Teaching is a vocally demanding profession that often results in dysphonia1 and vocal fatigue.2 Dysphonia leads to adverse vocal symptoms such as hoarseness, weakness, sore throat, and aphonia.3 The most common organic pathology identified in this occupational group is vocal fold nodules, which are commonly associated with vocal abuse.4,5
The prevalence of current dysphonia among teachers ranges between 8.7%6 and 36.6%.7 A study among primary school teachers in Malaysia indicated that 53.8% suffered from dysphonia in the past 12 months.8 In addition, another local study documented a 10.4% prevalence of voice disorders among Malaysian secondary school teachers.9
While most teachers appear high functioning, the consequences of voice disorders can be significant. This includes laryngeal injury, limitation to job satisfaction, impaired performance and attendance, and a reduction in social, psychological, emotional, physical, and communicative functioning.10
Voice-related absenteeism was observed in 19.2% of teachers in one study.11 Unfortunately, students are often at the receiving end of this backlash, as low teacher attendance is correlated with low student attendance.12 Additionally, a dysphonic voice is linked to decreased student performance.13 The economic cost of the education and health system due to dysphonia among teachers is heavy. The treatment expenses for voice problems and related absenteeism in the teaching profession alone was conservatively estimated to be USD 2.5 billion annually in the United States of America.14
Voice care interventions are aimed at voice recovery and making it functional for professional use and communication. There are various voice care interventions, and voice amplification in combination with vocal hygiene has been reported to be effective.15 Voice amplifiers are considered successful preventive and treatment measures which are also low cost. The use of voice amplifiers decreases vocal load thus reducing the impacts of dysphonia. Therefore, the introduction of an intervention program may dissipate the incidence and impacts of this disorder. Our study was targeted towards primary school teachers as the literature suggests that primary school teachers4 teaching lower grades (i.e., younger aged pupils)7 are at an increased risk for dysphonia. Our study aimed to determine the effectiveness of a voice care program among primary school teachers in a district in northeastern Malaysia.
Methods
We conducted a community trial involving eight primary schools randomly selected from the list of public primary schools in a district of northeastern Malaysia. All teachers who were permanent staff from these schools were invited to fill in the self-administered, translated, and validated Malay-Voice Handicap Index-10 (M-VHI-10) questionnaire to determine voice handicap based on individual self-perception.9 A total of 331 out of 395 (83.8%) teachers responded. Data collection was carried out from April to June 2016.
Teachers with M-VHI-10 scores of five or more (n = 86) were randomized into an intervention (four schools, n = 43) and control group (four schools, n = 45). Teachers who were under otorhinolaryngology follow-up and used voice amplification for teaching were excluded from the study. The background of the teachers such as sociodemographic, lifestyle, and occupational characteristics (except for maximum number of students per class) were similar between the intervention and control groups. The baseline M-VHI-10 scores between both groups were comparable.
Ethical clearance was obtained from the Human Research Ethics Committee, Universiti Sains Malaysia (USM) (Reference Code: USM/JEPeM/15040149). Additional approvals to conduct our study in the schools were granted by the Malaysian Ministry of Education and the State Education Department. All school headmasters from the selected schools were briefed on the study procedures. Informed consent was obtained from all teachers before data collection and participation in the study.
Teachers in the intervention group were prescribed with the elements of the voice care program, which included personal voice amplification (Ken Pro portable amplifier), vocal hygiene instructions, and a voice amplifier diary. The voice care program comprised of lectures on vocal hygiene, voice amplification, technical skills training on the usage of the voice amplifiers, and a briefing regarding participation in the voice care program as well as a question and answer session. These sessions were 30 minutes each (two hours in total) and delivered by the same speaker. The program was held in the respective schools at a date and time determined by the school’s administration. A fact booklet regarding vocal hygiene was distributed to communicate and enlighten teachers regarding dysphonia and its causes, symptoms, and impact, and voice care approaches.
The control group was not given any intervention but received the vocal hygiene fact booklet after the post-intervention assessment was carried out. There were no blinding or matching procedures performed. After eight weeks, both intervention and control groups were reassessed using the M-VHI-10.
Initially, baseline comparisons between intervention and control groups were performed. The independent t-test was used for continuous variables, and the Chi-square or Fisher’s exact test for categorical variables between the intervention and control groups. The effectiveness of the voice care program was assessed by the difference of total M-VHI-10 scores between the intervention and control group using repeated measures analysis of covariance (RM ANCOVA). This analysis would also control for the baseline difference (i.e., maximum number of students per class). Per protocol analysis was used, meaning only teachers who completed the allocated protocol were included in the analysis. The level of significance was set at p < 0.050. Adjusted means, 95% confidence interval (CI), and p-values were presented to establish the effectiveness of the program. Data analyses were conducted using SPSS Stastistics (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp).
Figure 1 presents the flow diagram for this study. Initially, 395 primary teachers from eight randomly selected schools were assessed for eligibility from which 89 were randomized and allocated into an intervention and control group (four schools each). In the intervention group, 43 teachers received the prescribed intervention (one was absent and two were lost to follow-up). In the control group, there were no dropouts. Per protocol analysis was used, and the final number of teachers who completed the allocated protocol and were analyzed were 41 in the intervention group and 45 in the control group.
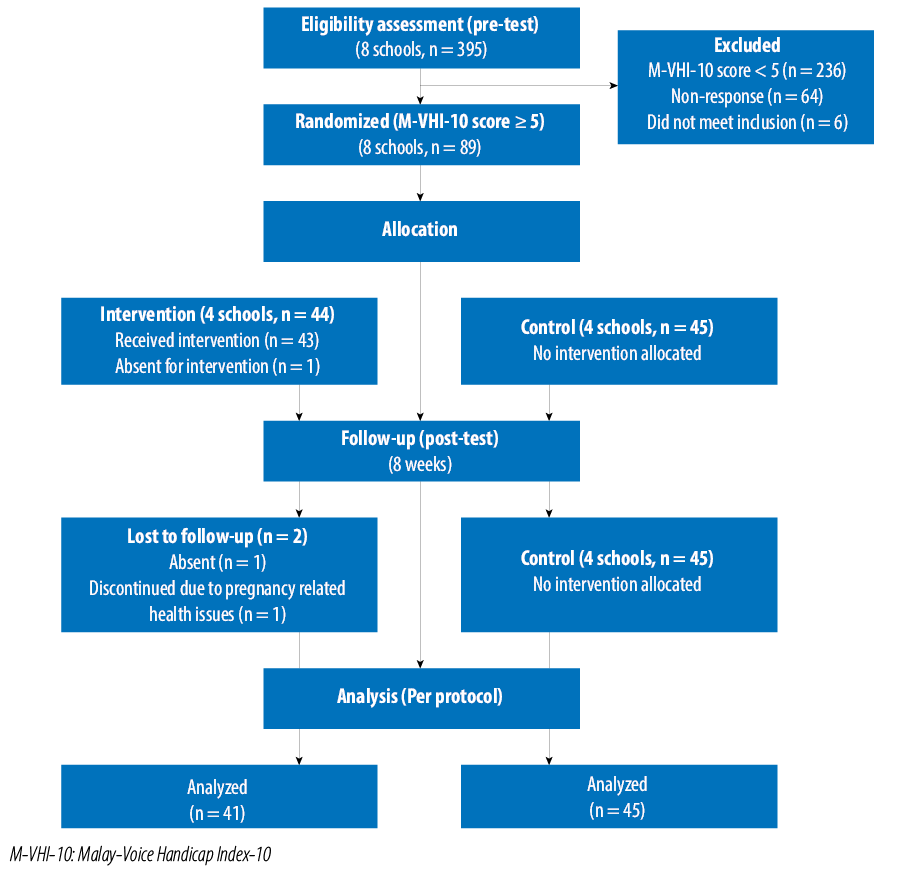
Figure 1: Flow diagram of the study.
Results
Teachers with M-VHI-10 scores of five and above were divided into an intervention (n = 43) and control group (n = 45). In the intervention group, the number of teachers from the four schools respectively was 3, 8, 14, and 18 teachers and in the control group the number of teachers was 8, 10, 11, and 16.
The mean age of the teachers in the intervention group was 43.5±7.2 years and 45.5±7.5 years in the control group. The majority of teachers were married and female. Baseline M-VHI-10 scores were similar in the intervention and control groups (p = 0.786). However, there was a significant difference in the maximum number of students per class (p = 0.032). Therefore, this variable was controlled as a confounder in RM ANCOVA. The other baseline parameters observed were comparable between the two groups (p ≥ 0.050) [Table 1].
Teachers reported using the voice amplifiers during 77.8% of classroom teaching hours. Table 2 presents the results from RM ANCOVA. The mean difference between M-VHI-10 scores after controlling for the maximum number of students per class was significant between intervention and control groups (F-stat (df): 5.53 (1,79), p = 0.021). The adjusted means (95% CI) at baseline were 9.65 (7.53–11.56) and 10.01 (8.05–11.97) in the intervention and control groups, respectively. The decrease was greater in the intervention group (adjusted means (95% CI): 3.99 (2.37–5.61)) compared to the control group (adjusted means (95% CI): 8.62 (7.12–10.13)).
Table 1: Comparison of descriptive characteristics of the participants between the intervention and
control groups.
|
Age, years |
|
43.5 ± 7.2 |
|
45.5 ± 7.5 |
0.389a |
|
Sex |
|
Male |
12 (29.3) |
|
12 (26.7) |
|
0.788b |
|
Female |
29 (70.7) |
|
33 (73.3) |
|
|
|
Marital status |
|
Married |
38 (92.7) |
|
44 (97.8) |
|
0.344c |
|
Single/divorced/widowed |
3 (7.3) |
|
1 (2.2) |
|
|
|
Number of children |
|
4.2 ± 2.2 |
|
4.2 ± 2.2 |
0.961a |
|
Occupational duration of
employment, years |
|
17.7 ± 8.4 |
|
19.6 ± 8.4 |
0.443a |
|
Subjects taught, n |
|
2.6 ± 1.4 |
|
2.1 ± 1.3 |
0.365a |
|
Teaching hours per week, n |
|
18.1 ± 15.1 |
|
15.5 ± 4.7 |
0.134a |
|
Maximum students per class |
|
29.6 ± 11.3 |
|
34.3 ± 6.1 |
0.032a |
|
Lifestyle |
|
Smoker |
|
Yes |
3 (7.3) |
|
4 (8.9) |
|
0.766b |
|
No |
38 (92.7) |
|
40 (91.1) |
|
|
|
Coffee consumption, cups/day |
|
0.9 ± 0.8 |
|
1.0 ± 1.8 |
0.680a |
aIndependent t-test; bChi-square test; cFisher’s exact test.
Table 2: M-VHI-10 scores between intervention and control group.
|
Intervention |
9.65 (7.53–11.56) |
3.99 (2.37–5.61) |
5.53 (1,79) |
0.021 |
M-VHI-10: Malay-Voice Handicap Index-10; CI: confidence interval; VHI: voice handicap index.
aRM ANCOVA: repeated measures analysis of covariance was applied while controlling covariate maximum number of students per class.
Box’s test: Box’s M = 5.98 (p = 0.121).
Levene’s test: pre-VHI (p = 0.217), post-VHI (p = 0.195).
Partial eta square for intervention effect = 0.065.
Wilk’s Lambda test (p = 0.634).
Discussion
We used a self-perceived outcome-based measure (total M-VHI-10 score) tool to evaluate the effectiveness of the voice care program (voice amplification and vocal hygiene instruction), which was administered to teachers with a score of five and above. There was a significant intervention effect observed between the two groups over the eight weeks after controlling for confounding factors. Our study provides credible evidence to support the effectiveness of a voice care program among school teachers.
Another study similarly administered this combined approach on a group of teachers and established it to be effective in reducing voice handicap index scores.15 Preceding studies also revealed voice amplification to be a valuable tool despite being utilized only as a single treatment approach.16,17 Amplification was observed to be the fastest way in improving overall voice quality.18 Theoretically, by using voice amplifiers less voicing effort is needed, thus decreasing vocal load and vibration dose.19 This promotes voice recovery, prevents vocal fatigue and damage to the vocal apparatus. Consequently, after the intervention period, teachers perceived that their voice handicap had diminished considerably.
The literature suggests that vocal hygiene as a sole strategy for dysphonia shows minimal but favorable results.20 It has been recommended that vocal hygiene provides greater benefit when used in conjunction with other forms of treatment such as voice amplification.16 In our study, vocal hygiene was infused into the voice care program and as it was intended to be exclusively didactic. It would have been a missed opportunity in increasing awareness and carrying out health education regarding this occupational disorder on this group of vulnerable workers.
In our study, self-reported compliance in the amplifier diaries reflected that teachers used the voice amplifiers during 77.8% of classroom teaching hours, 57% used the amplifiers for more than 80% of teaching hours, and 95.0% for more than 50%. Bovo et al,15 stated that 50% of teachers used the amplifier continuously and 40% used it for a limited number of hours, and Roy et al,16 reported 95% compliance in voice amplification use and 80% in vocal hygiene. Another study reported low compliance in 28.6% of teachers using vocal warm-up as a voice care approach and 17.6% in a breathing training group.21 In summary, voice amplification generally yielded good compliance among teachers compared to other approaches.
There were no unpredictable events such as damaged or faulty amplifiers. There were two (4.7%) dropouts, as one teacher had to withdraw from the study due to pregnancy-related problems that required sick leave and absenteeism, and the other teacher did not return the post-test questionnaire. Santos et al,22 observed a higher dropout rate of 34% when teachers were assigned to speech therapy.
There were numerous possibilities attributable to the success of the voice care program. Firstly, the portable voice amplifier was convenient in terms of portability, mobility, and size (8 × 4 × 10 cm) and weight (300 g). The teachers had the option to clip it onto their belts or sling it around their necks. The teachers had freedom of movement even when connected to the amplifier. In comparison, the voice amplifier used by Bovo et a,15 was 450 g with physical dimensions of 18 × 8 × 6 cm. However, the long-term durability and the lifespan of these devices are unknown.
Secondly, there was a technical skills training on the usage of the portable voice amplifiers. Teachers tested the equipment under supervision and asked for problem-solving methods (e.g., how to reduce the Larsen effect and troubles in operating the device) during the question and answer session. This session was held after taking into consideration a previous study that reported teachers encountered several technical problems due to the lack of skill in operating the equipment.23
Thirdly, the strategies employed in the implementation of the program were the group-based approach intervention, based in the workplace setting. This possibly played a key role in this study’s effectiveness. The voice care program was carried out in the teacher’s respective schools at an agreed time determined by the school’s administration. The four schools were visited at separate times. Also, support from the school’s administration and convenient access to the program were probable factors in the remarkable turn out rate of 97.7%.
Workplace-based interventions catered for teachers with dysphonia were successful in terms of improving individual’s risk, attitude and awareness.24 This approach has been seen to reduce health risks, increase productivity, decrease absenteeism, improve morale, and improve employee satisfaction.25 Moreover, the intervention participants did not have to skip work to enroll in this study.
Professionals have highlighted that group therapy is a strong method of intervention in the treatment of dysphonia as it allows for an interactive dynamic session.26 Furthermore, the advantage of the group over individual interventions includes knowing that others share the same difficulties and challenges and promotes support within the group.27 Thus, this intervention approach presumptively had a positive effect on the favorable outcome of the voice care program among the primary school teachers.
Another advantage is that the cost of our intervention approach was relatively low. The Ken Pro Professional portable amplifier was USD 31, and the fact booklet was USD 1. Furthermore, since the voice care program was held in the school setting, there were no rental or overhead costs incurred. In comparison, the ChatterVox portable amplifier used by Roy et al,16 was approximately USD 200.28 The Proel WAP 1 portable amplifier utilized by Bovo et al,15 was USD 55.29 Therefore, even though the two aforementioned studies declared that their amplifiers were a low-cost, effective treatment in reducing voice handicap among teachers, ours was just a fraction of that cost.
Several limitations should be considered while interpreting the results of this study. Even though the VHI questionnaire is regarded as the gold standard for the measurement of subjective suffering caused by dysphonia,30 the self-reported M-VHI-10 scores are subjective and may vary across individuals as every person has different thresholds for perceiving the severity of vocal symptoms or what they feel is a normal functioning voice. Additionally, the adherence to vocal hygiene was not specifically measured, and the assessment of the solitary effect of this method was beyond the scope of our study. Besides this, the Hawthorne effect where positive change is observed in a group of persons taking part in a study should be accounted. However, regarding assessing the effectiveness of the study, the Hawthorne effect is applied equally to both, treatment and control arms and should not affect the assessment of the difference between these two groups.
Conclusion
The results of our study support the use of voice amplification in adjunct with vocal hygiene instruction as a prevention and treatment modality to reduce voice handicap among teachers. Our study demonstrates encouraging evidence on the low-cost voice care program as well as the success of group and workplace-based approaches in the school setting. We recommend that screening be conducted for voice problems in the school setting, and teachers consult a healthcare professional for clinical verification, diagnosis, and treatment. These efforts are imperative to prevent further escalation and magnitude of this occupational health problem.
Disclosure
The authors have no conflict of interest to declare. The study was funded by the Universiti Sains Malaysia (Grant no: 304/PPSP/61313199).
Acknowledgements
We would like to express our gratitude to Universiti Sains Malaysia for supporting this research and the Ministry of Education Malaysia for their approval. We thank all school administrators, teachers, and support staff for their participation in this study.
references
- 1. Lee SY, Lao XQ, Yu IT. A cross-sectional survey of voice disorders among primary school teachers in Hong Kong. J Occup Health 2010;52(6):344-352.
- 2. Cantor Cutiva LC, Vogel I, Burdorf A. Voice disorders in teachers and their associations with work-related factors: a systematic review. J Commun Disord 2013 Mar-Apr;46(2):143-155.
- 3. Williams NR. Occupational groups at risk of voice disorders: a review of the literature. Occup Med (Lond) 2003 Oct;53(7):456-460.
- 4. Coyle SM, Weinrich BD, Stemple JC. Shifts in relative prevalence of laryngeal pathology in a treatment-seeking population. J Voice 2001 Sep;15(3):424-440.
- 5. Preciado J, Pérez C, Calzada M, Preciado P. [Prevalence and incidence studies of voice disorders among teaching staff of La Rioja, Spain. Clinical study: questionnaire, function vocal examination, acoustic analysis and videolaryngostroboscopy]. Acta Otorrinolaringol Esp 2005 May;56(5):202-210.
- 6. Angelillo M, Di Maio G, Costa G, Angelillo N, Barillari U. Prevalence of occupational voice disorders in teachers. J Prev Med Hyg 2009 Mar;50(1):26-32.
- 7. Thomas LB, Stemple JC. Voice therapy: does science support the art. Communicative Disorders Review 2007;1(1):49-77.
- 8. RoscellaInja HA. Prevalence of voice disorder among primary school teachers in Bintulu, Sarawak. Malays J Public Health Med 2016;16(2):89-98.
- 9. Moy FM, Hoe VC, Hairi NN, Chu AH, Bulgiba A, Koh D. Determinants and effects of voice disorders among secondary school teachers in Peninsular Malaysia using a validated Malay Version of VHI-10. PLoS One 2015 Nov;10(11):e0141963.
- 10. Ziegler A, Gillespie AI, Abbott KV. Behavioral treatment of voice disorders in teachers. Folia Phoniatr Logop 2010;62(1-2):9-23.
- 11. Van Houtte E, Claeys S, Wuyts F, Van Lierde K. The impact of voice disorders among teachers: vocal complaints, treatment-seeking behavior, knowledge of vocal care, and voice-related absenteeism. J Voice 2011 Sep;25(5):570-575.
- 12. Black AT, Seder RC, Kekahio W. Review of research on student nonenrollment and chronic absenteeism: a report for the Pacific Region. Washington, DC:US. Regional Educational Laboratory Pacific. 2014 [cited 2017 October 1]. Available from: https://ies.ed.gov/ncee/edlabs/regions/pacific/pdf/REL_2014054.pdf.
- 13. Rogerson J, Dodd B. Is there an effect of dysphonic teachers’ voices on children’s processing of spoken language? J Voice 2005 Mar;19(1):47-60.
- 14. Verdolini K, Ramig LO. Review: occupational risks for voice problems. Logoped Phoniatr Vocol 2001;26(1):37-46.
- 15. Bovo R, Trevisi P, Emanuelli E, Martini A. Voice amplification for primary school teachers with voice disorders: a randomized clinical trial. Int J Occup Med Environ Health 2013 Jun;26(3):363-372.
- 16. Roy N, Weinrich B, Gray SD, Tanner K, Toledo SW, Dove H, et al. Voice amplification versus vocal hygiene instruction for teachers with voice disorders: a treatment outcomes study. J Speech Lang Hear Res 2002 Aug;45(4):625-638.
- 17. Roy N, Weinrich B, Gray SD, Tanner K, Stemple JC, Sapienza CM. Three treatments for teachers with voice disorders: a randomized clinical trial. J Speech Lang Hear Res 2003 Jun;46(3):670-688.
- 18. Simberg S, Sala E, Rönnemaa AM. A comparison of the prevalence of vocal symptoms among teacher students and other university students. J Voice 2004 Sep;18(3):363-368.
- 19. Morrow SL, Connor NP. Voice amplification as a means of reducing vocal load for elementary music teachers. J Voice 2011 Jul;25(4):441-446.
- 20. Behlau M, Oliveira G. Vocal hygiene for the voice professional. Curr Opin Otolaryngol Head Neck Surg 2009 Jun;17(3):149-154.
- 21. Pereira LP, Masson ML, Carvalho FM. Vocal warm-up and breathing training for teachers: randomized clinical trial. Rev Saude Publica 2015;49:67.
- 22. Santos LR, Almeida L, Teixeira LC, Bassi I, Assunção AA, Gama AC. Adherence of the dysphonic teachers in speech therapy. Codas 2013;25(2):135-140.
- 23. Jónsdottir VI, Boyle BE, Martin PJ, Sigurdardottir G. A comparison of the occurrence and nature of vocal symptoms in two groups of Icelandic teachers. Logoped Phoniatr Vocol 2002;27(3):98-105.
- 24. Occupational Health Intervention Technologies. Workplace intervention. [cited 2017 June 1]. Available from: http://www.ctdmap.com/products/workplaceintervention.
- 25. Health and Safety Authority. Workplace health promotion: Workplace health toolkit for small businesses. [cited 2017 May 31]. Available from: http://www.hsa.ie/eng/Publications_and_Forms/Publications/Safety_and_Health_Management/Section%2014%20Workplace%20Health%20Promotion.pdf.
- 26. Almeida LN, Fahning AK, Trajano FM, Anjos UU, Almeida AA. Group voice therapy and its effectiveness in the treatment of dysphonia: a systematic review. Rev CEFAC 2015 Nov-Dec;17(6):2000-2008.
- 27. Gidron Y. Group therapy /intervention. InEncyclopedia of Behavioral Medicine. Springer: New York, NK; 2013. p. 880-881.
- 28. Amazon.com. Chattervox Amplifier. [cited 2017 March 31]. Available from: https://www.amazon.com/Chattervox-Speech-Amplifier-Transdermal-icrophone/dp/B00ZRZOIWO/ref=sr_1_1_a_it?ie=UTF8&qid=1542605653&sr=8-1-spons&keywords=chattervox+voice+amplifier&psc=1&smid=AYSGXV7QRGP7K.
- 29. Art Sound and Lights Audiovisual Services. Proel Wap-1. [cited 2017 March 31]. Available from: https://www.artsound.gr/catalog/proel-portable-speaker-eith-headmic-p-35004.html?language=en.
- 30. Grässel E, Hoppe U, Rosanowski F. [Grading of the Voice Handicap Index]. HNO 2008 Dec;56(12):1221-1228.