| |
Abstract
Giant cell fibroblastoma is a rare intermediate grade soft tissue tumor of childhood which characteristically occurs in males during the first decade of life. It has high incidence of local recurrence but metastasis has never been reported. Giant cell fibroblastoma merits attentive interpretation as they have been misdiagnosed as sarcoma in the past leading to erroneous remedies. Here we are reporting a case of giant cell fibroblastoma in a 3-year-old boy who presented with a painless swelling over the medial aspect of right ankle forthe last five months.
Keywords: Fibroblastoma; Giant cell; Soft tissue tumor.
Introduction
Giant cell fibroblastoma is an unusual childhood fibrohistiocytic tumor of intermediate malignancy. It was originally described by Schmookler and Enzinger in 1982,1 following which around 100 cases have been reported. Giant cell fibroblastoma characteristically occurs in males during the first decade of life, with more than half of cases seen before the age of 5 years.2 Giant cell fibroblastoma merits attentive interpretation as they have been misdiagnosed as sarcoma in the past leading to erroneous remedies. We are hereby reporting a case of giant cell fibroblastoma in a 3-year-old boy who presented with a painless swelling over the medial aspect of right ankle for the last five months.
Case Report
A 3-year-old boy presented with painless swelling at the medial aspect of right ankle for the last five months. Initially, the swelling was small and gradually increased to the present size of 2 × 2 cms. There was no history of trauma, fever, restriction of movements or any other swelling. On local examination, a soft, nontender, freely mobile swelling of 2 × 2 cms was present at medial aspect of right ankle. The swelling was not fixed to skin and there was no sinus or ulcer present over it. Hematological profile and all other investigations were within normal limits. An initial clinical diagnosis of lipomatous tumor was made and wide excision of swelling was done with split thickness skin grafting.
Gross specimen comprised a single, well-circumscribed, skin- covered, creamish white tissue piece measuring 2 × 1.8 × 1.4 cm and appeared gelatinous on cut section. (Fig. 1)

Figure 1: Gross cut section of skin covered well circumscribed creamish white gelatinous tissue piece.
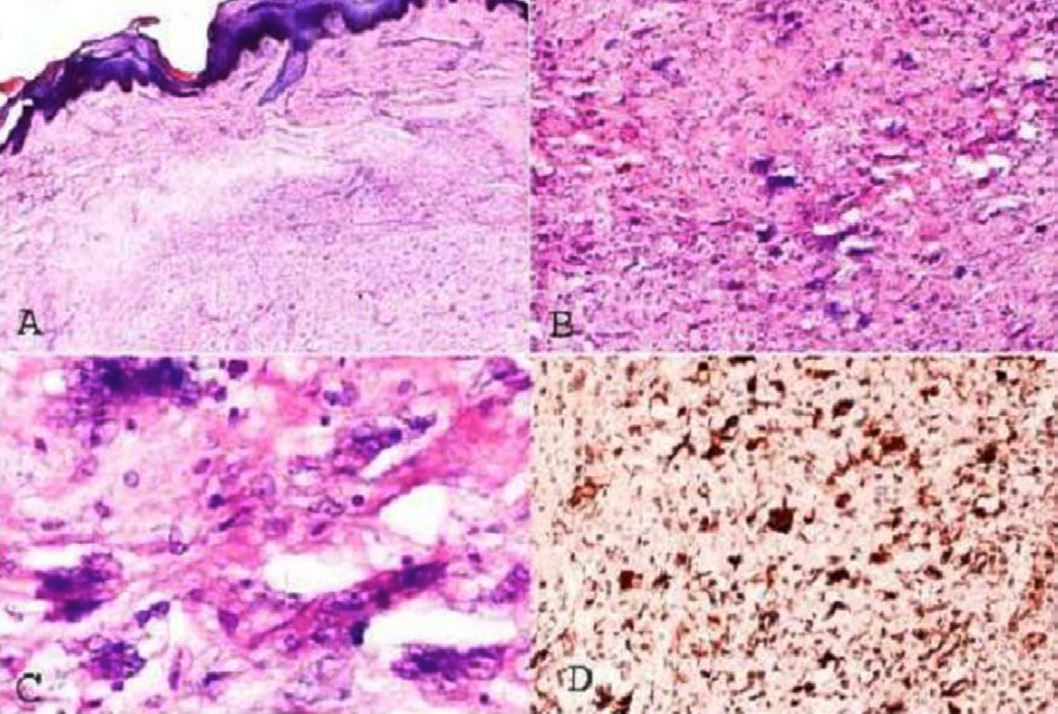
Figure 2: Microscopy of giant cell fibroblastoma. Hematoxylin and eosin-stained section showing stratified squamous epithelium and underlying dermal fibromyxoid component with infiltrate of spindle cells and floret like giant cells (A × 40). Slit like spaces lined by floret-like giant cells in a fibromyxoid stroma (B × 100, C × 400). Immunohistochemistry showing vimentin positive spindle cells and giant cells (D × 40).
Histopathologically, the section showed dermal infiltrate of fibroblast and floret-like giant cells in a fibromyxoid stroma (Fig. 2A). The spindle cells were arranged diffusely or in vague fascicles, their nuclei were elongated and had vesicular to hyperchromatic chromatin. The cytoplasm was scanty and eosinophilic. The giant cells contained a variable number of round to oval vesicular nuclei and had abundant amphophilic cytoplasm with irregular cytoplasmic contours. There were slit-like sinusoidal spaces lined by floret-like giant cells (Figs. 2B, 2C). Immunohistochemistry showed fibroblast and giant cells reactivity for vimentin but were negative for CD68 (Fig. 2D). Patient was regularly followed up and doing fine for the last six months.
Discussion
Giant cell fibroblastoma (GCF) is an intermediate grade, soft tissue tumor of childhood with high incidence of local recurrence. Metastasis has never been reported. It shows a male preponderance with majority of cases seen during the first decade of life.3-5 Clinically, the patient usually presents with a small, painless, slow growing soft tissue swelling which has a predilection for back and thigh.5 Other less common sites include anterior chest, shoulder, perineum, and extremities.5
The histogenesis of giant cell fibroblastoma has been a topic of considerable debate amongst researchers. Ultra structural studies have, however, demonstrated the fibroblastic differentiation.6 When grossly examined, giant cell fibroblastoma appears as an unencapsulated, gray-white, gelatinous lesion. Fine needle aspiration cytology of giant cell fibroblastoma shows hypocellular to moderately cellular smears consisting of clusters of small spindle or oval cells with minimal amphophilic cytoplasm lying in a background of metachromatic matrix. Rare multinucleated giant cells with floret like arrangement of nuclei are also seen.2,7
Histologically, these lesions show a variable degree of cellularity with a fibromyxoid to hyalinized stroma containing bland spindle cells and multinucleated giant cells. The spindle cells may demonstrate mild to moderate pleomorphism and are arranged diffusely or in vague fascicles, their elongated nuclei has vesicular to hyperchromatic chromatin. The cytoplasm is usually scanty and eosinophilic. The giant cells contain a variable number of round to oval vesicular nuclei and have abundant amphophilic cytoplasm with irregular cytoplasmic contours. Slit like sinusoidal spaces lined by either a continuous or discontinuous layer of multinucleated giant cell is a unique and diagnostic feature of giant cell fibroblastoma.3,4
Previously, giant cell fibroblastomas were considered as a juvenile form of dermatofibrosarcoma protuberans (DFSP) but recent studies suggests that both these lesions are on a spectrum of same entity as confirmed by clinical, morphological, immunophenotypical and molecular studies.3,6 Both lesions share common clinical features of male predominance, slow growth, painlessness, and anatomical location of mainly trunk. Morphologically, both GCF and DFSP shows mainly dermal or subcutaneous location and rarely superficial skeletal muscle involvement, honeycomb and parallel growth patterns, sparing of adnexa, myxoid changes and prominent vasculature.6
By using immunohistochemistry, both lesions show positive staining for CD34 and negative reaction to keratin, S-100, HMB-45, smooth muscle actin and desmin. Cytogenetically, t(17;22) translocation is seen in both giant cell fibroblastoma and dermatofibrosarcoma protuberans.6 Although both giant cell fibroblastoma and dermatofibrosarcoma protuberans share several clinical as well as morphological features, we still differentiate them solely on the basis of histological findings. The presence of pseudovascular spaces lined by giant cells, solid areas with stromal giant cells, consistent hemorrhage, perivascular and onion skin- like chronic inflammation without storiform pattern favors the diagnosis of giant cell fibroblastoma.6
Vimentin is the only immunohistochemical detection marker that has been found to consistently stain giant cell fibroblastoma.4 Treatment includes removal of the tumor with wide excision and these patients do not require any form of chemotherapy.8 Mohs' micrographic surgery has been advocated for recurrent giant cell fibroblastoma.9 Although local recurrence is common, long term outcome of this tumor is very good after reēxcision of the tumor.
Due to its rarity and unfamiliarity, GCF was misdiagnosed in the past as sarcoma, which leads to aggressive therapy for this tumor. Shmooker et al. in their study of 28 cases of GCF revealed that 14 cases were initially diagnosed as sarcoma which led to wider surgical reexcision in four patients, one of whom also received radiation therapy.4 Abdul-Karim et al. in their report of three cases of giant cell fibroblastoma misdiagnosed two cases as sarcomas which led to more aggressive therapy.10
The differential diagnoses of giant cell fibroblastoma includes liposarcoma,myxofibrosarcoma, malignant fibrous histiocytoma and papillary intralymphatic angioendothelioma. Liposarcoma can be differentiated by identification of lipoblast, absence of slit-like sinusoidal spaces, and occurrence of this lesion in adulthood. Myxofibrosarcoma can be differentiated by its deeper location and occurrence in older patients. Malignant fibrous histiocytoma is characterised by markedly atypical mesenchymal cells, frequent mitotic figures, absence of sinusoidal spaces, and rarity of this neoplasm in childhood. Papillary intralymphatic angioendothelioma can be differentiated by positive vascular markers and absence of myxoid and cellular areas in this tumor.3,6
Conclusion
Giant cell fibroblastoma is a rare childhood tumor of intermediate grade malignancy which share several features with dermatofibrosarcoma protuberans. Despite having many modern diagnostic modalities at our hand, we still differentiate these two lesions solely on histological examination and all that we need is thorough histopathological examination of the entire tumor mass.
Acknowledgements
The authors reported no conflict of interest and no funding was received on this work.
|
|
| |
References
1. Shmookler BM, Enzinger FM. Giant cell fibroblastoma. A peculiar Childhood tumor. Lab Invest 1982;46:76.
2. Maitra A, Timmons CF, Siddiqui MT, Saboorian MH. Fine-needle aspiration biopsy features in a case of giant cell fibroblastoma of the chest wall. Arch Pathol Lab Med 2001 Aug;125(8):1091-1094.
3. Shmookler BM, Enzinger FM, Weiss SW. Giant cell fibroblastoma. A juvenile form of dermatofibrosarcoma protuberans. Cancer 1989 Nov;64(10):2154-2161.
4. Vargas-Gonzalez R, Solis-Coria A. Giant cell fibroblastoma in a 3-year-old boy. Pathol Oncol Res 2003;9(4):249-251.
5. Chou P, Gonzalez-Crussi F, Mangkornkanok M. Giant cell fibroblastoma. Cancer 1989 Feb;63(4):756-762.
6. Jha P, Moosavi C, Fanburg-Smith JC. Giant cell fibroblastoma: an update and addition of 86 new cases from the Armed Forces Institute of Pathology, in honor of Dr. Franz M. Enzinger. Ann Diagn Pathol 2007 Apr;11(2):81-88.
7. Layfield LJ, Gopez EV. Fine-needle aspiration cytology of giant cell fibroblastoma: case report and review of the literature. Diagn Cytopathol 2002 Jun;26(6):398-403.
8. Nair R, Kane SV, Borges A, Advani SH. Giant cell fibroblastoma. J Surg Oncol 1993 Jun;53(2):136-139.
9. Najarian DJ, Morrison C, Sait SN, Meguerditchian AN, Kane J III, Cheney R, et al. Recurrent giant cell fibroblastoma treated with Mohs micrographic surgery. Dermatol Surg 2010 Mar;36(3):417-421.
10. Abdul-Karim FW, Evans HL, Silva EG. Giant cell fibroblastoma: a report of three cases. Am J Clin Pathol 1985 Feb;83(2):165-170.
|
|