, with or without thrombosis, the stent placement was safe, relieved pain in 90%, and helped swelling and venous ulcers in two-thirds or more.20 Rarely, open surgery may be required if endovascular therapy fails. Our patient was managed conservatively, and she was doing well on follow-up.
Conclusion
DVT is usually managed with a course of anticoagulation, but it is worthwhile to properly investigate some cases where remediable conditions with more definitive treatments and better prognosis may be found. For example, DVT of the IV may be due to arterial compression necessitating a stent.
Disclosure
The authors declared no conflicts of interest.
references
- 1. Heit JA. Epidemiology of venous thromboembolism. Nat Rev Cardiol 2015 Aug;12(8):464-474.
- 2. Cannon KA, Badiee J, Brill JB, Olson EJ, Sise MJ, Bansal V, et al. Hereditary thrombophilia in trauma patients with venous thromboembolism: Is routine screening necessary? J Trauma Acute Care Surg 2018 Feb;84(2):330-333.
- 3. Abboud G, Midulla M, Lions C, El Ngheoui Z, Gengler L, Martinelli T, et al. “Right-sided” May-Thurner syndrome. Cardiovasc Intervent Radiol 2010 Oct;33(5):1056-1059.
- 4. Virchow R. Ueber die Erweiterung kleinerer Gefafse. Arch Pathol Anat Physiol Klin Med 1851;3(3):427-462.
- 5. May R, Thurner J. The cause of the predominantly sinistral occurrence of thrombosis of the pelvic veins. Angiology 1957 Oct;8(5):419-427.
- 6. Markel A, Manzo RA, Bergelin RO, Strandness DE Jr. Pattern and distribution of thrombi in acute venous thrombosis. Arch Surg 1992 Mar;127(3):305-309.
- 7. Mickley V, Schwagierek R, Rilinger N, Görich J, Sunder-Plassmann L. Left iliac venous thrombosis caused by venous spur: treatment with thrombectomy and stent implantation. J Vasc Surg 1998 Sep;28(3):492-497.
- 8. Taheri SA, Williams J, Powell S, Cullen J, Peer R, Nowakowski P, et al. Iliocaval compression syndrome. Am J Surg 1987 Aug;154(2):169-172.
- 9. Kibbe MR, Ujiki M, Goodwin AL, Eskandari M, Yao J, Matsumura J. Iliac vein compression in an asymptomatic patient population. J Vasc Surg 2004 May;39(5):937-943.
- 10. Cockett FB, Thomas ML. The iliac compression syndrome. Br J Surg 1965 Oct;52(10):816-821.
- 11. Png CY, Nakazawa KR, Lau IH, Tadros RO, Faries PL, Ting W. Bilateral May-Thurner syndrome refractory to iliac aneurysm repair. J Vasc Surg Venous Lymphat Disord 2018 Sep;6(5):657-660.
- 12. Kaltenmeier CT, Erben Y, Indes J, Lee A, Dardik A, Sarac T, et al. Systematic review of May-Thurner syndrome with emphasis on gender differences. J Vasc Surg Venous Lymphat Disord 2018 May;6(3):399-407.
- 13. Foit NA, Chen QM, Cook B, Hammerberg EM. Iliofemoral deep vein thrombosis after tibial plateau fracture fixation related to undiagnosed May-Thurner syndrome: a case report. Patient Saf Surg 2013 Apr;7(1):12.
- 14. Khan TA, Rudolph KP, Huber TS, Fatima J. May-Thurner syndrome presenting as pelvic congestion syndrome and vulvar varicosities in a nonpregnant adolescent. J Vasc Surg Cases Innov Tech 2019 Jun;5(3):252-254.
- 15. Liu Z, Gao N, Shen L, Yang J, Zhu Y, Li Z, et al. Endovascular treatment for symptomatic iliac vein compression syndrome: a prospective consecutive series of 48 patients. Ann Vasc Surg 2014 Apr;28(3):695-704.
- 16. Wolpert LM, Rahmani O, Stein B, Gallagher JJ, Drezner AD. Magnetic resonance venography in the diagnosis and management of May-Thurner syndrome. Vasc Endovascular Surg 2002 Jan-Feb;36(1):51-57.
- 17. Neglén P, Raju S. Intravascular ultrasound scan evaluation of the obstructed vein. J Vasc Surg 2002 Apr;35(4):694-700.
- 18. Raju S, Owen S Jr, Neglen P. The clinical impact of iliac venous stents in the management of chronic venous insufficiency. J Vasc Surg 2002 Jan;35(1):8-15.
- 19. Neglén P, Raju S. Proximal lower extremity chronic venous outflow obstruction: recognition and treatment. Semin Vasc Surg 2002 Mar;15(1):57-64.
- 20. Raju S. Best management options for chronic iliac vein stenosis and occlusion. J Vasc Surg 2013 Apr;57(4):1163-1169.