Abdominal pregnancy is defined as pregnancy anywhere within the peritoneal cavity, exclusive of tubal, ovarian, or broad ligament locations.1 The Pouch of Douglas (POD) is the most common location of abdominal pregnancy followed by the mesosalpinx and omentum. However, implantation on other abdominal organs such as the spleen, liver, and appendix is also reported.2–4 Abdominal pregnancy is thought to represent around 1–1.5% of all ectopic pregnancies with an estimated incidence of 1:8000–10 000 pregnancies.5
It is a serious and potentially life-threatening condition, mainly due to the risk of massive hemorrhage from a partially or totally separated placenta at any stage of pregnancy. Maternal mortality is around 7.7-times that of other locations of ectopic pregnancy and 90-times that of intrauterine pregnancy.6 From the world literature, maternal mortality is estimated to be 2–30%,7 while perinatal mortality in those undiagnosed is 40–95%.8,9
Abdominal pregnancies are either primary or secondary, secondary being the more common type.7,10 For the diagnosis of primary abdominal pregnancy, Studdiford’s criteria need to be fulfilled. These include: (a) normal bilateral fallopian tubes and ovaries; (b) the absence of utero-peritoneal fistula; and (c) pregnancy related exclusively to the peritoneal surface and early enough to eliminate the possibility of secondary implantation following a primary location in the tube.11 Secondary abdominal pregnancies refer to pregnancies that originated in the tubes or, less commonly, the ovaries and reimplant in the peritoneum where the embryo or fetus continues to grow.10
We present two cases of confirmed abdominal pregnancies admitted with different initial diagnoses. A high index of clinical suspicion will improve diagnosis and lead to successful management.
Case Report
Case one
A 37-year-old Filipino woman, gravida 3, para 2, with previous normal vaginal deliveries (the youngest was 15-years-old) presented to the accident and emergency (A&E) unit at 12 weeks gestation with abdominal pain and constipation. She had a normal pulse and mildly increased blood pressure. She was known to be hypertensive and taking methyldopa tablets 250 mg twice daily. Abdominal examination revealed a distended abdomen with tympanic percussion and mild tenderness. Investigations showed hemoglobin levels of 10.5 g/dL, hematocrit of 31%, and normal serum amylase and lipase. A departmental scan showed a 12-week viable intrauterine pregnancy with no other remarkable findings. The patient was reassured, given dietary advice, glycerin suppositories, and an appointment to the antenatal clinic.
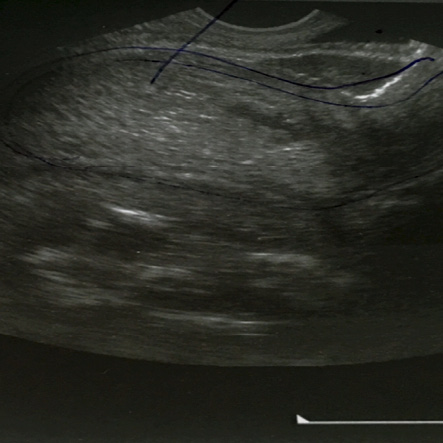
Figure 1: Ultrasound findings showing an empty uterus and a pregnancy in the Pouch of Douglas.
Two weeks later, she presented with nausea, vomiting, abdominal pain, and distention. She looked pale, and had a rapid pulse rate and normal blood pressure. Her hemoglobin was 5.1 g/dL and hematocrit 15.3%. Urgent departmental ultrasound revealed an intrauterine pregnancy of 14 weeks with large amount of abdominal fluid interpreted by the ultrasonographer as ascitic fluid. The ovaries were not properly visualized and the remaining pelvic and abdominal organs were normal. The gynecology team questioned the diagnosis and asked for magnetic resonance imaging (MRI) for further clarification, but the request was denied by the radiology department on the basis of relative contraindication.
A bedside abdominal ultrasound was done by the gynecology team, which revealed a large collection of fluid interpreted as hemoperitoneum and a viable pregnancy of around 14 to 15 weeks with vague boundaries. Transvaginal ultrasound showed a viable pregnancy located in the POD with an empty bulky uterus and normal adnexa [Figure 1].
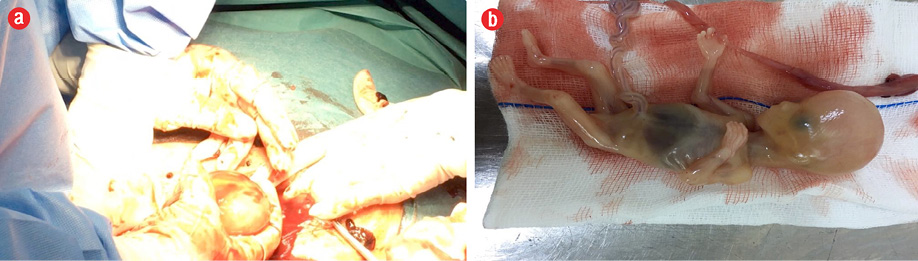
Figure 2: (a) Fetus and membranes retrieved from the Pouch of Douglas. (b) The fetus.
A laparotomy was urgently arranged which revealed the presence of around three liters of hemoperitoneum along with a viable pregnancy in the POD, which was removed intact [Figure 2]. The placenta was attached to the base of the POD and the surrounding posterior wall of the uterus, left adnexa, bowel loops, and part of the right adnexa [Figure 3]. Proper surgical dissection of the placenta from the adjacent structures was done, hemostasis was secured by stitches, cauterization, and application of topical hemostatic agents. Drains were inserted intraperitoneally, and her hemoglobin level was corrected with blood transfusion. She had a postoperative bout of paralytic ileus, which was managed conservatively. She made a good recovery and was discharged home on the fifth postoperative day.
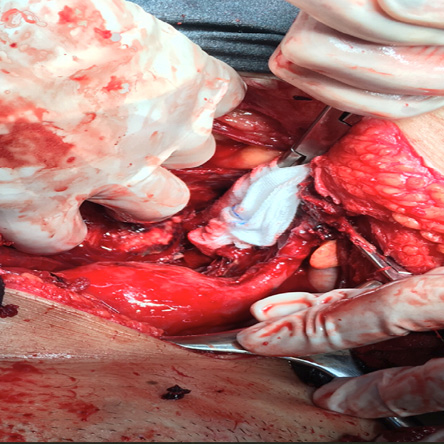
Figure 3: The area in the Pouch of Douglas where the abdominal pregnancy was retrieved.
Case two
A 36-year-old Emirati woman, para 3 + 4 miscarriages, presented to the A&E with a seven-week history of amenorrhea, mild bleeding, and abdominal pain. The patient was hemodynamically stable with a hemoglobin level of 11.2 g/dL and beta human chorionic gonadotropin (HCG) level of 14 444 mIU/mL. Transvaginal ultrasound showed an empty bulky uterus, normal both adnexa, and minimal fluid in the POD. She was admitted as a case of pregnancy of unknown location for observation and a repeat beta HCG level.
During the coming few hours, her pain and pulse rate increased. An urgent diagnostic laparoscopy revealed a hemoperitoneum of around 150 mL, a bulky uterus, and healthy right and left adnexa [Figure 4].
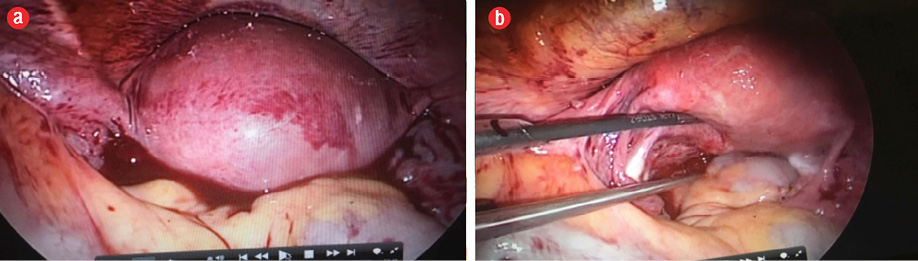
Figure 4: (a) Hemoperitoneum on entering the abdominopelvic cavity by laparoscopy. (b) Healthy left and right tubes and ovaries.
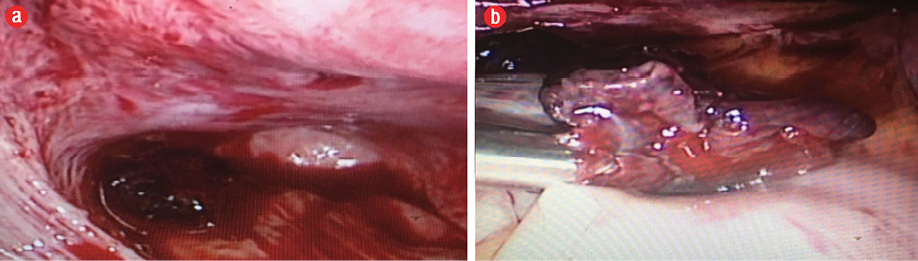
Figure 5: (a) ectopic (abdominal) pregnancy seen in the Pouch of Douglas. (b) Retrieved pregnancy.
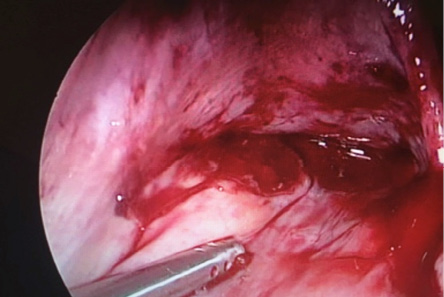
Figure 6: Bleeding raw area at the site of the attachment of the abdominal pregnancy dealt with by cautery and application of topical hemostatic agents.
There was an area of bleeding tissue deep in the POD of about 3 × 4 cm, which was removed and sent for histopathology [Figure 5]. The bleeding area was secured by cauterization and application of topical hemostatic agents [Figure 6]. Intrauterine curettage was done to rule out the possibility of retained intrauterine products of conception. The tissue retrieved was sent for histopathology.
The patient had an uneventful recovery and was discharged after 24 hours. Her beta HCG level dropped to negative in three weeks. The histopathology of the tissue from the POD revealed products of conception while that retrieved from the uterus revealed endometrial tissue with decidual reaction.
Discussion
The clinical presentation of an abdominal pregnancy can differ from that of a tubal pregnancy. Although there may be great variability in symptoms, severe lower abdominal pain is one of the most consistent findings.12 However, the risk factors for abdominal pregnancy are the same as those for tubal pregnancy.13 The recent use of progesterone-only pills and intrauterine devices with a history of surgery, pelvic inflammatory disease, sexually transmitted disease, and allergy increase the risk of ectopic pregnancy.14 The first patient had not been using any contraception and did not report any history of other risk factors. However, failure to conceive for around 15 years might indicate a history of pelvic inflammatory disease. The second patient had a history of recurrent miscarriages attributed to an earlier diagnosis of polycystic ovary syndrome for which few courses of progesterone were prescribed previously to regulate her cycle and enhance the luteal phase.
Ultrasound, especially transvaginal, remains the first-line tool for diagnosing abdominal pregnancy.15 Experience, vigilance, clinical correlation, and a high index of suspicion are of utmost importance in cases of clinical ambiguity and questionable findings. In the first case, we were able to diagnose an abdominal pregnancy with the use of bedside transabdominal and then transvaginal ultrasound imaging. The clinical presentation of the patient was not consistent with the departmental scan findings, which encouraged the gynecology team to do their own assessment. MRI provides additional information in patients who need a precise diagnosis in cases of ambiguity and can help define the extent of abdominal and pelvic organs invasion by the placental tissue, and is not contraindicated when needed.16
Diagnostic laparoscopy can be invaluable in answering queries when imaging techniques are not conclusive and the patient’s condition is alarming.17 With our second patient, the primary diagnosis was pregnancy of an unknown location and, as the patient was clinically stable, a period of waiting was suggested hoping to have a spontaneous decline in the level of beta HCG. However, the patient started to have increasing pain for which a decision to go for urgent diagnostic laparoscopy was made. The proper and swift preparation for surgical intervention can be lifesaving.
In the first case, the deep attachment of the placenta to the whole bulk of the left adnexa indicates that the primary origin is mainly from a left tubal ectopic. While in the second case, both adnexa were normal and the pregnancy was early enough to suggest a primary abdominal pregnancy. Once abdominal pregnancy is diagnosed, open laparotomy is usually needed to allow better access to deal with placental attachment and control the bleeding.2,18 On the other hand, removal of the placental tissue is less difficult in early pregnancy as is likely to be smaller and less vascular. For this reason, laparoscopic surgery should be considered for early abdominal pregnancy.19,20
Conclusion
Failure to diagnose abdominal pregnancies can have grave consequences. Gynecologists need to have a high index of suspicion and a better understanding and interpretation of clinical and imaging findings. Ultrasound examination is the diagnostic procedure of choice in the rare cases of abdominal pregnancy. However, diagnosis can be missed if attention was not paid or if the ultrasonographer is inexperienced. MRI can be used without hesitation in cases of ambiguity. Early reversion to surgery, including minimally invasive, in cases of diagnostic uncertainty can be invaluable.
Disclosure
The authors declared no conflicts of interest.
references
- Worley KC, Hnat MD, Cunningham FG. Advanced extrauterine pregnancy: diagnostic and therapeutic challenges. Am J Obstet Gynecol 2008 Mar;198(3):297.e1-297.e7.
- 2. Nama V, Gyampoh B, Karoshi M, McRae R, Opemuyi I. Secondary abdominal appendicular ectopic pregnancy. J Minim Invasive Gynecol 2007 Jul-Aug;14(4):516-517.
- 3. Chui AK, Lo KW, Choi PC, Sung MC, Lau JW. Primary hepatic pregnancy. ANZ J Surg 2001 Apr;71(4):260-261.
- 4. Yagil Y, Beck-Razi N, Amit A, Kerner H, Gaitini D. Splenic pregnancy: the role of abdominal imaging. J Ultrasound Med 2007 Nov;26(11):1629-1632.
- 5. Gibbs RS. Danforth’s obstetrics and gynecology. 10th ed. Philadelphia: Lippincott Williams & Wilkins; 2008. p. 84.
- 6. Kun KY, Wong PY, Ho MW, Tai CM, Ng TK. Abdominal pregnancy presenting as a missed abortion at 16 weeks’ gestation. Hong Kong Med J 2000 Dec;6(4):425-427.
- 7. Parekh VK, Bhatt S, Dogra VS. Abdominal pregnancy: an unusual presentation. J Ultrasound Med 2008 Apr;27(4):679-681.
- 8. Zhang J, Li F, Sheng Q. Full-term abdominal pregnancy: a case report and review of the literature. Gynecol Obstet Invest 2008;65(2):139-141.
- 9. Adesiyun AG, Audu AI. Term extrauterine pregnancy in a Nigerian mother: a complication of uterine dehiscence. Arch Gynecol Obstet 2009 Jan;279(1):75-77.
- 10. Masukume G. Live births resulting from advanced abdominal extrauterine pregnancy, a review of cases reported from 2008 to 2013. WebmedCentral OBSTETRICS AND GYNAECOLOGY 2014; 5(1): WMC004510.
- 11. King M, Bewes PC, Cairns J, Thornton J, eds. Abdominal pregnancy in primary surgery. 2014. Chapter 8.
- 12. Nkusu Nunyalulendho D, Einterz EM. Advanced abdominal pregnancy: case report and review of 163 cases reported since 1946. Rural Remote Health 2008 Oct-Dec;8(4):1087.
- 13. Berek JS. Berek & Novak’s Gynecology. 14th ed. Philadelphia: Lippincott Williams & Wilkins; 2007. p. 628.
- 14. Ankum WM, Mol BW, Van der Veen F, Bossuyt PM. Risk factors for ectopic pregnancy: a meta-analysis. Fertil Steril 1996 Jun;65(6):1093-1099.
- 15. Cohen JM, Weinreb JC, Lowe TW, Brown C. MR imaging of a viable full-term abdominal pregnancy. AJR Am J Roentgenol 1985 Aug;145(2):407-408.
- 16. Teng HC, Kumar G, Ramli NM. A viable secondary intra-abdominal pregnancy resulting from rupture of uterine scar: role of MRI. Br J Radiol 2007 Jul;80(955):e134-e136.
- 17. Gerli S, Rossetti D, Baiocchi G, Clerici G, Unfer V, Di Renzo GC. Early ultrasonographic diagnosis and laparoscopic treatment of abdominal pregnancy. Eur J Obstet Gynecol Reprod Biol 2004 Mar;113(1):103-105.
- 18. Patel C, Feldman J, Ogedegbe C. Complicated abdominal pregnancy with placenta feeding off sacral plexus and subsequent multiple ectopic pregnancies during a 4-year follow-up: a case report. J Med Case Rep 2016 Feb;10:37.
- 19. Morita Y, Tsutsumi O, Kuramochi K, Momoeda M, Yoshikawa H, Taketani Y. Successful laparoscopic management of primary abdominal pregnancy. Hum Reprod 1996 Nov;11(11):2546-2547.
- 20. Tsudo T, Harada T, Yoshioka H, Terakawa N. Laparoscopic management of early primary abdominal pregnancy. Obstet Gynecol 1997 Oct;90(4 Pt 2):687-688.