More patients with pleural effusions or pneumothorax are being treated with small-bore chest tubes rather than with large-bore tubes in recent years.1–3 The small-bore catheters are easier to insert, have fewer complications, and cause less pain while they are in place. The placement of the small-bore catheters is probably more optimal when done with ultrasound (US) guidance. However, though less traumatic, there are certain possible complications like pneumothorax, hemorrhage, occlusion, tube migration, and infection.1,3 In a study of 51 patients, pigtail catheter drainage of pleural effusion was successful in 82.35%, and the success rate was highest with transudative pleural effusions.4 Liu et al,5 reported a success rate of 64.0–81.6% in patients with different etiologies of pleural effusion. This study aimed to evaluate the efficacy and complications of US-guided pigtail catheter drainage of pleural effusions.
Methods
We conducted a retrospective study of patients who underwent US-guided pigtail catheter insertion between January 2009 and December 2015 at Sultan Qaboos University Hospital, Muscat, a tertiary care center in Oman. All adult patients with pleural effusion who underwent US-guided pigtail drainage during this period were included. The medical record number of these patients was collected from the records of the radiology department. After approval by the local ethical and research committee, subjects data was gathered from the hospital’s electronic patient record system. The patient’s demographic information, diagnosis, the reason for requesting US-guided pleural drainage, and the imaging findings were collected from the patient records. Further data on the biochemical, microbiological, and cytological characteristics of the pleural fluid were also obtained. The duration of drainage and the outcome were also recorded. From the radiology records, the site of insertion and the catheter size were extracted.
All procedures were done in the radiology suite using 5–10 mL lidocaine 2% for local anesthesia. Pigtail catheters (Cook Medical Inc., Bloomington, IN, USA) size 8.5–14 French (Fr) were routinely used. The catheter insertion site was determined according to the US findings. Usually, after determining the insertion site, the catheters were inserted using the modified Seldinger technique. The pigtail catheters were then attached to a drainage bag or a pleural drainage system as appropriate. Success of pigtail catheter drainage for our study was defined as a clinical improvement by image findings and/or symptoms without requiring a second intervention (repeat pigtail placement, tube thoracostomy, or surgical intervention) within 72 hours after removal of the catheter. A significant reduction in the effusion size as decided by the treating physician or a total clearance of the effusion was considered radiological improvement. Pleural effusion was classified as a transudate or exudate based on the well-known Light’s criteria.
We used SPSS (IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp.) for both data collection and analysis. Independent t-test and chi-square test were used to test for statistical significance. A p-value of < 0.005 was considered statistically significant.
Table 1: Baseline characteristics and the duration of drainage in exudative and transudative effusions.
|
Gender |
|
|
1.000 |
|
Male |
57 (52.3) |
17 (53.1) |
|
Female |
52 (47.7) |
15 (46.9) |
|
Site |
|
|
< 0.001* |
|
Right |
58 (53.2) |
18 (56.3) |
|
Left |
46 (42.2) |
4 (12.5) |
|
Bilateral |
5 (4.6) |
10 (31.3) |
|
Duration of drainage, days |
|
|
0.074 |
|
≤ 3 |
26 (23.9) |
13 (40.6) |
|
> 3 |
83 (76.1) |
19 (59.4) |
|
Hypertension |
40 (36.7) |
25 (78.1) |
< 0.001* |
|
Diabetes |
28 (25.7) |
18 (56.3) |
0.002* |
|
Smoking |
7 (6.4) |
2 (6.3) |
1.000 |
*Statistically significant.
Test: independent samples t-test and Fisher’s exact test/likelihood ratio test.
Results
One hundred and forty-one patients underwent a pigtail catheter insertion under US guidance during the study period. There were 74 (52.5%) males and 67 (47.5%) females. The majority of patients (n = 109, 77.3%) had an exudative and the rest (n = 32, 22.7%) had transudative effusions. The effusion was on the right in 76 (53.9%) patients, on the left in 50 (35.5%), and bilateral in 15 (10.6%). The baseline characteristics and the duration of drainage in exudative and transudative effusions are given in Table 1. Hypertension (p < 0.001), diabetes mellitus (p = 0.002), and ischemic heart disease (p = 0.003) were greater in those with transudative effusion [Table 1]. Interestingly, smoking rates were low in both groups at 6.4% and 6.3% for exudative and transudative effusion cases, respectively.
In both groups, the majority of the effusions requiring drainage were on the right side (p < 0.001). The median duration of drainage was 5.0 days for the whole study group. There was no significant difference (p = 0.232) in the median drainage duration between exudates (6.0 days) and transudates (4.5 days). Though not statistically significant (p = 0.074), 76.1% of the exudative effusions required drainage for three or more days. On the other hand, 40.6% of transudative effusion drained for less than three days compared with 23.9% in the exudative group.
The mean age of the patients with exudative effusion was 50.0±18.6 years and 67.3±15.5 years in patients with transudative effusion (p < 0.001). The number of males in both groups was greater, (n = 57, 52.3% and n = 17, 53.1%, respectively). The main cause of exudate was metastasis followed by pleural infection, while cardiac and renal failures were the main causes for transudate [Table 2]. Among the pleural infections, four (11.1%) cases were frank empyema. The most frequent metastasis was from the breast, which accounted for 20.0% (n = 8) of the cases of metastatic pleural effusions. A few of the etiologies were clubbed together as non-specific in 18.3% of exudates and 6.3% of transudates at the initial evaluation. The causes of effusion grouped as non-specific exudates included those seen in patients with trauma, pulmonary embolism, drug reaction, hemangioma, and muscular dystrophy. In trauma, only minimally or no blood-stained effusions were included and not frank hemothorax. Of the two patients with non-specific transudate, one had chylothorax and the other had asthma with type 2 respiratory failure.
The overall success rate of pleural effusion drainage using US-guided pigtail insertion was 90.1%. Among the 109 cases of exudative pleural effusion, 89.0% were successful compared to 93.8% success among patients with transudative effusion (n = 32) (p = 0.737). The success rates in different conditions are given in Table 2.
Table 2: The causes of effusions and the success rates of pigtail catheter drainage.
|
Exudate |
109 |
77.3 |
89.0 |
|
Lung cancer |
5 |
4.6 |
100 |
|
Metastasis |
40 |
36.7 |
90.0 |
|
Pleural infection |
36 |
33.0 |
83.3 |
|
Inflammatory |
8 |
7.3 |
87.5 |
|
Non-specific exudate |
20 |
18.3 |
95.0 |
|
Transudate |
32 |
22.7 |
93.8 |
|
Cardiac failure |
19 |
59.4 |
94.7 |
|
Renal disease |
7 |
21.9 |
85.7 |
|
Liver disease |
4 |
12.5 |
100 |
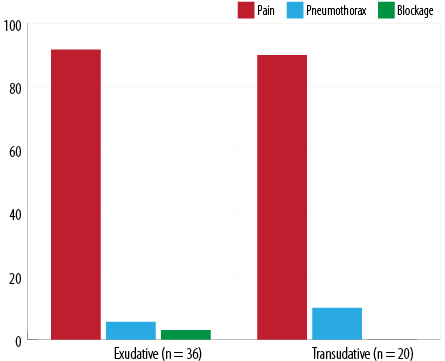
Figure 1: The complications of ultrasound-guided pigtail catheter drainage in exudative and transudative effusions.
Out of the 141 cases who underwent pigtail catheter insertion, 60.3% (n = 85) reported no complications. The incidence of pain requiring regular analgesics, pneumothorax, and blockage were seen in 36.2% (n = 51), 2.8% (n = 4), and 0.7% (n = 1), respectively. In the 56 patients with complications, generally no statistical significant difference was found in the incidence between the two groups (p = 0.541). Among those with complications, pain was the most frequently reported, 91.1% (n = 51) with 91.7% (n = 33) of patients in exudative group and 90.0% (n = 18) in transudative effusions [Figure 1]. Iatrogenic pneumothorax occurred in 5.6% (n = 2) of the exudative cases and 10.0% (n = 2) of the transudative cases. There was only a single case of pigtail blockage requiring removal.
Discussion
The growing interest in the use of small-bore catheters for pleural effusion drainage is rationalized based on the fact that it is less invasive, better tolerated, has fewer complications, and has a comparable efficiency with standard large-bore drains. In this report on 141 cases who underwent US-guided pigtail catheter insertion, we found that the procedure’s overall success rate was excellent with very few complications. Understandably, pain at the insertion site was the most frequent but was seen in < 37%. We also noted that most of the patients needed drainage for less than seven days.
Chest tubes, large bore (≥ 20 Fr), and small bore (< 20 Fr) are usually inserted for pneumothorax, hemothorax, parapneumonic effusions, empyema, malignant pleural effusion, chylothorax, chronic recurrent pleural effusions, and management of the postoperative chest space.1,6 The measurement unit French (Fr) was introduced by the French surgical instrument maker Joseph-Frédéric-Benoît Charrière in the 1800s.6 Typically, the small-bore tubes range from 6–19 Fr; 6-Fr tubes being used for pediatric patients. The most common tubes are pigtail catheters, which curl after the removal of a rigid insert. The coiled end of the tube thus prevents dislodgement of the drain.6 In recent years, with the use of the Seldinger technique for chest tube insertion, smaller tubes of 14 Fr or less have become more popular.2,7 This appears logical as the average adult intercostal space measured at the fifth intercostal space in the mid-axillary line measures 8.8±1.4 mm, and the outer diameter of the 8.3 Fr pigtail catheter is only 2.8 mm while it is 8 mm and 10.7 mm for the 24 Fr and 32 Fr chest tubes, respectively.8 Nevertheless, large-bore chest tubes are preferred for hemothorax and empyema. Unfortunately, there are no randomized studies comparing the clinical efficacy, complications, cost, and patient satisfaction with large-bore and small-bore tubes.6
The duration of drainage in our study group ranged from one to 25 days (median 5.0 days) for the whole study group. In other studies, the duration of drainage of pleural fluid using pigtail catheter were similar to our results.4,5,9,10 A report from Egypt recorded a duration between three and 14 days with a mean of 5.8±2.4 days.4 Similarly, Parulekar et al,11 reported a mean period of drainage of six days (three to 21 days) and Jain et al,9 seven days. Another study reported shorter drainage of 97 hours.8 The exudates needed a longer time for drainage in our group, with 76.1% draining for more than three days (median 6.0 days).
Liu et al,5 reported success rates from 64.0% to 81.6% in various pleural diseases. The success rate of pigtail catheter in empyema has been reported between 42% and 80%.4,5,12 The low success rate of 42% was on critically ill patients in the intensive care unit.12 Nevertheless, from a view of easiness, safety, less trauma, and better cosmetic result, pigtail catheter could be used initially in treating pleural empyema if there is no US evidence of loculations.1,13 We report a success rate of 83.3% in pleural infections. In tuberculosis, another frequently reported pleural infection, early drainage of effusions by pigtail catheter improves the dyspnea but fails to decrease the incidence of residual pleural thickening.14 We did not have any patients with tuberculosis pleural effusion needing pigtail drainage.
A retrospective review of 1092 pleural lesions with 324 drains for malignant effusions reported a success rate of 93.8% for small-bore wire-guided chest drains.15 Bediwy and Amer reported an 81.81% success in their cases of malignancy.4 The procedure was well-tolerated by patients and offered an effective treatment for malignant pleural effusions with success rates of 83%.13 We report a higher success rate of 90.0% to 100% in metastatic and primary lung malignancies, respectively. Pleurodesis is the only definitive treatment for recurrent symptomatic pleural effusions in malignant diseases. However, these days indwelling pleural catheters have become more popular as they not only lead to immediate symptom relief but also potentially create pleurodesis even without sclerosing agents.16
Recurrent and sometimes persistent transudative pleural effusions occur in chronic systemic illness due to a progressive deterioration of the underlying disease. Therapeutic approaches usually focus on intensifying the management strategies of the underlying condition. However, sometimes, effusions make the treatment refractory and will need drainage or introduction of new interventional procedures, making the management more complex.17,18 A high success rate of 85.71% was noted in transudative pleural effusions.4 Drains were found to be more successful when used for treating massive transudative pleural effusions.5 Nonetheless, drainage of massive transudative pleural effusions is of serious concern because it may lead to a prolonged drainage period and infection.12 Treatment of hepatic hydrothorax is a clinical challenge. Pigtail catheter is an effective and safe way for pleural drainage in patients with recurrent hepatic hydrothorax and provides a good treatment option.19 We noted improvement in all four patients with liver disease related transudative effusion. Heart failure is the most common cause of transudative pleural effusion and the second most common cause of pleural effusion.20 We noted high success rates of 93.8% in general for all transudates and 94.7% in patients with heart failure in particular.
Nearly 40% of our patients reported complications, but all were minor. Pain at the drainage site needing analgesics was the commonest. Pain has been reported previously in 45% of patients.4 Nevertheless, using a visual analog scale, the
small-bore catheter was found to cause significantly less pain than the large-bore chest tubes.21 The difference in pain intensity may be related to the tube’s size, the technique of insertion, use of analgesia, or the underlying cause.3 Pneumothorax was seen in only 2.8% of our study population. The incidence of pneumothorax varies from 3.3% to 20% in various studies. Lower incidence was noted by Sabry et al,21 (3.3%), Horsley et al,13 (3.8%), and Davies et al,22 (5.8%). Higher percentages of 19% to 31% were noted in other studies.23,24 Small pneumothoraxes occurring in 20% of patients in another study were thought to be due to air introduction during the procedure.9 Small catheters have a chance of blockage, and it was reported in 3.9% to 15% of the patients.4,9,13 Drains are particularly prone to blockage in empyemas.25 Though 15% of drains in a study failed due to blocking, the failure rate fell to 9.5% when the empyemas were not included.13 Tube getting blocked and needing removal was seen in only one of our patients. Interestingly, in another study, no complications of placement were seen, despite the fact that 24% of patients had laboratory evidence of coagulopathy and 47% were on mechanical ventilation.8 Rarely serious complications like left ventricular penetration, subclavian artery laceration, cerebral air embolism, and lung laceration have been reported.26,27 Besides, even in critically ill patients with pleural effusions the US-guided pigtail catheter insertion by the intensivists is well-tolerated and effective.12
Our study has a few limitations. The retrospective nature meant we could not gather the information on the total amount of fluid drained. Additionally, the etiology and the success were measured at the index admission. We measured only the early success rate; the patient may have had further interventions in subsequent admissions. Moreover, the data do not reflect the etiology of pleural effusions in our hospital as many would have had aspirations alone, single or multiple, or some would have had large-bore tubes placed in the wards. Since data collection, thoracic US has become more popular, and the number of interventions has increased.
Conclusion
US-guided pigtail catheter insertion is an effective and safe method of draining pleural fluid. It should be considered as the first intervention if drainage of a pleural effusion is indicated. It can be done easily and safely outside the radiology suite and even at the bedside. With the gaining popularity of point-of-care US, pigtail catheter insertions have already gained wider acceptance.
Acknowledgements
We would like to thank Dr. Usama Al-Amri, Medical officer, Department of Medicine and Mr. Al-Khatab Al-Saqri, Medical student, College of Medicine and Health Sciences, Sultan Qaboos University, for their help with a part of the data collection.
references
- 1. Havelock T, Teoh R, Laws D, Gleeson F; BTS Pleural Disease Guideline Group. Pleural procedures and thoracic ultrasound: British thoracic society pleural disease guideline 2010. Thorax 2010 Aug;65(Suppl 2):ii61-ii76.
- 2. Light RW. Pleural controversy: optimal chest tube size for drainage. Respirology 2011 Feb;16(2):244-248.
- 3. Rahman NM, Maskell NA, Davies CW, Hedley EL, Nunn AJ, Gleeson FV, et al. The relationship between chest tube size and clinical outcome in pleural infection. Chest 2010 Mar;137(3):536-543.
- 4. Bediwy AS, Amer HG. Pigtail catheter use for draining pleural effusions of various etiologies. ISRN Pulmonology 2012;2012:1-6.
- 5. Liu YH, Lin YC, Liang SJ, Tu CY, Chen CH, Chen HJ, et al. Ultrasound-guided pigtail catheters for drainage of various pleural diseases. Am J Emerg Med 2010 Oct;28(8):915-921.
- 6. Cooke DT, David EA. Large-bore and small-bore chest tubes: types, function, and placement. Thorac Surg Clin 2013 Feb;23(1):17-24.
- 7. McCracken DJ, Rahman NM. Chest drain size: does it matter? Eurasian J Pulmonol 2018;20(1):1-6.
- 8. Gammie JS, Banks MC, Fuhrman CR, Pham SM, Griffith BP, Keenan RJ, et al. The pigtail catheter for pleural drainage: a less invasive alternative to tube thoracostomy. JSLS 1999 Jan-Mar;3(1):57-61.
- 9. Jain S, Deoskar RB, Barthwal MS, Rajan KE. Study of pigtail catheters for tube thoracostomy. Med J Armed Forces India 2006 Jan;62(1):40-41.
- 10. Saricam M. Comparision of chest tube and intrapleural catheter applied for benign pleural effusions. J Ank Med Sch 2018;71(2):162-165.
- 11. Parulekar W, Di Primio G, Matzinger F, Dennie C, Bociek G. Use of small-bore vs large-bore chest tubes for treatment of malignant pleural effusions. Chest 2001 Jul;120(1):19-25.
- 12. Liang SJ, Tu CY, Chen HJ, Chen CH, Chen W, Shih CM, et al. Application of ultrasound-guided pigtail catheter for drainage of pleural effusions in the ICU. Intensive Care Med 2009 Feb;35(2):350-354.
- 13. Horsley A, Jones L, White J, Henry M. Efficacy and complications of small-bore, wire-guided chest drains. Chest 2006 Dec;130(6):1857-1863.
- 14. Lai YF, Chao TY, Wang YH, Lin AS. Pigtail drainage in the treatment of tuberculous pleural effusions: a randomised study. Thorax 2003 Feb;58(2):149-151.
- 15. Cafarotti S, Dall’Armi V, Cusumano G, Margaritora S, Meacci E, Lococo F, et al. Small-bore wire-guided chest drains: safety, tolerability, and effectiveness in pneumothorax, malignant effusions, and pleural empyema. J Thorac Cardiovasc Surg 2011 Mar;141(3):683-687.
- 16. Frost N, Brünger M, Ruwwe-Glösenkamp C, Raspe M, Tessmer A, Temmesfeld-Wollbrück B, et al. Indwelling pleural catheters for malignancy-associated pleural effusion: report on a single centre’s ten years of experience. BMC Pulm Med 2019 Dec;19(1):232.
- 17. Ekpe EE, Idongesit U. Significant pleural effusion in congestive heart failure necessitating pleural drainage. Nig J Cardiol 2015;12(2):106-110.
- 18. Ferreiro L, Porcel JM, Valdés L. Diagnosis and management of pleural transudates. Arch Bronconeumol 2017 Nov;53(11):629-636.
- 19. Sharaf-Eldin M, Bediwy AS, Kobtan A, Abd-Elsalam S, El-Kalla F, Mansour L, et al. Pigtail catheter: a less invasive option for pleural drainage in Egyptian patients with recurrent hepatic hydrothorax. Gastroenterol Res Pract 2016;2016.
- 20. Shetty S, Malik AH, Aronow WS, Alvarez P, Briasoulis A. Outcomes of thoracentesis for acute heart failure in hospitals. Am J Cardiol 2020;125(12):1863-1869.
- 21. Sabry ME, Hamad AM. Small bore catheter versus wide bore chest tube in management of malignant pleural effusions. J Egypt Soc Cardiothorac Surg 2012;20:197-201.
- 22. Davies HE, Merchant S, McGown A. A study of the complications of small bore ‘Seldinger’ intercostal chest drains. Respirology 2008 Jun;13(4):603-607.
- 23. Chang YC, Patz EF Jr, Goodman PC. Pneumothorax after small-bore catheter placement for malignant pleural effusions. AJR Am J Roentgenol 1996 May;166(5):1049-1051.
- 24. Morrison MC, Mueller PR, Lee MJ, Saini S, Brink JA, Dawson SL, et al. Sclerotherapy of malignant pleural effusion through sonographically placed small-bore catheters. AJR Am J Roentgenol 1992 Jan;158(1):41-43.
- 25. Hantera MA, Abdel-Hafiz H. Chest tube versus pigtail catheter in the management of empyema. Egypt J Chest Dis Tuberc 2019;68(3):390-393.
- 26. Kim SI, Kwak HJ, Moon JY, Kim SH, Kim TH, Sohn JW, et al. Cerebral air embolism following pigtail catheter insertion for pleural fluid drainage. Tuberc Respir Dis (Seoul) 2013 Jun;74(6):286-290.
- 27. Saqib A, Ibrahim U, Maroun R. An unusual complication of pigtail catheter insertion. J Thorac Dis 2018 Oct;10(10):5964-5967.