Congenital hypothyroidism (CHT) results from an absent or under-developed thyroid gland (dysgenesis), or the gland has developed but cannot produce enough thyroid hormone (dyshormonogenesis). Most neonates with CHT have a normal gross appearance on birth; however, a delay in the diagnosis of abnormalities threatens their neurodevelopmental function, especially in preterm and low-birth-weight infants.1-3
Different screening programs were established more than 40 years ago with the purpose of preventing intellectual disability arising from CHT. Screening programs for CHT were first established in North America in 1972, and this program is now performed routinely in most developed countries.4,5 Iranian screening programs for CHT were established in 19876 and were included in health care services in 2005. Thyroid-stimulating hormone (TSH) levels determined by filter-paper blood-spot is used preferably for CHT screening in Iran due to its high specificity.7,8
The best time to determine TSH levels is when the neonate is three to six days old, which can minimize the false positive of high TSH due to the physiological neonatal TSH rise.8 Although many centers have recommended repeated screening tests in premature newborns, there is no general agreement on the time of its measurement.
The reported incidence rate of both CHT and preterm infants has increased significantly during the past two decades.9 In this study, we evaluated the prevalence of CHT among preterm infants by studying the results of thyroid screening tests in different parts of Fars province, Iran, from 2014 to 2017. Our study sought to determine the incidence of abnormal TSH at three to six days old and in weeks two, six, 10, and 12 to evaluate the validity of repeating the test.
Methods
This retrospective cross-sectional study recorded all live births in Fars province, Iran, from March 2014 to October 2017. Neonates with a gestational age
< 37 weeks were considered premature and included in this study. Any neonates with major congenital anomalies were excluded from the study. This study was approved by the Ethics Committee of Shiraz University of Medical Sciences (IR.SUMS.REC.1397.138).
All data, including TSH measurements, were collected from the central newborn screening center of the Shiraz University of Medical Science. TSH was measured from dried blood spots from the newborns’ heel on filter paper using commercial enzyme-linked immunosorbent assay (ELISA) kits (NEO-TSH, Pishtaz Teb Zaman Diagnostics) according to the manufacturer’s instructions. TSH levels were first measured between three and six days of birth; however, the premature newborns were rescreened in weeks two, six, 10, and 12 after birth. The cut-off for a positive test was ≥ 10.0 mU/L in the first seven days of life and ≥ 5.0 mU/ L after seven days in premature infants.10 We also recorded sex and birth date data. If the results were abnormal, the newborns were referred to an endocrinologist, but we had no information about the follow-up.
The data were analyzed using SPSS Statistics (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp.), and a p-value ≤ 0.050 was considered statistically significant. Chi-square test was used to evaluate the qualitative variables, and McNemar’s test was used for comparing the results of different levels of TSH in several times.
Results
From March 2014 to October 2017, 320 886 (48.0% girls and 52.0% boys) live births were screened in Fars province. The number of premature newborns was 15 381(4.8%); one neonate with Down syndrome was excluded from the study. Three-hundred and fifty-five premature newborns had an abnormal TSH screening test (TSH > 10.0 mU/L in the first week and TSH > 5.0 mU/L after the first week of life) during the 12 weeks follow-up giving a CHT prevalence of 2.3%. There were 195 (54.9%) boys and 160 (45.1%) girls with CHT, and no significant difference was found between boys and girls with prematurity (p = 0.050). TSH ranged from 0.1 mU/L to 285.4 mU/L (mean = 6.6±22.4 mU/L) in 355 premature newborns with CHT.
The number of newborns with high TSH levels recorded at three to six days old was 111 giving a 31.3% prevalence of CHT at first screening. Among the remaining 244 premature newborns with CHT; 156 (43.9%) had increased TSH levels in week two, 51 (14.4%) in week six, 35 (9.9%) in week 10, and two (0.6%) newborns in week 12 [Figure 1].
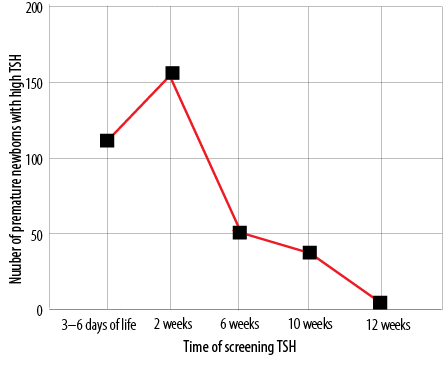
Figure 1: Number of premature newborns with high Thyroid-stimulating hormone (TSH) measure in the first three to six days of life and in weeks two, six, 10, and 12.
McNemar’s test showed that the results of the first screening (days three to six) were significantly different with the results of the second test in the second week of life (p < 0.001) and with the third test in the sixth week (p < 0.001). Current data revealed that 63.9% (156/244) of the premature neonates who had the first negative test had positive second test results.
Among 88 premature newborns with normal TSH at the first screening and in the second week, 51 (58.0%) newborns showed high TSH in the sixth week (p < 0.001) post-birth.
Discussion
We found a 2.3% prevalence rate of hypothyroidism in 15 381 premature newborns born in Fars province, Iran, from 2014 to 2017. The rate of CHT was reported as 0.1% in all live births in this area in 2006–2007.11 Many studies found that CHT was more common in premature newborns. This high rate of CHT in premature newborns is explained by immaturity in the hypothalamic-pituitary-thyroid axis, a low thyroidal capacity to synthesize iodine, and immature thyroid hormone metabolism; however, premature newborns also need more thyroid hormone for thermogenesis.12
A Korean study found 12.2% (30/246) of very low birth newborns (< 1500 g) exhibited CHT.13 Another study from the USA revealed 9.1% of 280 premature infants < 30 weeks gestation had thyroid dysfunction.14 European studies showed ranges from 5% to 18% of preterm infants with hypothyroidism.15,16 Our study considered only screening data; therefore, we did not have the weight and exact gestational age data for the newborns.
According to our data, the first screening test revealed one-third of premature newborns had CHT. A recent review indicated that many studies emphasized repetition of TSH for proper CHT screening in preterm infants; however, the proper time for retesting is disputed.17 The number of premature newborns with CHT in our study detected by the second and sixth weeks TSH retesting was 43.9% and 14.4%, respectively, which was significantly increased compared with our first sampling. We recommend repeating TSH testing in the second week of life similar to previous studies15,17 and six weeks after birth. Delaying the second and third screening test, and therefore the diagnosis of CHT can threaten the intellectual ability in preterm newborns. Our data found 10.4% of preterm infants (37/355) showed a rise of TSH after the sixth week of life; however, commencing appropriate initial therapy can reduce the pathological consequences of CHT.
Endocrinologists and pediatricians recommended measuring both TSH and free thyroxine for CHT screening in preterm neonates.18 Therefore, it is advised that primary screening tests and following the tests with both TSH and free thyroxine could diagnose CHT with delayed TSH elevation.
All premature patients were recruited from a screening referral center in Fars province and may not represent premature newborns in other major cities of Iran. Another limitation of our study was a lack of data on the exact gestational age and birth weight of our study cohort.
Conclusion
Our report described the prevalence of CHT in premature newborns based on measuring TSH in a large cohort of newborns in Fars province, Iran. The thyroid screening program of preterm infants needs a second (week two), third (week six), and fourth (week 10) screening test for CHT and is essential in detecting newborns who would not otherwise
be identified.
Disclosure
The authors declared no conflicts of interest. The present article was extracted from the thesis written by Dr. Pegah Hasanshahi and was financially supported by Shiraz University of Medical Science grant number 16086-47-01-1396.
Acknowledgements
The authors would like to thank the Center for Development of Clinical Research of Nemazee Hospital, Dr. Nasrin Shokrpour for editorial assistance, and Dr. Ahmadpoor and Dr. Modaressi for statistical analysis.
references
- 1. Wassner AJ, Brown RS. Congenital hypothyroidism: recent advances. Curr Opin Endocrinol Diabetes Obes 2015 Oct;22(5):407-412.
- 2. Hemmati F, Pishva N. Evaluation of thyroid status of infants in the intensive care setting. Singapore Med J 2009 Sep;50(9):875-878.
- 3. Razavi Z, Yavarikia A, Torabian S. Congenital anomalies in infant with congenital hypothyroidism. Oman Med J 2012 Sep;27(5):364-367.
- 4. Fisher DA, Dussault JH, Foley TP Jr, Klein AH, LaFranchi S, Larsen PR, et al. Screening for congenital hypothyroidism: results of screening one million North American infants. J Pediatr 1979 May;94(5):700-705.
- 5. Desai MP, Sharma R, Riaz I, Sudhanshu S, Parikh R, Bhatia V. Newborn screening guidelines for congenital hypothyroidism in India: recommendations of the Indian society for pediatric and adolescent endocrinology (ISPAE) - Part I: Screening and confirmation of diagnosis. Indian J Pediatr 2018 Jun;85(6):440-447.
- 6. Azizi F, Oladi B, Nafarabadi M, Hajipoor R. Screening for congenital hypothyroidism in Tehran. Effect of iodine deficiency on transient elevation of neonatal TSH. J Shaheed Beheshti School Med. 1994;18(1):34-38.
- 7. Bourdoux PP, Van Thi HV, Courtois PA, Ermans AM. Superiority of thyrotropin to thyroxine as a tool in the screening for congenital hypothyroidism by the filter paper spot technique. Clin Chim Acta 1991: 15;195(3):97-105.
- 8. Büyükgebiz A. Newborn screening for congenital hypothyroidism. J Clin Res Pediatr Endocrinol 2013;5 Suppl 1(Suppl 1):8-12.
- 9. Hinton CF, Harris KB, Borgfeld L, Drummond-Borg M, Eaton R, Lorey F, et al. Trends in incidence rates of congenital hypothyroidism related to select demographic factors: data from the United States, California, Massachusetts, New York, and Texas. Pediatrics 2010 May;125(Suppl 2):S37-S47.
- 10. Korzeniewski SJ, Kleyn M, Young WI, Chaiworapongsa T, Schwartz AG, Romero R. Screening for congenital hypothyroidism in newborns transferred to neonatal intensive care. Arch Dis Child Fetal Neonatal Ed 2013 Jul;98(4):F310-F315.
- 11. Karamizadeh Z, Saneifard H, Amirhakimi G, Karamifar H, Alavi M. Evaluation of congenital hypothyroidism in fars province, iran. Iran J Pediatr 2012 Mar;22(1):107-112.
- 12. Murphy N, Hume R, van Toor H, Matthews TG, Ogston SA, Wu SY, et al. The hypothalamic-pituitary-thyroid axis in preterm infants; changes in the first 24 hours of postnatal life. J Clin Endocrinol Metab 2004 Jun;89(6):2824-2831.
- 13. Lee JH, Kim SW, Jeon GW, Sin JB. Thyroid dysfunction in very low birth weight preterm infants. Korean J Pediatr 2015 Jun;58(6):224-229.
- 14. Kaluarachchi DC, Colaizy TT, Pesce LM, Tansey M, Klein JM. Congenital hypothyroidism with delayed thyroid-stimulating hormone elevation in premature infants born at less than 30 weeks gestation. J Perinatol 2017 Mar;37(3):277-282.
- 15. Rooman RP, Du Caju MV, De Beeck LO, Docx M, Van Reempts P, Van Acker KJ. Low thyroxinaemia occurs in the majority of very preterm newborns. Eur J Pediatr 1996 Mar;155(3):211-215.
- Delange F, Dalhem A, Bourdoux P, Lagasse R, Glinoer D, Fisher DA, Walfish PG, Ermans AM. Increased risk of primary hypothyroidism in preterm infants. J Pediatr. 1984 Sep;105(3):462-469.
- 16. Chung HR, Shin CH, Yang SW, Choi CW, Kim BI, Kim EK, et al. High incidence of thyroid dysfunction in preterm infants. J Korean Med Sci 2009 Aug;24(4):627-631.
- 17. Hashemipour M, Hovsepian S, Ansari A, Keikha M, Khalighinejad P, Niknam N. Screening of congenital hypothyroidism in preterm, low birth weight and very low birth weight neonates: A systematic review. Pediatr Neonatol 2018 Feb;59(1):3-14.