|
Introduction
Bronchogenic cysts originate from abnormal budding of the tracheal diverticula during the embryological period.1 During the third week of embryonic development, the dorsal portion of the primitive foregut lengthens to form the oesophagus, and the ventral portion of the primitive gut undergoes differentiation to form the tracheobronchial tree. Insuffiency in the process of growing of the ventral foregut will give rise to bronchogenic cysts.2,3 The eventual location of the bronchogenic cysts depends on the stage of development in which the errors occur.2,4 Mediastinum is the most common extrapulmonary location. Other rare location like lingual, intra-abdominal and cutaneous regions have also been reported.1 Cutaneous bronchogenic cysts are the most infrequent lesions that are diagnosed by histopathological examination. However, the scapular bronchogenic cyst is an extremely rare form of this anomaly.5,6 Hereby, we describe a boy with a scapular bronchogenic cyst where the diagnosis was made by histopathological examination.
Case report
A three years old boy with no comorbids was brought to the Pediatric Surgery Department at Sultan Qaboos University Hospital, Sultanate of Oman, with complaints of left sided suprascapular cystic lesion starting 2 years back. It was gradually increasing in size and not associated with pain, fever or weight loss. There was no other swelling elsewhere in the body and no history of trauma. On examination, there was a cystic swelling overlying the left scapular region measuring 4 × 3 cm in size, which was smooth walled, fluctuant, nontender, and freely mobile. There was a scar overlying the swelling. Systemic examination was normal. He was evaluated by CT scan in another hospital which showed oval complex cystic lesion over the left scapular spine measuring 4 × 3 × 4 cm with calcification as well as the impression of the teratodermoid subcutaneous cyst. Total excision of the cyst was carried out. Pre-operatively, the cyst was adherent to the bone but without any communication with the joint cavity. The post-operative condition of the patient was uneventful. Macroscopically, the specimen consisted of a smooth walled unilocular cyst, 4 × 3.5 × 2 cm with a wall thickness of 0.2 - 0.4 mm and containing yellowish mucoid material. (Fig. 1)
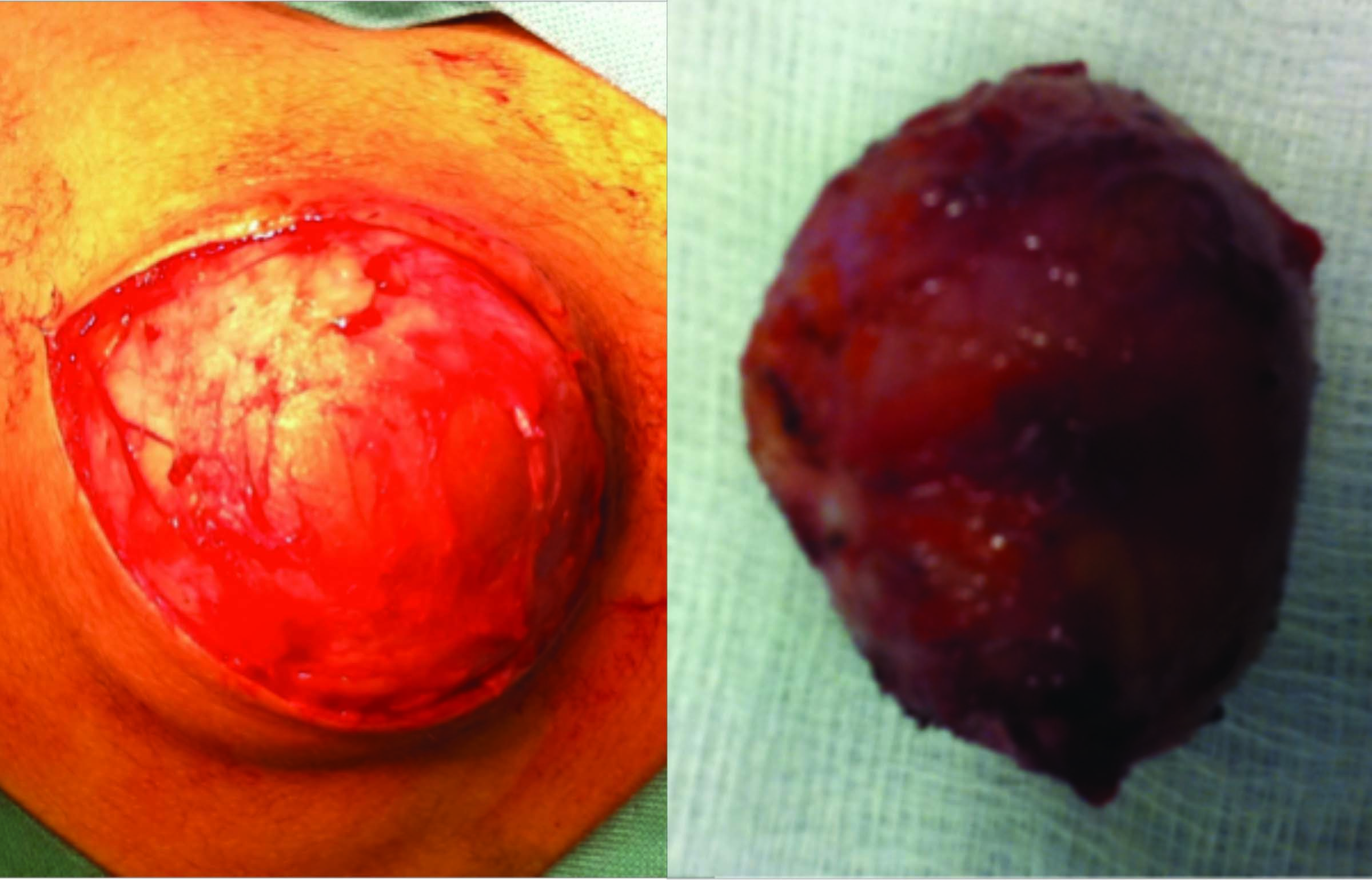
Figure 1: Scapular bronchogenic cyst.
Histopathological examination showed a cyst wall predominantly lined by ciliated pseudo stratified columnar epithelium with interspersed goblet cells and partly by stratified squamous epithelium. Smooth muscle cells, adipose tissue, nerve bundles as well as seromucinous glands were present in its wall. The appearances were consistent with the cutaneous bronchogenic cyst. (Figs. 2, 3)
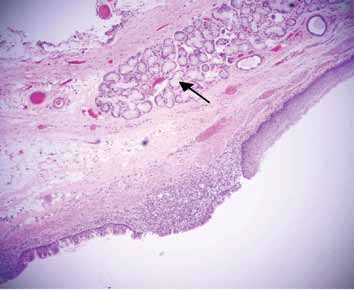
Figure 2: The cyst is lined by ciliated pseudocolumnar respiratory type epithelium (left) and squamous epithelium (right). Sermucinous glands are present in its wall (H&E).
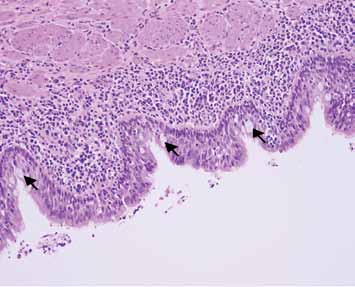
Figure 3: High power view of the ciliated respiratory epithelium with interspersed goblet cells (arrow) and smooth muscle bundles in it (H&E).
Discussion
Bronchogenic cysts are very rare lesions; the reported incidence being 1 in 42000-68000.7 Abnormal separations of developing lung tissue result in the formation of these congenital cysts. Therefore, the thoracic cavity is the most common location for these cysts.8-10
Extra-thoracic cutaneous bronchogenic cysts are observed soon after birth or in early childhood as cystic masses. The usual sites of these lesions are suprasternal notch, presternal area, the neck and scapula.11,12 Scapular bronchogenic cysts are extremely rare among the extrathoracic variety. The division of developing lung bud, formation of the chest wall and scapula with its musculature are occurrences that imbricate during organogenesis.5 It is anticipated that accessory buds from the tracheobronchial tree/ primitive foregut migrated from the thorax in an aberrant manner to lie in periscapular positions. Additional proposed mechanisms for such devious cutaneous locations include in situ growth of a respiratory epithelium due to metaplasia of mature pre-existing cutaneous tissue and primary bizarre differentiation (heterotopia) in the developing skin.13
Scapular cutaneous bronchogenic cyst presents as a progressively enlarging soft tissue swelling or a discharging sinus.14 Most of these are present shortly after birth or in early childhood and are more common among the male population.5 Along with the current case, 69 cutaneous bronchgenic cysts have been reported in the literature, with 14 (20.3%) located in the scapular region, (Table 1). Of these 14 scapular bronchogenic cysts, only 2 cases presented in females.1 These cases have similar male preponderance as other locations of cutaneous bronchogenic cysts. Also, among these cases, 11 (78.6%) were diagnosed before the age of 4 years. In 1971, Fraga reported 30 cases of bronchogenic cysts, which is the largest population of cutaneous bronchogenic cysts, 12 out of the 30 patients (40%) were diagnosed below the age of 4 years.4 The majority of these cases presented with a swelling adjacent to the scapula that drained clear fluid. Remarkably, all the cysts were located subcutaneously.11 The reason for early detection may be the anatomical location itself as the scapular area is relatively exposed when compared with other parts of the body.1
Table 1: Scapular bronchogenic cyst reported in the literature (1971-2012)
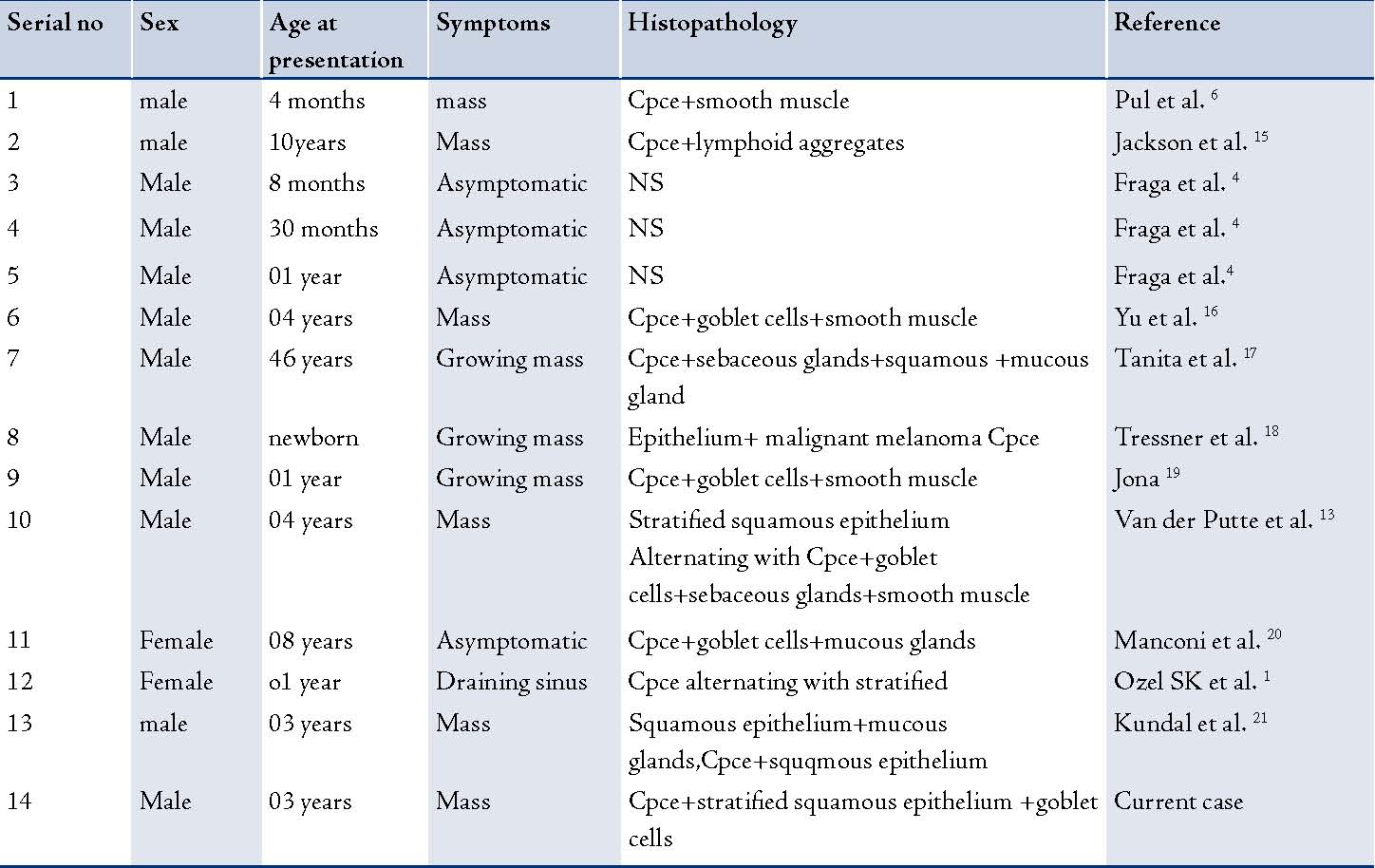
cpce-ciliated pseudostrtified columnar epithelium; NS-not specified
Proper imaging intervention (sinogram, chest X-ray, CT/MRI) will facilitate the evaluation of intrathoracic continuation as well as planning for the operative approach.21 The definitive treatment of scapular lesions is total surgical excision due to potential risk of infection; and more rarely, a malignant transformation of the epithelium in a scapular bronchogenic cyst.17 The pathological diagnosis is carried out based on the presentation of one or more tracheobronchial structures in the cyst wall. Frequently, hyaline cartilage, smooth muscle cells, elastic fibers, fibrous tissue, neural cells and seromucous glands can be seen.1
Conclusion
This very rare congenital anomaly may present as common superficial skin lesion. Therefore, pediatric surgeons should be aware while dealing with superficial skin lesions in the scapular regions. The final diagnosis is based on the histopathological findings in the majority of cases.
Acknowledgements
The authors reported no conflict of interest and no funding was received on this work.
References
1. Ozel SK, Kazez A, Koseogullari AA, Akpolat N. Scapular bronchogenic cysts in children: case report and review of the literature. Pediatr Surg Int 2005 Oct;21(10):843-845.
2. Rodgers BM, Harman PK, Johnson AM. Bronchopulmonary foregut malformations. The spectrum of anomalies. Ann Surg 1986 May;203(5):517-524.
3. Nobuhara KK, Gorski YC, La Quaglia MP, Shamberger RC. Bronchogenic cysts and esophageal duplications: common origins and treatment. J Pediatr Surg 1997 Oct;32(10):1408-1413.
4. Fraga S, Helwig EB, Rosen SH. Bronchogenic cysts in the skin and subcutaneous tissue. Am J Clin Pathol 1971 Aug;56(2):230-238.
5. Das K, Jackson PB, D’Cruz AJ. Periscapular bronchogenic cyst. Indian J Pediatr 2003 Feb;70(2):181-182.
6. Pul N, Pul M. Bronchogenic cyst of the scapular area in an infant: case report and review of the literature. J Am Acad Dermatol 1994 Jul;31(1):120-122.
7. Sanli A, Onen A, Ceylan E, Yilmaz E, Silistreli E, Açikel U. A case of a bronchogenic cyst in a rare location. Ann Thorac Surg 2004 Mar;77(3):1093-1094.
8. Rodgers BM, Harman PK, Johnson AM. Bronchopulmonary foregut malformations. The spectrum of anomalies. Ann Surg 1986 May;203(5):517-524.
9. Nobuhara KK, Gorski YC, La Quaglia MP, Shamberger RC. Bronchogenic cysts and esophageal duplications: common origins and treatment. J Pediatr Surg 1997 Oct;32(10):1408-1413.
10. Fraga S, Helwig EB, Rosen SH. Bronchogenic cysts in the skin and subcutaneous tissue. Am J Clin Pathol 1971 Aug;56(2):230-238.
11. Schouten van der Velden AP, Severijnen RS, Wobbes T. A bronchogenic cyst under the scapula with a fistula on the back. Pediatr Surg Int 2006 Oct;22(10):857-860.
12. Zvulunov A, Amichai B, Grunwald MH, Avinoach I, Halevy S. Cutaneous bronchogenic cyst: delineation of a poorly recognized lesion. Pediatr Dermatol 1998 Jul-Aug;15(4):277-281.
13. van der Putte SC, Toonstra J. Cutaneous ‘bronchogenic’ cyst. J Cutan Pathol 1985 Oct;12(5):404-409.
14. Muramatsu T, Shirai T, Sakamoto K. Cutaneous bronchogenic syst. Int J Dermatol 1990;2:143-144 .
15. Miller OF III, Tyler W. Cutaneous bronchogenic cyst with papilloma and sinus presentation. J Am Acad Dermatol 1984 Aug;11(2 Pt 2):367-371.
16. Yu HJ, Kwon HM, Park JW, Hwang DK, Ahn DK, Park YW. A case of cutaneous bronchogenic cyst over the left scapula. J Dermatol 2001 Oct;28(10):572-575.
17. Tanita M, Kikuchi-Numagami K, Ogoshi K, Suzuki T, Tabata N, Kudoh K, et al. Malignant melanoma arising from cutaneous bronchogenic cyst of the scapular area. J Am Acad Dermatol 2002 Feb;46(2)(Suppl Case Reports):S19-S21.
18. Tresser NJ, Dahms B, Berner JJ. Cutaneous bronchogenic cyst of the back: a case report and review of the literature. Pediatr Pathol 1994 Mar-Apr;14(2):207-212.
19. Jona JZ. Extramediastinal bronchogenic cysts in children. Pediatr Dermatol 1995 Dec;12(4):304-306.
20. Manconi R, Bolla G, Pavon I. Congenital bronchogenic subcutaneous cyst of the back. A case report and review of the literature. Pediatr Med Chir 2003 Sep-Oct;25(5):364-366.
21. Kundal AK, Zargar NU, Krishna A. Scapular bronchogenic cyst. J Indian Assoc Pediatr Surg 2008 Oct;13(4):147-148.
|