According to the International Labour Organization, ‘going to work is more dangerous than war.’1 Although the detrimental effects of working have only been definitely linked to certain professions, there is increasing evidence suggesting that physicians often have high levels of stress and are at high risk of developing occupational burnout.2 Burnout among physicians is known to have negative repercussions on their wellbeing, as well their abilities as working physicians. In addition to an increased risk of medical error, physicians suffering from burnout tend to have lower levels of productivity, utilize more sick leave, and resort to early retirement.3,4 Overall, enormous revenue is lost due to stress-induced poor decision making, stress-related mental illness, and substance abuse among physicians.5,6 The consequences following burnout among physicians appears to be catastrophic when compared to the prevalence of burnout among the general population.7
The Maslach Burnout Inventory (MBI) has been used extensively to identify the prevalence and determinants of occupational burnout among primary care physicians (PCPs) globally. The MBI is known as an introspective psychological inventory,’ designed to uncover the presence of occupational burnout. Burnout is a psychological syndrome, characterized by a symptomatic triad: emotional exhaustion (EE), including feelings of tiredness and emptiness; depersonalization (DP), such as a lack of empathy, increased levels of cynicism and automatism; and a lack of personal accomplishment (PA), including a lack of self-esteem and increased levels of frustration.8 Among training PCPs in France, high levels of EE was noted (16%), along with a high score for DP (34%), and low PA (40%).9 The factors associated with burnout include an imbalance in effort and reward, working in accident-prone environments, and work-life imbalance. One study sought to determine the magnitude of burnout and its determinants among PCPs in 12 European countries.10 Using the MBI, it was found that 43% of respondents had high levels of EE, 35% showed DP, and 12% lacked PA. This study suggested a strong correlation between burnout and absenteeism and a tendency to self-medicate. Gender and age were also found to be significant factors. A study from the US used the MBI to explore the link between clinic capacity and burnout.11 The results suggested that burnout rates strongly influenced the variation in clinical capacity.
The prevalence of burnout has also risen in transitional societies, where PCPs meet the bulk of the population’s healthcare needs.12,13 The MBI was utilized to determine the rate of occupational burnout among PCPs in Cameroon.14 This study found that although the majority of the sample was not aware of the concept of burnout, approximately 42% displayed burnout symptoms. Burnout was associated with specific sociodemographic factors.
Studies have also been carried out in Middle Eastern countries. In Turkey, there was a high prevalence of occupational burnout among PCPs, with sociodemographic factors such as gender and marital status noted to be strongly related to the EE and DP subscale of the MBI.15 In Israel, there was a direct relationship between increased workloads and levels of burnout symptoms.16 A study from Egypt used the MBI to compare the rate of occupational burnout between hospital physicians and PCPs.17 This study suggested that hospital physicians had higher levels of burnout syndrome symptoms compared to PCPs. In Iran, approximately 15% of the PCPs showed high levels of EE, DP, and a lack of interest in PA.18 The high levels of occupational burnout were strongly associated with certain temperaments. In contrast to previous studies, low levels of EE and DP and high levels of interest in PA were reported among PCPs in Australia.19 This implies that there is high variability in the occupational burnout rate among different populations, and suggests that ecological and personal factors play a substantial role in the expression and correlation of occupational burnout.
As stated above, some studies have suggested that occupational burnout is more common among PCPs in certain parts of the world. Some studies have also suggested that there are various predictors of occupational burnout among PCPs. There is currently a dearth of burnout studies among PCPs in Arabian Gulf countries.20 To the best of our knowledge, this is the first study to assess the rates of burnout among PCPs in Oman. We sought to assess the risk factors for developing burnout among PCPs in Oman.
Methods
We conducted a cross-sectional study among a random cluster sample of PCPs working in Muscat, Oman, between March and May 2017. In Oman, healthcare is free for its citizens, and primary healthcare is the basic first portal of entry to all levels of health care.21 Primary health care centers are meant to provide both preventive and curative primary care services to all acute and chronic somatic and mental health illnesses.22
Based on a previous study in Arabic populations looking at the prevalence of occupational burnout among PCPs, the total number of PCPs in Oman, a 95% confidence interval (CI), a type 1 error probability of 5%, and a power of 80%, we calculated a required sample size of 197.20,21 The EpiInfo™ software (Epi Info™, Division of Health Informatics & Surveillance, enter for Surveillance, Epidemiology & Laboratory Services, 1600 Clifton Road Atlanta, GA 30329-4027 USA) was used to calculate the sample size.
A two-stage sampling process was employed to select the participants. First, Muscat was the randomly selected governorate out of ten potential governorate in Oman. Second, within Muscat, a simple computer-aided list of a random sample of currently working PCPs was generated.
The investigators of this study approached the randomly selected participants at their workplace after arranging appointments with them. The purpose of the study, confidentiality, and anonymity were explained to the participants. Then, informed consent forms and the study questionnaire were handed over to the participants to complete in a private room. After 20 minutes, the investigators collected the questionnaire along with the signed consent forms.
Participant burnout was evaluated using the MBI-Human Services Survey (HSS).23 It is a self-administered tool designed to capture three facets of burnout syndrome: EE, DP, and reduced PA. The questionnaire has 22 items, divided into the three categories. Each item is accompanied by a seven-point Likert scale, in terms of the frequency with which the participant experiences the feelings related to burnout (from 0 = never to 6 = everyday). The nine-item EE subscale (statements 1–9) evaluate feelings of being emotionally exhausted by one’s job. The DP subscale (statements 10–14) assesses how detached the participants feel when they are delivering treatment, care, or instructions. The PA subscale reflects how the participant feels regarding their success at work and their level of competence. Higher mean scores in EE and DP and lower mean score on PA indicates a high level of burnout. In the existing literature, the following cut-off means scores were used to differentiate those with burnout and those without: EE ≥ 26, DP ≥ 9, PA ≤ 33.
The reliability and validity of MBI-HSS in the present study sample were also noted. The internal consistency reliabilities of the three subscales were as follows; Cronbach’s α was 0.75 for EE, 0.80 for DP, and 0.78 for PA. Confirmatory factor analysis was performed to examine the construct validity of MBI-HSS in the current study. The analysis found the three factors (EE, DP, and PA) had an Eigenvalue > 1 and accounted for 70.5% of the total variance. The items loaded well in each subscale or factor.
We also used a questionnaire to obtain demographic and job data, including gender, marital status, average number of working hours per week, number of patients attended to per day, and whether they have previously felt the need to seek professional help due to stress at work.
We used SPSS Statistics (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.) for data analysis. Sociodemographic factors were described using descriptive analysis. The prevalence rate of burnout syndrome was calculated by dividing the total number of cases by the total number of study participants. We used the chi-square test to compare the statistical difference of the proportions of burnout syndrome among the independent variables, and a p-value of < 0.050 was deemed to be statistically significant. For confirmatory factor analysis of the data in the study, a goodness-of-fit index with a cut-off score of > 0.9 was set to decrease the chance of type one error. The Varimax rotation approach was then performed. Factor loading was no more than 0.30 for the item to be considered belonging to a certain factor. Suitability of the data for factor analysis was assessed by Bartlett’s test and the Kaiser-Meyer-Olkin index.24
We used a stepwise backward binary logistic regression analysis for the significant factors at univariate analysis (chi-square test) to decipher the predictors of burnout syndrome. Covariates were incorporated into the model according to their potential link to the other independent variables and the trend of being associated with burnout syndrome in univariate analysis (p = 0.250). The unadjusted and adjusted odds ratios (OR) were depicted in univariate and multivariate analysis with a 95% CI. We used the Cox and Snell approach25 to judge the goodness-of-fit of the logistic regression model.
This study was conducted according to the Declaration of Helsinki ensuring confidentiality, autonomy, correct data management, as well as ensuring informed consent was obtained.26 This study was granted ethical approval by the Ministry of Health, Oman (MH/DGPS/MG154).
Results
Table 1 presents the sociodemographic characteristics of the PCPs in this study (n = 190). Approximately 50% of PCPs were aged 30–39 years old. The majority were female (78.4%) and married (87.4%). Most PCPs (n = 112, 58.6%) were not trained as family physicians or general practitioners. Eighty-seven PCPs stated that they were under financial strain. More than half of the participants (57.4%) admitted that they had contemplated seeking professional psychological help. The response rate was 96%.
Table 1: Characteristics of the sample (n = 190) of primary care physicians in Muscat governorate.
|
Sex |
|
|
Male |
41 (21.6) |
|
Female |
149 (78.4) |
|
Age, years |
|
|
18–29 |
36 (18.9) |
|
30–39 |
95 (50.0) |
|
40–49 |
48 (25.3) |
|
≥ 50 |
11 (6.3) |
|
Marital status |
|
|
Married |
166 (87.4) |
|
Single |
19 (10.0) |
|
Divorced |
4 (2.1) |
|
Widowed |
1 (0.5) |
|
Average working hours per week |
|
|
0–20 |
9 (4.7) |
|
21–40 |
115 (60.2) |
|
41–80 |
62 (33.0) |
|
> 80 |
4 (2.1) |
|
Patients seen per day, n |
|
|
0–10 |
8 (4.2) |
|
11–20 |
4 (20.1) |
|
21–30 |
55 (28.9) |
|
31–50 |
84 (44.2) |
|
> 50 |
4 (2.1) |
|
Felt like they need professional psychological help |
|
Yes |
109 (57.4) |
Table 2: Binary logistic regression models for predicting burnout syndrome (high EE and DP, and low PA) from the sociodemographic variables.
|
Sex |
|
|
|
|
|
|
|
|
|
Male |
2 (4.9) |
0.718 |
0.151–3.414 |
1.000 |
0.441 |
6.085 |
0.032 |
0.541 |
|
Female (Ref.) |
10 (6.7) |
|
|
|
|
|
|
|
Age |
|
|
|
|
|
|
|
|
18–29 (Ref.) |
2 (5.6) |
1.352 |
0.267–6.837 |
0.923 |
|
|
|
0.809 |
|
30–39 |
7 (1.1) |
0.739 |
0.099–5.513 |
|
1.534 |
16.142 |
0.146 |
0.721 |
|
40–49 |
2 (4.2) |
1.545 |
0.128–18.731 |
|
2.604 |
42.716 |
0.159 |
0.503 |
|
> 50 |
1 (8.3) |
|
|
|
5.142 |
240.098 |
0.110 |
0.404 |
|
Marital status |
|
|
|
|
|
|
|
|
|
Married (Ref.) |
10 (6.2) |
1.835 |
0.371–9.077 |
0.763 |
|
|
|
0.735 |
|
Single |
2 (10.5) |
|
|
|
4.531 |
62.408 |
0.329 |
0.259 |
|
Divorced |
0 (0.0) |
|
|
|
0.000 |
. |
0.000 |
0.999 |
|
Widowed |
0 (0.0) |
|
|
|
0.000 |
. |
0.000 |
1.000 |
|
Average working hours per week |
|
0–20 |
2 (22.2) |
0.094 |
|
0.039* |
|
|
|
|
|
21–40 |
3 (2.6) |
0.438 |
0.013–0.656 |
|
0.025 |
0.845 |
0.001 |
0.040 |
|
41–80 (Ref.) |
7 (11.1) |
|
0.075–2.535 |
|
0.049 |
1.426 |
0.002 |
0.080 |
|
Number of patients seen per day |
|
0–10 (Ref.) |
1 (12.5) |
0.179 |
|
0.813 |
|
|
|
0.989 |
|
11–20 |
1 (2.5) |
0.549 |
0.010–3.217 |
|
0.000 |
71.536 |
0.000 |
0.997 |
|
21–30 |
4 (7.3) |
0.538 |
0.053–5.639 |
|
1.160 |
28.649 |
0.019 |
0.944 |
|
31–50 |
6 (7.1) |
|
0.057–5.128 |
|
0.694 |
- |
0.017 |
0.848 |
|
> 50 |
0 (0.0) |
|
|
|
0.000 |
71.536 |
0.000 |
0.999 |
|
Felt like they need professional psychological help |
|
Yes |
10 (9.3) |
8.144 |
1.021–64.994 |
0.025* |
59.573 |
5334.578 |
0.665 |
0.075 |
Ref: Value used as the denominator in the calculation of odds ratios; OR: odds ratio; CI: confidence interval.
*p-value of < 0.050 was considered statistically significant.
The overall prevalence of burnout was 6.3% [Figure 1]. High levels of EE were reported by 17.8% of participants, while 38.2% experienced high levels of DP and 21.5% had low levels of PA.
Table 2 shows the univariate (unadjusted) and multivariable (adjusted) analysis results. Working hours was the only statistically significant factor in predicting burnout syndrome (high EE and DP, and low PA) in the multivariate analysis (p < 0.050). Participants who worked 40–80 hours per week had the higher risk of burnout syndrome compared to participants working ≤ 20 hours per week (OR = 0.025; 95% CI: 0.845–0.001; p = 0.040).
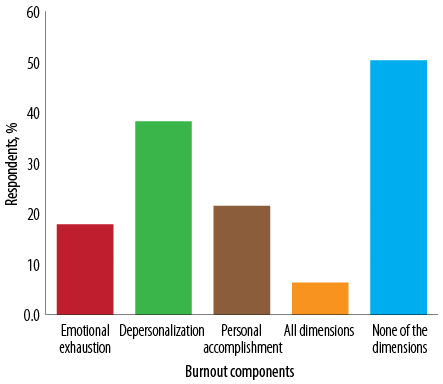
Figure 1: Prevalence of burnout as defined by the Maslach Burnout Inventory among primary care physicians in Oman.
Discussion
Various studies have explored the prevalence of occupational burnout among PCPs and trainees using the MBI, which has been specifically designed to solicit the presence of three symptoms of occupational burnout (EE, DP, and PA). In the USA, the incidence of EE has been reported to vary from 19.5% to 34.4%, DP to vary from 6.0% to 26.9%, and PA to vary from 28.2% to 38.68%.4,27,28 It has been reported that among PCPs in 12 European countries, 43%, 35%, and 32% of the participants displayed EE, DP, and PA, respectively.10 In our study, the figures were 17.8%, 38.2%, and 21.5% for EE, DA, and PA. In general, the figures fall within the international trend. These figures from PCPs in Oman also appear to be displaying the same trends as other transition societies, such as Turkey, Israel, Egypt, Iran, and Saudi Arabia.15–18,20 In most of these studies from industrialized countries as well as those from transition societies have focused on medical students. Our study, in agreement with others, found that medical professionals, irrespective of their level of training or status, are marked with indices of occupational burnout.
In addition to examining the prevalence, there is a vast amount research in the current literature regarding the factors associated with burnout among PCPs, including inadequate staff, excessive workload, financial strain, inadequate supervision, night work, witnessing death in practice, frequent conflicts among healthcare professionals, stressors in their private life, and a lack of social support.29–32 Due to these factors, PCPs tend to exhibit high rates of turnover and have a high risk of depressive disorders, poor job performance, and high rates of absenteeism.12,33–35 The multivariate analysis of this study indicate a significant relationship between the average number of working hours per week, the need for professional psychological help, and the indices of burnout. Understanding the factors associated with burnout among physicians could lay the groundwork for evidence-based interventions. Indeed, some initiatives to prevent burnout and other interventions can currently be found in the literature. A systematic review of 19 studies and a meta-analysis on the effectiveness of interventions to reduce burnout in physicians, which included 1550 physicians, concluded that the existing interventions do not help to mitigate burnout among physicians. 2 Therefore, the present burnout crisis would require institutional changes rather than relying on existing token measures of providing stress-management for physicians suffering from burnout.
Being a cross-sectional study, we cannot eliminate causal association. This study also relied on a self-reported questionnaire, which are often marred by factors such as recall bias and social desirability. Another limitation is that approximately 59% of the study samples were not trained as family physicians or general practitioners. In Oman, primary health care services are predominantly attended by non-specialized physicians as this study suggests. Therefore, the generalization of our results should be taken with this caveat. Finally, the bulk of the population in Oman live in Muscat, where this study was conducted. However, primary health care centers are spread in all corners of the country.36 This implies that the generalization of this study will be limited to PCPs working in urban areas. Previous studies have indicated that the urban-rural dichotomy tends to play a part in the development of occupational burnout.37,38
Conclusions
We sought to examine the prevalence and correlates of burnout among PCPs working in urban areas of Oman. The second, related, aim was to explore the antecedent factors associated with their burnout. Using the MBI, the prevalence of burnout was 6.3% among the participants in this study with long working hours strongly associated with high occupational burnout. Although we found a lower prevalence rate compared to the international trend, our results indicate that burnout among PCPs should be of serious concern. Therefore, more studies are needed so that an evidence-based intervention can be devised.
Disclosure
The authors declare no conflicts of interest. No funding was received for this study.
Acknowledgements
We would like to thank all the residents who participated in the study.
references
- 1. International Labour Organization. World day for safety and health at work 2013. [cited June 2018]. Available from: www.ilo.org/safework/events/safeday/WCMS_204594/lang--en/index.htm.
- 2. Panagioti M, Panagopoulou E, Bower P, Lewith G, Kontopantelis E, Chew-Graham C, et al. Controlled interventions to reduce burnout in physicians: asystematic review and meta-analysis. JAMA Intern Med 2017 Feb;177(2):195-205.
- 3. Kang EK, Lihm HS, Kong EH. Association of intern and resident burnout with self-reported medical errors. Korean J Fam Med 2013 Jan;34(1):36-42.
- 4. Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med 2002 Mar;136(5):358-367.
- 5. Hughes PH, Brandenburg N, Baldwin DC Jr, Storr CL, Williams KM, Anthony JC, et al. Prevalence of substance use among US physicians. JAMA 1992 May;267(17):2333-2339.
- 6. Baharvand P, Hormozi M, Anbari K. Mental health and related factors in physicians working in hospitals: a study in Western Iran in 2016. Middle East JFam Med 2018 Apr;16(4):85.
- 7. Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med 2012 Oct;172(18):1377-1385.
- 8. Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual. 4th Edition. 1996–2016. Menlo Park, CA: Mind Garden, Inc.
- 9. Galam E, Komly V, Le Tourneur A, Jund J. Burnout among French GPs in training: a cross-sectional study. Br J Gen Pract 2013 Mar;63(608):e217-e224.
- 10. Soler JK, Yaman H, Esteva M, Dobbs F, Asenova RS, Katic M, et al; European General Practice Research Network Burnout Study Group. Burnout in European family doctors: the EGPRN study. Fam Pract 2008 Aug;25(4):245-265.
- 11. Olayiwola JN, Willard-Grace R, Dubé K, Hessler D, Shunk R, Grumbach K, et al. Higher perceived clinic capacity to address patients’ social needs associated with lower burnout in primary care providers. J Health Care Poor Underserved 2018;29(1):415-429.
- 12. Chaudhury N, Hammer J, Kremer M, Muralidharan K, Rogers FH. Missing in action: teacher and health worker absence in developing countries. J Econ Perspect 2006;20(1):91-116.
- 13. Rule J, Ngo DA, Oanh TT, Asante A, Doyle J, Roberts G, et al. Strengthening primary health care in low- and middle-income countries: generating evidence through evaluation. Asia Pac J Public Health 2014 Jul;26(4):339-348.
- 14. Mandengue SH, Owona Manga LJ, Lobè-Tanga MY, Assomo-Ndemba PB, Nsongan-Bahebege S, Bika-Lélé C, et al. [Burnout syndrome among generalist medical doctors of Douala region (Cameroon): Can physical activities be a protective factor?]. Rev Med Brux 2017;38(1):10-15.
- 15. Karakose T. An evaluation of the relationship between general practitioners’ job satisfaction and burnout levels. Stud Ethno-Med 2014;8(3):239-244.
- 16. Kushnir T, Greenberg D, Madjar N, Hadari I, Yermiahu Y, Bachner YG. Is burnout associated with referral rates among primary care physicians in community clinics? Fam Pract 2014 Feb;31(1):44-50.
- 17. Kotb AA, Mohamed KA, Kamel MH, Ismail MA, Abdulmajeed AA. Comparison of burnout pattern between hospital physicians and family physicians working in Suez Canal University Hospitals. Pan Afr Med J 2014 Jun;18:164.
- 18. Ahmadpanah M, Torabian S, Dastore K, Jahangard L, Haghighi M. Association of occupational burnout and type of personality in Iranian general practitioners. Work 2015 Jun;51(2):315-319.
- 19. Ifediora CO. Burnout among after-hours home visit doctors in Australia. BMC Fam Pract 2016 Jan;17(1):2.
- 20. Al-Sareai NS, Al-Khaldi YM, Mostafa OA, Abdel-Fattah MM. Magnitude and risk factors for burnout among primary health care physicians in Asir Province, Saudi Arabia. East Mediterr Health J 2013 May;19(5):426-434.
- 21. Oman Information Centre. Primary Health Care in Sultanate of Oman. [cited June 2018]. Available from: www.omaninfo.com/health/primary-health-care-sultanate-oman.asp.
- 22. Al-Salmani A, Juma T, Al-Noobi A, Al-Farsi Y, Jaafar N, Al-Mamari K, et al. Characterization of depression among patients at urban primary healthcare centers in Oman. Int J Psychiatry Med 2015;49(1):1-18.
- 23. Al-Alawi M, Al-Sinawi H, Al-Qubtan A, Al-Lawati J, Al-Habsi A, Al-Shuraiqi M, et al. Prevalence and determinants of burnout Syndrome and Depression among medical students at Sultan Qaboos University: A cross-sectional analytical study from Oman. Arch Environ Occup Health 2017 Nov;(Nov):1-10.
- 24. Dziuban CD, Shirkey EC. When is a correlation matrix appropriate for factor analysis? Some decision rules. Psychol Bull 1974 Jun;81(6):358.
- 25. Cox DR, Snell EJ. The choice of variables in observational studies. J R Stat Soc Ser C Appl Stat 1974 Jan;23(1):51-59.
- 26. World Medical Association General Assembly. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. J Int Bioethique 2004 Mar;15(1):124-129.
- 27. Michels PJ, Probst JC, Godenick MT, Palesch Y. Anxiety and anger among family practice residents: a South Carolina family practice research consortium study. Acad Med 2003 Jan;78(1):69-79.
- 28. Dyrbye LN, Thomas MR, Huntington JL, Lawson KL, Novotny PJ, Sloan JA, et al. Personal life events and medical student burnout: a multicenter study. Acad Med 2006 Apr;81(4):374-384.
- 29. Parola V, Coelho A, Cardoso D, Sandgren A, Apóstolo J. Prevalence of burnout in health professionals working in palliative care: a systematic review. JBI Database System Rev Implement Rep 2017 Jul;15(7):1905-1933.
- 30. Trufelli DC, Bensi CG, Garcia JB, Narahara JL, Abrão MN, Diniz RW, et al. Burnout in cancer professionals: a systematic review and meta-analysis. Eur J Cancer Care (Engl) 2008 Nov;17(6):524-531.
- 31. Medisauskaite A, Kamau C. Prevalence of oncologists in distress: Systematic review and meta-analysis. Psychooncology 2017 Nov;26(11):1732-1740.
- 32. Roberts DL, Cannon KJ, Wellik KE, Wu Q, Budavari AI. Burnout in inpatient-based versus outpatient-based physicians: a systematic review and meta-analysis. J Hosp Med 2013 Nov;8(11):653-664.
- 33. Mata DA, Ramos MA, Bansal N, Khan R, Guille C, Di Angelantonio E, et al. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA 2015 Dec;314(22):2373-2383.
- 34. Linzer M, Manwell LB, Williams ES, Bobula JA, Brown RL, Varkey AB, et al; MEMO (Minimizing Error, Maximizing Outcome) Investigators. Working conditions in primary care: physician reactions and care quality. Ann Intern Med 2009 Jul;151(1):28-36, W6-W9.
- 35. Panagioti M, Geraghty K, Johnson J, Zhou A, Panagopoulou E, Chew-Graham C, et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction: asystematic review and meta-analysis. JAMA Intern Med 2018 Oct;178(10):1317-1330.
- 36. Al-Mandhari A, Alsiyabi H, Al Rabhi S, Al-Adawi SS, Al-Adawi S. Oman: Paradigm change: healthy villages to meet tomorrow’s health needs. In: Braithwaite J,
Mannion R, Matsuyama Y, Shekelle PG, Whittaker S, Al-Adawi S (Eds). Healthcare systems: future predictions for global care. Florida, CRC Press Taylor & Francis Group, 2018. p. 319-325.
- 37. Koike S, Matsumoto M, Kawaguchi H, Ide H, Atarashi H, Kotani K, et al. Board certification and urban-rural migration of physicians in Japan. BMC Health Serv Res 2018 Aug;18(1):615.
- 38. Lo D, Wu F, Chan M, Chu R, Li D. A systematic review of burnout among doctors in China: a cultural perspective. Asia Pac Fam Med 2018 Feb;17:3.