Inborn errors of metabolism (IEM) can be defined as a large group of inherited or genetic disorders caused by enzyme or protein transport defects leading to a block in different metabolism pathways. The problems are usually due to an accumulation of toxic substances, or to the effects of decreased synthesis of essential compounds.1
IEM has a wide range of clinical presentation, which varies with different age groups depending on the severity of the enzyme’s defect or deficiency. Complete deficiency of one enzyme will lead to severe and early presentation in the neonatal period while a partial lack will lead to later presentation in infants and children. A high index of suspicion based on clinical presentation is required to raise the diagnosis of IEM.2
Tandem mass spectrometry (MS/MS) is an important new technology for neonatal screening and diagnosis of IEM. It allows the detection and quantification of many IEM in a single blood spot. Additionally, MS/MS has introduced the concept of multiple metabolite analyses for the detection of numerous metabolic disorders in a single analytical run.3 In the last decades, different studies recognize the role of newborn screening using MS/MS.4–7
Iraq is a country in the Middle East countries consisting of 18 provinces with a population more than 37 million. Misan is located in the South East of Iraq with a population of more than 1.1 million reported in 2016.8 Most of the people there are belonged to tribes with a high frequency of consanguineous marriages. However, there was limited data about this rate in Misan. But, in general, a high rate of consanguinity was recorded in Iraq reaching an average of 47–60%, which may be related to the social, cultural, religious, and political factors.9
To date, in Iraq only two provinces (Baghdad and Karbala) had applied a newborn screening (which was started at 2013).
Unfortunately, screening programs are limited in their application and are restricted to screening phenylketonuria, galactosemia, and congenital hypothyroidism only.10 Early suspicion, diagnosis, and treatment of metabolic disorders will change the overall picture and even mortality rates.2,11 So some patients may have a normal life, and in others the irreversible brain damage and neurological disabilities can be avoided if early treatment is initiated.2,12
For these reasons, our study sought to estimate the prevalence and type of IEM in children with unexplained developmental delay and to highlight the importance of early diagnosis and treatment in this group to avoid these consequences.
Methods
A cross-sectional study with analytical elements was carried out in Misan Hospital for Child and Maternity in Misan province over one year (from 1 April 2017 to 1 April 2018). A total of 112 children with unexplained developmental delay were included in this study whether attending Misan Hospital for Child and Maternity or a private clinic as outpatient visitors or inpatient admissions to the pediatrics ward.
We included children between the ages of one month and eight years old with significant developmental delays. Specifically, children with delays in language or speech, cognitive, motor, and/or social development.
The data were collected through face-to-face interviews with the parents. The questionnaire included the patient’s full name, age (date of birth), gender, consanguinity, and family history (of the same condition, unexplained death, unexplained neurodevelopmental delay, or genetic disease). In addition, the results of computed tomography (CT) scan of the brain were recorded (the presence of brain atrophy or other abnormalities). Moreover, other data were needed for MedLabs’ Referral Laboratory, which included the mother’s name, patient’s weight, gestational period (weeks), twin, and mode of delivery (normal or cesarean section). A detailed clinical evaluation and laboratory investigations including full blood counts, blood films, blood glucose, renal function tests, serum electrolyte, and liver function tests were already performed. Some investigations like blood gas analysis, serum lactate, and serum ammonia were not available, and other further investigations were difficult to perform.
Exclusion criteria includes patients with normal development, neonates, and any cases without parental consent to be involved in this study and those who did not complete the screen.
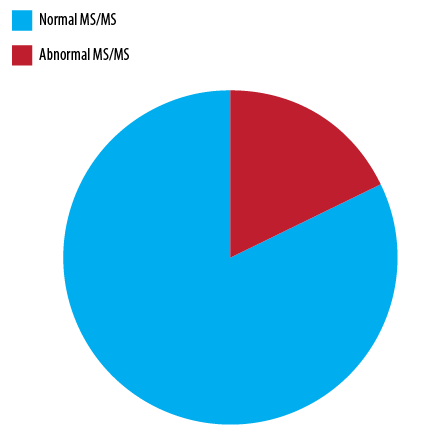
Figure 1: Classification of cases according to the results of tandem mass spectrometry (MS/MS).
The results of MS/MS were obtained in collaboration with MedLabs’ Referral Laboratory in Amman, Jordan. Blood sample collection was done via heel prick. The first drop of blood would be discarded then the next blood drops would be applied to the center of the circles of the filter paper, making sure that each drop would permeate through the back of the filter paper. All the four rings were filled. The filter papers were then shipped to MedLabs’ Referral Laboratory for performing MS/MS.
The review of the study protocol was done after obtaining ethical approval and permission from the Ministry of Higher Education, Misan College of Medicine, Misan Directorate of Health and Misan Hospital for Child and Maternity to conduct the study. Informed written consent was obtained from all parents.
The data analysis was carried out using SPSS Statistics (SPSS Inc. Released 2009. PASW Statistics for Windows, Version 18.0. Chicago: SPSS Inc.). The chi-square test was applied to meet the Cochran’s criteria to test the association between the different study variables (gender, family history, and CT scan of brain), while Fisher’s exact test was used for variables that did not meet Cochran’s criteria (consanguinity), and for the median age and range, the Mann-Whitney U test was used. Statistical significance (p-value) was calculated for each variable independently and considered significant when the value was equal to or less than 0.050.
Table 1 Types of inborn errors of metabolic disorders according to the results of tandem mass spectrometry.
|
Amino acid metabolism |
10 |
|
Phenylketonuria |
5 |
|
Maple syrup urine disease |
5 |
|
Organic acid metabolism |
5 |
|
Glutaric acidemia |
2 |
|
Propionic academia |
2 |
|
Others |
1 |
|
Fatty acid metabolism |
2 |
|
Carnitine uptake defect |
2 |
|
Other disorders |
3 |
|
Congenital adrenal hyperplasia |
1 |
|
Galactosemia |
1 |
|
Cystic fibrosis |
1 |
Results
Total cases were categorized into two groups according to the results of MS/MS; there were 20 cases with abnormal MS/MS, while the remaining cases had normal MS/MS [Figure 1].
The types of IEM were demonstrated according to the results of MS/MS:
- Half of abnormal MS/MS were amino acid metabolic disorders (10/20); five cases had phenyl-ketonuria and five had maple syrup urine disease.
- Disorders of organic acid metabolism were about 25% of the abnormal MS/MS in which glutaric acidemia and propionic academia were the most prevalent types.
- Disorders of fatty acid metabolism: two cases had a carnitine uptake defect.
- Finally, other disorders detected by MS/MS were congenital adrenal hyperplasia, galactosemia, and cystic fibrosis [Table 1].
In studying the association between disorders of IEM (abnormal MS/MS results) and some risk factors; the median age was 22 months while the gender association showed approximately the same number. Most cases of IEM had a positive history of consanguinity, as well as a family history. Statistically, only the family history showed a highly significant relationship with IEM (p < 0.001) while the other risk factors such as age, gender, and consanguinity had no significant association [Table 2].
Table 2: Relationship between some risk factors and the results of tandem mass spectrometry.
|
Age, median (range), months |
18 (2–72) |
22 (2–90) |
0.630* |
|
Gender |
|
|
0.500** |
|
Male |
57 |
11 |
|
|
Female |
35 |
9 |
|
|
Consanguinity |
|
|
|
|
Positive |
69 |
17 |
0.300*** |
|
Negative |
23 |
3 |
|
|
Family history |
|
|
|
|
Positive |
44 |
18 |
< 0.001** |
|
Negative |
48 |
2 |
|
|
Brain CT |
|
|
|
|
Abnormal |
44 |
8 |
0.500** |
*Mann-Whitney U test; **Chi-square test; ***Fisher’s exact test;
CT: computed tomography.
Discussion
Disorders of IEM are considered an important cause of morbidity and mortality in children. A delay in diagnosis as well as failure to treat these metabolic disorders in the appropriate time will lead to more damaging effects including mental retardation, neuropsychological abnormalities, poor outcome, and increased risk of death.13
We found a high rate of IEM disorders in children with unexplained developmental delay. A consanguineous marriage would cause greater expression of autosomal recessive disorders,14 and increased the prevalence of IEM disorders. The majority of IEM cases had positive consanguinity (17/20) and this can partially explain the high rate of IEM disorders in Misan despite the limited data on the consanguinity rate in Misan itself.
The effect of consanguinity was supported by different studies in Baghdad,15,16 Oman,17,18 the UAE,19 and Turkey.20
There are few studies of screening for IEM in patients with unexplained developmental delay. However, most of the studies emphasized that the screening for metabolic and genetic disorders of patients with unexplained developmental delay were needed as baseline investigations.21,22
Amino acid disorders followed by organic and fatty acid metabolism disorders were the most common in our study. A study from Baghdad revealed that the amino acid disorders were the most common type in newborn screening.15 In spite of the difference in the sample selection, amino acid disorders were still predominant in Iraq.
On the other hand, another study in Iran revealed that the incidence of organic academia was 42% and formed the first major type of IEM.23
These discrepancies in the sequence of IEM in comparison with other countries may be attributed to the differences among the population (race and ethnicity), the rate of consanguinity, screening criteria selection, and sample size.
Moreover, phenylketonuria and maple syrup urine diseases were the most frequent amino acid metabolic disorders with an equal detection rate for each. These results were higher than that of Baghdad for both.15
Males and females are affected equally because almost all types of IEM are inherited as autosomal recessive traits and this was in agreement with a previous study in which males were nearly equal to females (11:9).2
Our study showed a considerable number of IEM cases with abnormal findings in the brain CT scan at the time of diagnosis. Moreover, neuroimaging studies are of importance in the primary evaluation and diagnosis of IEM, estimating the severity of brain injury, and in providing baseline data to evaluate the efficacy of treatment.24
Furthermore, the family history in this study was of significant importance in the screening for IEM, which was consistent with other studies in Baghdad15,16 and Oman.17,18
The MS/MS is regarded as a single vital test using the same blood drop searching for different biochemical markers to screen for different IEM disorders.3,6 Meanwhile, this screening is not implemented in Misan in spite of having a high prevalence of IEM.
In Oman, it was reported that the MS/MS screening would be more feasible compared to the cost of caring for handicapped children.25
Before this study, IEM cases were not diagnosed in Misan, thus this study highlights this group of cases. Therefore, newborn screening programs such as MS/MS must be implemented in Misan, expanding the number of IEM disorders screened. We did not report or analyze the exact clinical presentation of the patients or any initial laboratory investigations, which is a limitation of this study. Further research, including these details, should be taken into consideration in the future. Additionally, there was a lack of facilities to perform MS/MS in our country, so these tests were directed to MedLabs’ Referral Laboratory in Amman, hence, no detailed information was obtained about their procedure.
Conclusion
A high rate of IEM were detected in children with unexplained developmental delay in Misan. A high clinical suspicion with a positive family history and consanguinity supported by MS/MS played an essential role in diagnosis. Implementation of newborn screening is essential for early diagnosis and to determine appropriate therapy in newborns with IEM in Iraq and in Misan in particular.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study. Abstract poster was presented in British Pediatric Neurology Association Annual Meeting in United Kingdom in January 2019.
references
- 1. Zhang C, Xu K, Dave UP, Wang Y, Matsumoto I. Inborn errors of metabolism discovered in Asian department of pediatrics and mental retardation research center. J Chromatogr B Biomed Sci Appl 2000 Sep;746(1):41-49.
- 2. Rezvani I, Rezvani GA. An approach to inborn errors of metabolism. In: Kliegman R, Stanton B, Geme JW, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. 20th ed. Philadelphia, Pennsylvania: Elsevier; 2016. p.634-636.
- 3. Chace DH, Kalas TA, Naylor EW. Use of tandem mass spectrometry for multianalyte screening of dried blood specimens from newborns. Clin Chem 2003 Nov;49(11):1797-1817.
- 4. Therrell BL Jr, Lloyd-Puryear MA, Camp KM, Mann MY. Inborn errors of metabolism identified via newborn screening: Ten-year incidence data and costs of nutritional interventions for research agenda planning. Mol Genet Metab 2014 Sep-Oct;113(1-2):14-26.
- 5. Bodamer OA, Hoffmann GF, Lindner M. Expanded newborn screening in Europe 2007. J Inherit Metab Dis 2007 Aug;30(4):439-444.
- 6. Wilcken B, Haas M, Joy P, Wiley V, Bowling F, Carpenter K, et al. Expanded newborn screening: outcome in screened and unscreened patients at age 6 years. Pediatrics 2009 Aug;124(2):e241-e248.
- 7. Waisbren SE, Albers S, Amato S, Ampola M, Brewster TG, Demmer L, et al. Effect of expanded newborn screening for biochemical genetic disorders on child outcomes and parental stress. JAMA 2003 Nov;290(19):2564-2572.
- 8. Ministry of Health and Environment. Iraq. Annual Statistical Report 2016, Directorate General of Planning, Department of Information and Statistics, 2017.
- 9. COSIT (Central Organization for Statistics and Information Technology). Iraq Living Conditions Survey 2004: Analytical Report Volume II. Baghdad: Ministry of Planning and Development Cooperation; 2005.
- 10. USAID; Primary Health Care Project. National guideline of newborn screening for care providers in PHC centers Iraq 2014. p.2-3. [cited June 2019]. Available from: https://studylib.net/doc/6617400/newborn-screening---primary-health-care-iraq.
- 11. Rao AN, Kavitha J, Koch M, Suresh Kumar V. Inborn errors of metabolism: review and data from a tertiary care center. Indian J Clin Biochem 2009 Jul;24(3):215-222.
- 12. Machado MC, Pinheiro da Silva F. Hyperammonemia due to urea cycle disorders: a potentially fatal condition in the intensive care setting. J Intensive Care 2014 Mar;2(1):22.
- 13. Raghuveer TS, Garg U, Graf WD. Inborn errors of metabolism in infancy and early childhood: an update. Am Fam Physician 2006 Jun;73(11):1981-1990.
- 14. Tadmouri GO, Nair P, Obeid T, Al Ali MT, Al Khaja N, Hamamy HA. Consanguinity and reproductive health among Arabs. Reprod Health 2009 Oct;6(1):17.
- 15. Arif HS, Thejeal RF, Farhan A. Inborn errors of metabolism status in Iraq. J Pharm Biol Sci. 2016;11(2):58-62.
- 16. Thijeel RF. The Prevalence of Phenylketonuria and other metabolic diseases in sick Iraqi children; the importance of the newborn screening program. J Fac Med. 2013;55(3):214-219.
- 17. Al Riyami S, Al Maney M, Joshi SN, Bayoumi R. Detection of inborn errors of metabolism using tandem mass spectrometry among high-risk Omani patients. Oman Med J 2012 Nov;27(6):482-485.
- 18. Joshi SN, Hashim J, Venugopalan P. Pattern of inborn errors of metabolism in an Omani population of the Arabian Peninsula. Ann Trop Paediatr 2002 Mar;22(1):93-96.
- 19. Al-Jasmi FA, Al-Shamsi A, Hertecant JL, Al-Hamad SM, Souid A-K. Inborn errors of metabolism in the United Arab Emirates: disorders detected by newborn screening (2011–2014). JIMD Reports 2016;28:127–135.
- 20. Tunçbilek E. Clinical outcomes of consanguineous marriages in Turkey. Turk J Pediatr 2001 Oct-Dec;43(4):277-279.
- 21. Silove N, Collins F, Ellaway C. Update on the investigation of children with delayed development. J Paediatr Child Health 2013 Jul;49(7):519-525.
- 22. O’Byrne JJ, Lynch SA, Treacy EP, King MD, Betts DR, Mayne PD, et al. Unexplained developmental delay/learning disability: guidelines for best practice protocol for first line assessment and genetic/metabolic/radiological investigations. Ir J Med Sci 2016 Feb;185(1):241-248.
- 23. Najafi R, Hashemipour M, Mostofizadeh N, Ghazavi M, Nasiri J, Shahsanai A, et al. Demographic and clinical findings in pediatric patients affected by organic acidemia. Iran J Child Neurol 2016;10(2):74-81.
- 24. Cakir B, Teksam M, Kosehan D, Akin K, Koktener A. Inborn errors of metabolism presenting in childhood. J Neuroimaging 2011 Apr;21(2):e117-e133.
- 25. Joshi SN, Bayoumi R. Newborn screening program for Oman: the time is here and now. Oman Med J 2012 Sep;27(5):346-347.