Miscarriage is considered a common pregnancy complication occurring in 14–20% of pregnancies.1 About 50% of women experiencing miscarriage experience psychological turmoil for weeks and even months following the loss of their pregnancy. Short-term depression and short-term anxiety symptoms have been reported in 20–55% and 20–40% of cases, respectively.2 About 10.9% women with miscarriage experience a major depressive episode in the six months after loss.3 Several risk factors cause psychiatric complications, including a history of psychiatric disorders, history of infertility, lack of social support or lack of marital satisfaction, history of fetal loss in previous pregnancies, as well as unintentional or unwanted pregnancies.4–8 Prior studies have suggested that experiencing high levels of anxiety and stress during pregnancy is associated with adverse birth outcomes.9 The results of a study showed that pregnant women with a history of spontaneous abortion are at risk of psychiatric morbidities in subsequent pregnancies.10 The findings of a meta-analysis study investigating the psychological reaction of patients after perinatal loss reported that psychiatric disorders occur in 27% of cases after miscarriage.11 The results of another recent meta-analysis study revealed that the incidence of miscarriage would lead to higher stress levels in women.12 Also, the occurrence of the previous miscarriage may be considered as a risk factor for increasing levels of distress in a consequent pregnancy, which in turn is associated with adverse pregnancy outcomes.12
Although many studies have emphasized the development of post-miscarriage psychological disorders, only a few studies have examined the effectiveness of interventions on the treatment of post-miscarriage psychological disorders. A previous review study on psychological consequences of miscarriage suggested that women, especially those with low social support, needed to receive psychological support based on their cultural context. Providing this care is regarded as an opportunity to provide information and explanations and to re-establish trust, thereby reducing mental disorders in women.13 The administration of three counseling sessions by a caregiver resulted in the resolution of grief among couples after miscarriage.14 The results of another study recommended that medical counseling, combined with psychological counseling, can be effective in mitigating women’s distress after miscarriage.15 However, the results of a systematic review on the Cochrane Library revealed that scarce evidence exists on the effectiveness of supportive psychological interventions after miscarriage.16
There are some uncertainties about the administration of psychological interventions after miscarriage. First, there is still not enough evidence demonstrating that psychological interventions are effective for improving women’s mental health after miscarriage. Further, the researchers are not sure about the kind of psychological intervention that is appropriate for women after miscarriage. Also, clinical trials introducing interventions with standard quality are rare or have not been performed recently. Eventually, there is no study exploring the effectiveness of brief psychological psychotherapy during the first 24 hours of hospitalization for women with miscarriage to prevent psychiatric morbidity at four-months follow-up. Accordingly, this study aimed to determine whether the administration of a two-hour brief supportive psychotherapy during the first 24 hours of hospitalization is effective in preventing anxiety, depression, and grief at four-months
post- miscarriage.
Methods
This randomized clinical trial was approved by the Ethics Committee of Babol University of Medical Sciences (Ref: No.3461) and was registered in the Iranian Registry of Clinical Trials under the number of IRCT201312255931N4.
The participants were recruited at the obstetrics ward in the Ayatollah Rohani teaching hospital affiliated with Babol University of Medical Sciences, from October 2016 to May 2018. The sample size was calculated based on the efficacy of psychotherapy on the prevention of anxiety and depression symptoms, and perinatal grief after pregnancy loss.15 Using an effect size of 65%, a confidence interval of 95% and 80% power, the sample size of each group was calculated as 40. The inclusion criteria for recruiting the subjects were as follows: being diagnosed with miscarriage (pregnancy loss under 20 weeks), a history of the first or second spontaneous abortion or induced abortion (therapeutic abortion, in response to a health condition of the women or fetus, or elective abortion, for other reasons), age between 18 and 40 years old, and those with at least five years of formal education. Patients who had recurrent abortions, were diagnosed with schizophrenia or bipolar disorders, and also those with a history of infertility were excluded from this study.
The midwives and nurses working obstetrics or high-risk pregnancy wards of the hospital were asked to invite the inpatients undergoing treatment for miscarriage to participate in the study. An explanation regarding the purpose and the procedure of the study was given to the staff to give to patients invited to participate in the study. Of the 105 women with miscarriage invited to the study, 14 women were excluded by the midwives/nurses because they did not meet the inclusion criteria. Finally, 79 with miscarriage were eligible to enter the study and completed an informed consent form [Figure 1].
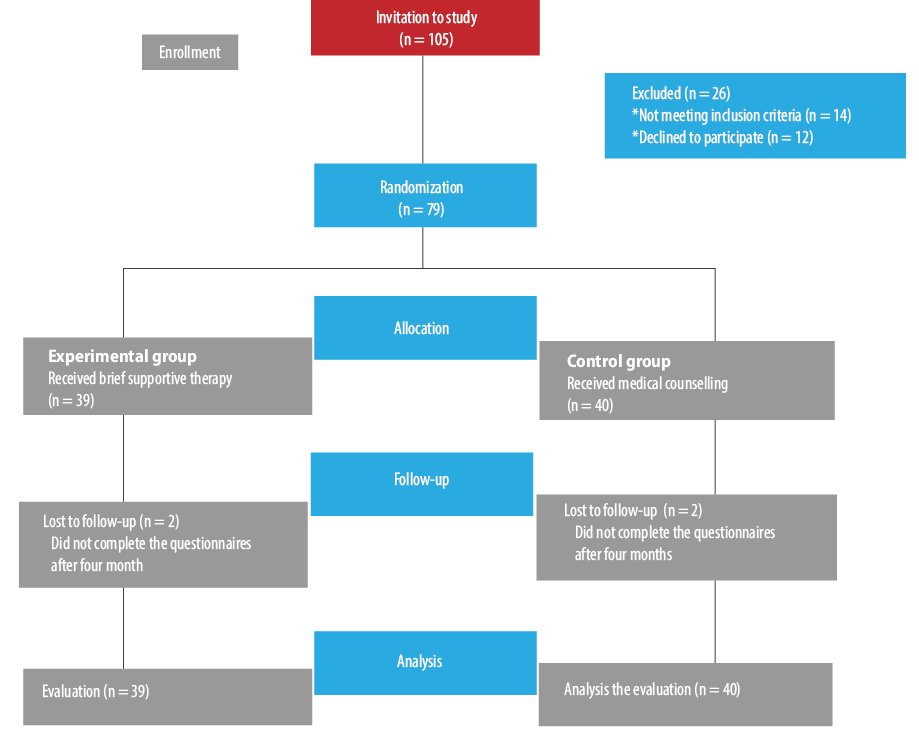
Figure 1: Flow chart of the subjects during the trial.
After completing patients’ obstetric history and performing baseline assessments, the patients were divided randomly into two groups; experimental group (brief psychotherapy) and control group (medical). An independent statistician made random allocation sequences using computer-generated numbers with equal probability (1:1) to either the intervention group or the control group. Allocation sequences were kept by the statistician and were not made available to any of the staff, patients, or researchers. The patients in both experimental and control groups received standard inpatient medical care for treatment of miscarriage. A midwife who was independent of the research team held an interview session with the patients. She assessed the patients in terms of inclusion and exclusion criteria and then recorded their demographic and obstetric information. She also asked the patients to complete two sets of questionnaires at the beginning and end of the study.
The midwife asked the patients to attend the obstetric clinic of the hospital four months after miscarriage. If the patients did not attend the clinic, the midwife called and asked them to complete the questionnaires and send them through e-mail. All patients completed all of the questionnaires of primary outcomes twice including the Hospital Anxiety and Depression Scale (HADS) and Perinatal Grief Scale (PGS) at the beginning of the study (before intervention) and at four-months post-miscarriage.
The HADS scale is a self-administered, practical, acceptable, reliable, valid, and easy to use instrument used to screen for the presence of depression and anxiety.17 The HADS is composed of two seven-item subscales including seven items for assessing anxiety and seven items for assessing depression. Items are rated on a four-point Likert scale. Both subscales are scored ranging from 0 to 21 with higher scores indicating more severe distress. The scores of each subscale can be interpreted as normal anxiety/depression (0 to 7), possible anxiety/depression (8 to 10), and probable anxiety/depression (> 10).17 We used the validated Persian version of the HADS in this study.18 The Cronbach’s alpha coefficient for the reliability of the HADS was equal to 0.810.
Toedter et al, designed the PGS to measure the degree of grief after perinatal loss.19 It is composed of 33 items on a five-point Likert scale, with scores ranging from 33 to 165. PGS consists of three subscales including active grief, difficulty coping, and despair. Each subscale consists of 11 items, with scores ranging from 11 to 55. Higher scores reflect more intense grief.19 We used the validated Persian version of PGS in this study.20 The cut-off score of 91 in PGS is considered as abnormal grief symptoms.21 The Cronbach’s alpha coefficient for the reliability of the PGS was equal to 0.944.
We also assessed the proportion of women whose anxiety symptoms, depression symptoms, and perinatal grief were resolved four months after miscarriage. The frequency of anxiety symptoms, depression symptoms, and perinatal grief in the experimental and control groups was also assessed as secondary outcomes.
The method of intervention, brief supportive psychotherapy (BSP), was developed based on the Winston’s supportive psychotherapy.22 BSP is a non-directive patient approach, though the therapist deals with the patient’s affect. The common elements of BSP approach for treatment include making an emotional connection, following the affect, letting it linger, encouraging catharsis, building alliance, and emphasizing the patient’s strengths (but not avoiding negative affect).
A BSP psychotherapist builds the therapeutic alliance through three core techniques including allowing the patient to set the course of treatment, listening to him/her carefully, and reflecting back the affect to the patient with careful clarifications. BSP helps the patients to develop a new skill for identifying and describing their emotions. BSP therapist assigns no homework for the patients. Although a BSP therapist provides a little psychoeducation about the target disorder, there is no attempt to urge the patient to ‘do’ anything rather than reflecting on his or her emotions. A BSP therapist helps the patients to experience a new understanding of one’s world, clarify symptoms and problems, inspire hope, facilitate experiences of success or mastery, and alleviate the patients’ anxiety regarding the power to change them or their environment.23
A female psychologist who was trained based on the BSP approach conducted the sessions for the entire course of the study. Each session lasted two hours. The psychologist held the psychotherapy session with the patient in a private room in the hospital during the first 24 hours of hospitalization. She received supervision by conducting supervision sessions once a week by the help of an experienced psychotherapist in obstetrics field. A placebo two-hour counseling session was held by a midwife in a private room during the first 24 hours of hospitalization. In this session, the midwife encouraged the patient to talk about the experience of the miscarriage and to ask the medical questions about the miscarriage. The midwife answered the inquiries of the patients, assessed the results and implications with respect to the medical management after miscarriage, as well as aspects for planning the future pregnancies and controlling general health.
Standard medical care was provided for inpatient women with miscarriage based on the recent recommendations proposed by The American College of Obstetricians and Gynecologists (2015) for management of pregnancy loss.24,25
For comparison of two groups at baseline, categorical data were expressed as numbers and percentages which were compared using the chi-square test. Continuous data were also expressed as means±standard deviations and compared using the Student’s t-test.
The scores of perinatal grief, depression, and anxiety at follow-up were assessed for obtaining primary outcomes. The Kolmogorov-Smirnov test was performed to test the normal distribution of the variables. All of the outcome variables for analysis had normal distribution except for differences between two groups. Therefore, we used both t-test and paired t-test for all of the outcome variables. Paired t -test was applied to compare changes within groups (before and four-months post-miscarriage). Also, the t-test was used to compare the changes between groups. As the variable ‘difference changes’ had abnormal distribution, we used the Mann-Whitney U test to compare the difference changes between the two groups.
The potential effect of the intervention was estimated by generalized estimating equations (GEE). The interaction effect between changes in groups and time was assessed using GEE. The use of GEE is preferable to the repeated-measures analysis of variance for pre- and post-analysis, as it allows including all randomized participants in the analysis and less bias due to lack of follow-up data.26 As there were three missing data at the follow-up time (two people in the control group and one person in experimental group), GEE was found to be superior method to assess the effect of the intervention. The total score of the perineal grief, three subscales of grief (active grief, difficulty, despair), anxiety score, depression score, and total score of depression/anxiety were included in GEE models.
Difference in the prevalence frequency of psychiatric morbidities was assessed for obtaining secondary outcomes between experimental and control groups. Thus, the proportion of women whose symptoms were resolved was assessed according to a score of 7 or less on the depression/anxiety scale and a score ≥ 91 on the PGS.17,21 We evaluated the difference between experimental and control groups regarding the prevalence frequency of psychiatric morbidities using the chi-square test.
The alpha level was set to 0.050. Data were analyzed using SPSS Statistics (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp).
Results
The characteristics of the patients are shown in Table 1. There were no significant differences between experimental and control groups at baseline in terms of the demographic characteristics.
Table 1: Characteristics of the study population.
|
Gestational
age, mean ±
SD, years |
19.4 ± 8.1 |
17.2 ± 9.6 |
0.140 |
|
Education,
years |
|
|
|
|
≤ 12 |
29 (76.3) |
30 (85.7) |
0.195 |
|
> 12 |
9 (23.7) |
5 (24.3) |
|
Number of
children |
|
|
|
|
0 |
14 (35.9) |
12 (30.0) |
0.566 |
|
1 |
16 (41.0) |
19 (47.5) |
|
> 2 |
9 (23.1) |
9 (22.5) |
|
Abortion type |
|
|
|
|
Induced** |
3 (7.7) |
5 (12.5) |
0.464 |
|
Spontaneous |
36 (92.2) |
35 (870) |
|
Number of
abortions |
|
|
|
|
0 |
26 (66.7) |
33 (82.5) |
Data given as n (%) unless otherwise stated.
SD: standard deviation.
*There are missing values for some variables.
**Termination of pregnancy under 20 weeks due to maternal or fetal reasons.
The results of paired t-test revealed that the participants receiving BSP reported significant reductions in mean scores of active grief, difficulty coping, despair, and total perinatal grief score in the follow-up [Table 2]. In contrast, the participants in the control group did not report significant reductions in the mean scores of active grief, difficulty coping, despair, and total perinatal grief score in the follow-up. Also, there was a significant reduction in depression score, anxiety score, total anxiety/depression score at follow-up in the experimental group, while the control group reported no reduction in this regard.
Table 2: Comparison of mean scores of perinatal grief, depression, and anxiety within and between groups.
|
Active |
34.2
(9.7) |
28.1
(6.9) |
-0.5*
(0.8) |
37.2
(6.3) |
35.0
(10.2) |
-0.1
(0.7) |
-0.35
(-0.72 to 0.01) |
0.001 |
0.009 |
|
Difficulty |
27.1
(6.4) |
23.3
(4.3) |
-0.3*
(0.5) |
30.7
(4.7) |
29.9
(7.8) |
-0.0
(0.4) |
-0.27
(-0.50 to -0.03) |
0.010 |
< 0.001 |
|
Despair |
28.0
(8.4) |
22.8
(5.2) |
-0.4*
(0.8) |
30.3
(5.6) |
27.5
(8.4) |
-0.2
(0.6) |
-0.22
(-0.55 to 0.11) |
0.048 |
0.032 |
|
Total perinatal grief |
89.6
(23.1) |
74.4
(15.3) |
-0.4
(0.6) |
98.1
(14.7) |
92.5
(25.9) |
-0.1
(0.6) |
-0.29
(-0.57 to -0.01) |
0.003 |
0.003 |
|
Depression |
6.4
(2.7) |
3.5
(3.3) |
-0.4*
(0.5) |
7.9
(3.1) |
8.0
(3.8) |
-0.0
(0.4) |
-0.41
(-0.65 to -0.18) |
< 0.001 |
0.004 |
|
Anxiety |
9.4
(3.0) |
6.4
(3.1) |
-0.4*
(0.4) |
10.3
(3.0) |
10.1
(4.4) |
-0.0
(0.4) |
-0.40
(-0.60 to -0.20) |
< 0.001 |
< 0.001 |
*reflects a pair t-test (comparing within the groups) is significant.
**differences changes of means between the groups.
***p-values of the Mann-Whitney U test for significantly of differences changes.
****p-value indicates interaction of groups and time using generalized estimating equations (GEE).
CI: confidence interval
Table 3: Psychiatric symptoms at four-months post-miscarriage in the control and experimental groups.
|
Anxiety symptoms |
|
|
|
|
No |
32 (86.5) |
15 (39.5) |
0.015 |
|
Yes |
5 (13.5) |
23 (60.5) |
|
Depressive symptoms |
|
No |
25 (67.6) |
11 (28.9) |
0.001 |
|
Yes |
12 (32.4) |
27 (71.1) |
|
High perinatal
grief symptoms |
|
|
|
|
No |
33 (89.2) |
13 (34.2) |
Anxiety symptom (yes: HADS anxiety score < 7, no: HADS anxiety score >7); depressive symptoms (yes: HADS anxiety score < 7, no: HADS anxiety
score >7); total scores of anxiety and depression (normal < 21, abnormal >21); grief symptoms (high when PGS > 91 and low when PGS < 91).
The results of the GEE model for mean differences between two groups in the follow-up are presented in Table 2. The results of GEE model indicated that the BSP caused a significant decline in the scores of subscales including active grief, difficulty coping, despair, and total perinatal grief in the experimental group compared to the control group in the follow-up period (p < 0.050). Also, we found a difference in improvement of perinatal grief between the experimental and control groups in the follow-up. There was also a difference in the results of GEE for each group over time of the trial. Indeed, the mean scores of depression and anxiety symptoms decreased significantly in the experimental group compared to the control group from baseline to follow-up (p < 0.001). Note that the control group did not show any significant improvement in depression and anxiety symptoms from baseline to follow-up.
Table 3 compares the frequency of the psychiatric symptoms between the two groups in the four-month follow-up. The frequency of anxiety symptoms was significantly lower in the experimental group than in the control group (13.5% vs. 60.5%). Also, the frequency of depressive symptoms was significantly lower in the experimental group than in the control group (32.4% vs. 71.1%). Finally, the results indicated that the participants in the experimental group experienced lower levels of grief than in the control group in the follow-up at four months (10.8% vs. 65.8%).
Discussion
Our findings suggest that the administration of BSP has a significant improvement in anxiety and depression symptoms in women who experienced miscarriage at four-months follow-up compared to those who did not receive psychotherapy. The administration of BSP reduced the total scores of perinatal grief and the three subscales (active grief, difficulty coping, and despairs) in the experimental group compared to the control group. Our study is the first randomized control trial (RCT) suggesting that holding two-hour sessions of BSP during the first 24 hours of hospitalization can be effective in the prevention of psychiatric symptoms after miscarriage. Further, our study suggests that the introduction of psychotherapy in the experimental group appears to have prevented the development of grief reaction or anxiety and
depression symptoms.
Some RCTs have investigated the effects of administration of psychotherapy on prevention of psychiatric morbidity after miscarriage.26–29 The results of a meta-analysis study supported that psychological interventions may improve psychological well-being of pregnant women after miscarriage.12 One study conducted in 2007 compared the effect of psychological intervention and medical intervention on women’s distress who were referred for a routine scan at 10–14 weeks gestation and were diagnosed with miscarriage. The authors concluded that psychological intervention coupled with medical counseling was beneficial in reducing psychological adverse complications after miscarriage.15 The methodology of this study differed from ours, which may have led to the different outcomes. The first difference was the study population; the 2007 study included patients referred within five weeks of miscarriage, while our study included the patients with miscarriage hospitalized after surgical evacuation or medical management with BSP conducted within the first 24 hours of admission. The second difference resulted from the use of different interventions. In the 2007 study, the experimental group received a 50-minute session of psychological counseling by a psychologist, while our study conducted a two-hour session of BSP. Thirdly, the design of the 2007 study was prospective, while this study was a RCT with a control group who received a placebo intervention similar to experimental group (two-hour session of medical intervention by a midwife).15
Another study investigated whether a structured follow-up visit to a midwife at 21–28 days after early miscarriage could reduce the women’s grief. The results showed that the scores of active grief and difficulty coping subscales changed significantly after the intervention. Our study had some differences, which may have led to the different results. While the first study included patients with early miscarriage before 13 weeks, our study included patients that miscarried before 20 weeks. Further, the first study gave the experimental group a 50-minute session of medical intervention by a midwife and the control group received 30-minute sessions of counseling by a midwife, while our study conducted a two-hour session of psychotherapy for patients by a psychologist with the control group receiving a placebo intervention.30
Lee et al,31 investigated whether the administration of a psychological debriefing process has a positive effect on reduction of emotional consequences (anxiety and depression) using the HAD scale. They concluded that the administration of psychological debriefing did not cause improvement in the emotional consequences. Our study had some differences with the study by Lee et al,31 which may have led to the inconsistent results. First, in the study by Lee et al,31 a psychologist conducted one-hour counseling sessions at patients’ home two weeks after the miscarriage and we conducted two-hour sessions of BSP in the hospital during the first 24 hours of hospitalization. Secondly, in the study by Lee et al, the control group did not receive any intervention.
However, the results of our study are not consistent with some of the previous research in terms of the improvement of symptoms of anxiety, depression, and perinatal grief after psychotherapy.
A meta-analysis study concluded that there was not enough evidence to show whether psychological follow-up improves the well-being of women with pregnancy loss.32 Also, the results of another systematic review revealed that there is lack of evidence to support that psychological follow-up is useful for improving women’s well-being after miscarriage.16
Some studies reported different psychotherapy interventions for improving complicated grief. For example, one study concluded that psychotherapy based on grief treatment was superior to interpersonal psychotherapy in treatment of patients with complicated grief.33 To the best of our knowledge, there is no published study reporting the effectiveness of brief psychotherapy intervention with a specific approach.
Another question is how BSP can prevent anxiety symptoms, depression symptoms, and perinatal grief in the four-month follow-up. Although the mechanism of the effect of BSP on prevention of psychiatric symptoms is not yet clear, some hypotheses have been proposed. The first assumption is related to the nature of the therapeutic approach. A BSP psychotherapist listens to emotional disturbances carefully, follows the patient’s affect, reflects the affects, and helps the patients to develop a new skill for identifying and describing their emotions. The second assumption is related to the time of intervention, which was the first 24 hours after the loss - a golden time to release the negative effect. Also, the duration of the intervention, which was a long two-hour session, may have helped the patient to release the negative effects and restructure their thoughts to cope with the loss. Therefore, the match between the nature of miscarriage (a high negative effect) and nature the psychotherapy method, which was a long session (two hours) with golden time of intervention (first 24-hours post-loss) may have led to the effect of BSP on prevention of anxiety symptoms, depression symptoms, and perinatal grief at four-months follow-up.
Our study had some limitations. First, our small sample size and short follow-up time are considered limitations. Further studies are required to find the effectiveness of administering BSP with a larger sample size in long-term follow-up periods. Further, our study did not provide any detailed information on psychological counseling or medical treatment during the follow-up period. Thus, it was not possible to assess whether differences between experimental and control groups in co-treatment could have explained some of our results. In addition, the results were obtained from self-report measures. It is suggested to conduct further studies on the clinical prevention of psychiatric morbidities developing after miscarriage to obtain definitive results. Moreover, further research is needed to compare the effect of BSP with other psychotherapy interventions in improvement of women’s well-being after miscarriage. Future research should also confirm the findings of our study to test potential moderators influencing psychotherapy response and to improve the acceptance of therapy model.
Conclusion
BSP is an efficacious and reliable intervention for preventing depressive symptoms, anxiety symptoms, and high level of grief after miscarriage. The findings of this study suggested that miscarriage is considered a specific condition that needs early brief psychological counseling during the first 24 hours of admission in hospital to prevent anxiety, depression, and perinatal grief by four-months post-loss.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
Acknowledgements
The authors thank all of the patients who took part in the present study.
references
- 1. Farquharson RG, Jauniaux E, Exalto N; ESHRE Special Interest Group for Early Pregnancy (SIGEP). Updated and revised nomenclature for description of early pregnancy events. Hum Reprod 2005 Nov;20(11):3008-3011.
- 2. Janssen HJ, Cuisinier MC, Hoogduin KA, de Graauw KP. Controlled prospective study on the mental health of women following pregnancy loss. Am J Psychiatry 1996 Feb;153(2):226-230.
- 3. Lok IH, Neugebauer R. Psychological morbidity following miscarriage. Best Pract Res Clin Obstet Gynaecol 2007 Apr;21(2):229-247.
- 4. Faramarzi M, Pasha H. The role of social support in prediction of stress during pregnancy. JBUMS 2015;17(11):52-60.
- 5. Neugebauer R, Kline J, Shrout P, Skodol A, O’Connor P, Geller PA, et al. Major depressive disorder in the 6 months after miscarriage. JAMA 1997 Feb;277(5):383-388.
- 6. Goff BS, Smith DB. Systemic traumatic stress: the couple adaptation to traumatic stress model. J Marital Fam Ther 2005 Apr;31(2):145-157.
- 7. Lok IH, Yip AS, Lee DT, Sahota D, Chung TK. A 1-year longitudinal study of psychological morbidity after miscarriage. Fertil Steril 2010 Apr;93(6):1966-1975.
- 8. Thapar AK, Thapar A. Psychological sequelae of miscarriage: a controlled study using the general health questionnaire and the hospital anxiety and depression scale. Br J Gen Pract 1992 Mar;42(356):94-96.
- 9. Hasanjanzadeh P, Faramarzi M. Relationship between maternal general and specific-pregnancy stress, anxiety, and depression symptoms and pregnancy outcome. J Clin Diagn Res 2017 Apr;11(4):VC04-VC07.
- 10. Haghparast E, Faramarzi M, Hassanzadeh R. Psychiatric symptoms and pregnancy distress in subsequent pregnancy after spontaneous abortion history. Pak J Med Sci 2016 Sep-Oct;32(5):1097-1101.
- 11. Adolfsson A. Meta-analysis to obtain a scale of psychological reaction after perinatal loss: focus on miscarriage. Psychol Res Behav Manag 2011;4:29-39.
- 12. San Lazaro Campillo I, Meaney S, McNamara K, O’Donoghue K. Psychological and support interventions to reduce levels of stress, anxiety or depression on women’s subsequent pregnancy with a history of miscarriage: an empty systematic review. BMJ Open 2017 Sep;7(9):e017802.
- 13. Van den Akker OB. The psychological and social consequences of miscarriage. Expert Rev Obstet Gynecol 2011;6(3):295-304.
- 14. Swanson KM, Chen HT, Graham JC, Wojnar DM, Petras A. Resolution of depression and grief during the first year after miscarriage: a randomized controlled clinical trial of couples-focused interventions. J Womens Health (Larchmt) 2009 Aug;18(8):1245-1257.
- 15. Nikcević AV, Kuczmierczyk AR, Nicolaides KH. The influence of medical and psychological interventions on women’s distress after miscarriage. J Psychosom Res 2007 Sep;63(3):283-290.
- 16. Murphy FA, Lipp A, Powles DL. Follow-up for improving psychological well being for women after a miscarriage. Cochrane Database Syst Rev 2012 Mar;3(3):CD008679.
- 17. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983 Jun;67(6):361-370.
- 18. Montazeri A, Vahdaninia M, Ebrahimi M, Jarvandi S. The Hospital Anxiety and Depression Scale (HADS): translation and validation study of the Iranian version. Health Qual Life Outcomes 2003 Apr;1(1):14.
- 19. Toedter LJ, Lasker JN, Alhadeff JM. The Perinatal Grief Scale: development and initial validation. Am J Orthopsychiatry 1988 Jul;58(3):435-449.
- 20. Siadatnezhad S, Ziaei T, Khoori E, Vakili MA, Lasker J. Translation and validation of the persian version of the perinatal grief scale in Iranian mothers with an experience of pregnancy loss. Middle East J Famil Med 2018;16(1):55-61.
- 21. Bennett SM, Litz BT, Maguen S, Ehrenreich JT. An exploratory study of the psychological impact and clinical care of perinatal loss. J Loss Trauma 2008;13(6):485-510.
- 22. Winston A, Rosenthal RN, Pinsker H. Learning supportive psychotherapy: An illustrated guide. American Psychiatric Pub; 2011.
- 23. Markowitz JC. What is supportive psychotherapy? Focus 2014;12(3):285-289.
- 24. American College of Obstetricians and Gynecologists. Early pregnancy loss. Practice Bulletin No. 150. Obstet Gynecol 2015;125:1258-1267.
- 25. Tunçalp O, Gülmezoglu AM, Souza JP. Surgical procedures for evacuating incomplete miscarriage. Cochrane Database Syst Rev 2010 Sep;(9):CD001993.
- 26. Moudi Z, Talebi B, Faramarzi M, Ansari H. Studying the effect of a supportive communication techniques program on the quality gap among women who gave birth in local childbirth outposts, south-east. Iran J Public Health 2019; 1-8.
- 27. Luise C, Jermy K, May C, Costello G, Collins WP, Bourne TH. Outcome of expectant management of spontaneous first trimester miscarriage: observational study. BMJ 2002 Apr;324(7342):873-875.
- 28. Neilson JP, Hickey M, Vazquez J. Medical treatment for early fetal death (less than 24 weeks). Cochrane Database Syst Rev 2006 Jul;(3):CD002253.
- 29. Zhang J, Gilles JM, Barnhart K, Creinin MD, Westhoff C, Frederick MM. A comparison of medical management with misoprostol and surgical management for early pregnancy failure. Obstet Gynecol Surv 2006;61(2):110-111.
- 30. Adolfsson A, Berterö C, Larsson PG. Effect of a structured follow-up visit to a midwife on women with early miscarriage: a randomized study. Acta Obstet Gynecol Scand 2006;85(3):330-335.
- 31. Lee C, Slade P, Lygo V. The influence of psychological debriefing on emotional adaptation in women following early miscarriage: a preliminary study. Br J Med Psychol 1996 Mar;69(Pt 1):47-58.
- 32. Flenady V, Wilson T. Support for mothers, fathers and families after perinatal death. Cochrane Database Syst Rev 2008 Jan;(1):CD000452.
- 33. Shear K, Frank E, Houck PR, Reynolds CF III. Treatment of complicated grief: a randomized controlled trial. JAMA 2005 Jun;293(21):2601-2608.