Asherman syndrome strictly comprises a combination of pain, menstrual disturbance, and subfertility in any combination.1 It involves adhesions in the endometrium leading to varying degrees of uterine cavity obliteration as a result of trauma, especially to pregnant uterus (after curettage in puerperium or after missed abortion) or secondary to genital tuberculosis.2
Hysteroscopic lysis of adhesions is the gold standard for treatment of intrauterine adhesions.3 Normal menses resume in most cases after surgery. However, surgical procedures are associated with a considerable risk of perforation, and repeated surgical procedures might be required especially in cases with severe adhesions.1–5 Cervical dilatation in Asherman syndrome can be especially difficult at times due to the presence of fibrosis at the internal or external os. The novel mini-resectoscope has an outer diameter of only 5 mm, requiring minimal cervical dilatation, compared with 10 mm dilatation required for the conventional resectoscope, thus reducing the chances of cervical trauma and uterine perforation, as well as improving postoperative pain control.6,7
Large case series published so far for assessing the effectiveness of mini-resectoscope in treating various intrauterine pathologies, such as hysteroscopic polypectomy, have shown excellent success rates.8–10 Since there is a paucity of data available evaluating the usefulness of the mini-resectoscope in the treatment of intrauterine adhesions, we conducted this randomized study comparing hysteroscopic adhesiolysis by conventional resectoscope versus the mini-resectoscope.11,12
Methods
This pilot study was conducted at All India Institute of Medical Sciences from May 2014 to September 2016 following approval by the institute’s ethics committee. One-hundred and fifty-eight infertile women with suspected intrauterine adhesions (hypomenorrhea/amenorrhea or imaging showing intrauterine synechiae [hysterosalpingogram/ultrasound/prior hysteroscopy]) underwent diagnostic hysteroscopy to confirm the diagnosis and grade the adhesions. Infertility was defined as the inability to conceive after one year of regular unprotected sexual intercourse.13 Amenorrhea was defined as the absence of menstruation for three normal menstrual cycles.14 Hypomenorrhea was defined as light menstrual flow or menses for less than two days.15 A detailed clinical history was taken to find out the cause of intrauterine adhesions. Endometrial biopsy was done in all cases to rule out endometrial tuberculosis. Analysis of the husbands’ semen was done for all.
Inclusion criteria for the study were: 1) cases with a minimal and moderate grade of adhesions on hysteroscopy (according to the March classification5), 2) complaints of infertility, with or without menstrual symptoms. Minimal adhesions implies adhesions involving < ¼ of uterine cavity, thin or filmy adhesions, either clear or minimal involvement of ostial areas and upper fundus.5 Moderate adhesions implies adhesions involving ¼ to ¾ of uterine cavity, no agglutination of walls, adhesions only, partially occluded ostial areas and upper fundus.5 Exclusion criteria were: 1) adhesions of severe grade on hysteroscopy, 2) histologically proven endometrial tuberculosis, 3) other endocrinological disorders causing menstrual symptoms, 4) abnormal husband semen parameters, and 5) presence of other contributing factors to infertility.
Seventy patients fulfilling these criteria were shortlisted. On further workup, one patient was found to have uterine myomas, two were found to have endometrial tuberculosis on biopsy, and three patients’ husbands were found to have abnormal semen parameters. These six cases were excluded from the study.
The remaining 64 cases were recruited and randomized into two groups. At the time of initiating the study, serial numbers from 1 to 70 were taken and equal size of 35 numbers were selected randomly using the software Epi-InfoTM version 7.0 (CDC, Atlanta, GA, USA under OpenEpi random programme (www.openepi.com) module). The allocation sequence was concealed in stapled envelopes coded as group 1 (conventional resectoscope) and group 2 (mini-resectoscope) were retained by the statistician. Prospectively consecutively recruited patients who were found eligible and gave written consent for participating in the study were assigned numbers starting 1 to 70. The type of resectoscopic procedure to be followed was allotted by the statistician using the stapled envelopes. The patients were blinded after taking due consent to either of the two groups. Four cases did not follow-up for treatment after allocation. The modified intention-to-treat approach was followed and these four patients were excluded from the study. Thus, a final total of 60 patients divided into two groups were analyzed [Figure 1].
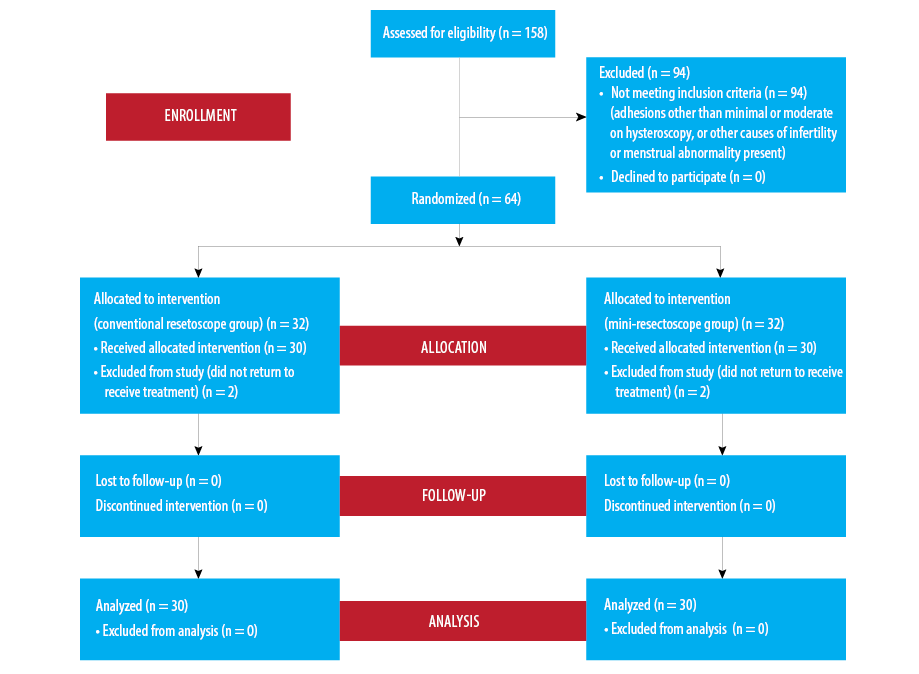
Figure 1: Flow diagram depicting the outcome of women recruited into the study.
Hysteroscopic adhesiolysis was done in the early proliferative phase of the cycle (day 6–11) under general anesthesia. All procedures were done by a single experienced operator to eliminate subject bias. Intravaginal misoprostol 400 mcg was administered for cervical ripening six hours before the procedure. Hysteroscopic adhesiolysis was done using the conventional resectoscope in the first group, henceforth named the CR group. It consisted of a 9 mm working element with a sheath and 4 mm 30° telescope (Karl Storz, Germany), along with monopolar electrode (Collin’s knife). The resectoscope was introduced into the uterine cavity after cervical dilatation using a Hegar’s dilator up to a size of 10 mm. The cavity was distended using glycine (1.5%) as the medium through an automated hysteroscopic insufflator. Karl Storz Hysteromat was used and the intrauterine pressure was not allowed to exceed 100 mmHg. The difference between the total fluid infused minus the outflow fluid volume was taken as the fluid deficit. No intravenous fluids were given during the operation. The outflow channel of the resectoscope was connected to a closed-suction unit draining into well calibrated transparent containers. The fluid loss from the vagina was assessed using plastic drapes with graduated marks. Fluid deficit was monitored manually by a dedicated operating room person and the procedure was stopped immediately in cases of fluid deficit exceeding one liter. The goal of the procedure was to restore normalcy of the uterine cavity. Adhesiolysis was performed by making incisions into the avascular adhesions. Flimsy and central adhesions were divided first, followed by marginal and dense adhesions. The procedure was continued in a cephalad direction until the visualization of pink myometrium and tubal ostia.
The mini-resectoscope was used in the second group, henceforth named the MR group. It consists of a 5 mm working element with a sheath and a 2.9 mm, 30° telescope (Karl Storz, Germany) along with compatible Colin’s knife. Cervical dilatation up to Hegar’s dilator size 5 mm was required. The rest of the procedure was done as in conventional hysteroscopic adhesiolysis. Serum electrolytes were checked in all patients 30 minutes before and after the procedure.
The following parameters were recorded in both the groups: 1) cervical dilatation time, 2) operation time, 3) intraoperative complications, 4) postoperative morbidity with respect to time required for hospitalization, ambulation time and postoperative pain, and 5) postoperative complications like cervical stenosis, cervical incompetence or remnant adhesions. Cervical dilatation time was defined as the time from insertion of the first dilator to completion of dilatation (up to 5 mm or 10 mm in the CR and MR group, respectively). Operation time was taken from the time of entry of the resectoscope into the vagina (excludes time required for cervical dilatation) until the completion of the adhesiolysis process and reassessment of the final cavity created. The discomfort experienced by each patient was assessed at 30 minutes and two hours after the end of the procedure. Pain was assessed using the visual analog scale ranging from absence of discomfort/pain to intolerable pain on a scale of 0 to 10. These scores were assessed by a second operator, other than the chief investigator, so as not to influence the assessment.
All patients were discharged on the same day and were advised antibiotics (ciprofloxacin) for five days. Hormonal treatment in the postoperative period has been shown to reduce adhesion reformation in a few studies. Based on our previous experience and further supportive evidence, all patients were given estradiol valerate 4 mg per day for six weeks after surgery.3,14,15 Repeat hysteroscopy was done after six weeks in all cases to assess the normalcy of the uterine cavity or any adhesion reformation. In case of reformation of adhesions, a repeat hysteroscopic adhesiolysis procedure was performed. If the uterine cavity was adequate, patients were advised to try for spontaneous conception. The duration of follow-up for these patients was a minimum of six months. Patients were contacted routinely at monthly intervals and followed-up.
To our knowledge, there is no parallel prospective randomized trial to compare the efficacy of conventional resectoscope and mini-resectoscope in terms of clinical pregnancy rate. However, an earlier study by Sanad and Aboulfotouh indicated that the clinical pregnancy rate among women with subfertility or recurrent pregnancy losses was 65.5% after adhesiolysis.12 Presuming a similar result would be obtained in our study, a sample of size of 90 was considered to be adequate to estimate clinical pregnancy rate with 10% absolute precision level at 5% level of significance. However, to assess the feasibility of such a study, the present pilot study was undertaken with 30 subjects in each group.
Statistical analysis was done using SPSS Statistics (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.). Normality assumptions were tested for all the continuous variables with appropriate statistical test. To test a significant difference between two mean values of continuous variables that followed approximate to normal distribution the Student’s t-independent test was used. Within-group changes in mean values from pre- to post-treatment were compared using the Student’s t-paired test. For non-normal data, median values were compared using the Mann-Whitney U-test. Frequency data across categories was compared either with the chi-squared test or Fisher’s exact test as appropriate. For all the statistical tests a two-tailed probability of p < 0.050 was considered statistically significant.
Results
We included only cases with infertility, of which 39 patients (65.0%) presented with secondary infertility, while 21 (35.0%) had primary infertility. Of the 39 patients with secondary infertility, 17 had history of recurrent abortions. In addition to infertility, menstrual symptoms comprised the presenting symptoms in 30 patients (i.e., hypomenorrhea in 21 patients and amenorrhea in nine patients) [Table 1]. The likely etiological cause for adhesions was suspected to be prior history of curettage (postabortion) in 33 cases (55.0%), history of intrauterine device use in 21 cases (35.0%), previous history of myomectomy in three cases (5.0%). No cause could be determined in the remaining three patients. Previous hysteroscopic adhesiolysis had been attempted in five patients. The participants in the CR group had a mean age of 30.6 years (range 27–38), whereas those in the MR group had a mean age of 28.6 years (range 23–34). There was no significant difference between the groups in the severity of adhesions [Table 1]. Both groups were similar with respect to all other baseline characteristics.
Table 1: Baseline characteristics of the two groups.
|
Age, mean ± SD, years |
30.6 ± 3.0 |
28.6 ± 3.3 |
0.020 |
|
Previous attempt at correction |
2 |
3 |
0.640 |
|
Presenting complaint |
|
|
0.410 |
|
Primary infertility |
9 |
12 |
|
|
Secondary infertility |
21 |
18 |
|
|
History of recurrent pregnancy losses |
9 |
8 |
0.771 |
|
Gravidity, mean ± SD |
1.9 ± 1.4 |
1.4 ± 1.2 |
0.162 |
|
Parity, mean ± SD |
0.3 ± 0.4 |
0.3 ± 0.46 |
1.000 |
|
Menstrual pattern at the time of presentation |
0.270 |
|
Normal menses |
12 |
18 |
|
|
Hypomenorrhea |
12 |
9 |
|
|
Amenorrhea |
6 |
3 |
|
|
Etiological factor |
|
|
0.150 |
|
1 prior curettage |
0 |
3 |
|
|
2 prior curettage |
9 |
9 |
|
|
3 prior curettage |
3 |
3 |
|
|
≥ 4 prior curettage |
3 |
3 |
|
|
Prior cesarean section |
3 |
0 |
|
|
Previous history of myomectomy |
3 |
0 |
|
|
History of intrauterine device use |
9 |
12 |
|
|
Grade of adhesions on hysteroscopy |
0.371 |
|
Minimal |
9 |
6 |
CR: conventional resectoscope; MR: mini-resectoscope; SD: standard deviation.
The time taken for cervical dilatation was less (mean 1.4±1.0 minutes) in the MR group compared to the CR group (2.6±1.1 minutes; p < 0.001). Pain scores 20 minutes after the procedure were significantly lower in the MR group compared to the CR group [Table 2]. Pain scores at two hours were also lower in the MR group compared to the CR group; however, the value failed to reach statistical significance. In seven cases in the CR group, the surgeon encountered difficulty in cervical dilatation. Of these, four patients developed scope entry-related complications (three patients developed cervical lacerations, and one patient had a uterine perforation). In the patient developing uterine perforation during scope entry in the CR group, surgery was abandoned and adhesiolysis could not be done in that sitting. The patient was given oral estrogen therapy for six weeks. Hysteroscopic adhesiolysis was done at a second sitting for this patient with the conventional resectoscope and results of this surgery were recorded and analyzed. In the MR group, there was subjective difficulty in dilatation in two cases. Both were associated with adhesions at the internal os. There were no complications related to the introduction of the scope in the MR group (p = 0.112) [Table 2].
There were no complications related to anesthesia in either group. There was no significant difference in the mean fluid deficit or the mean postoperative sodium levels between the two groups. On relook hysteroscopy at six weeks follow-up, two cases in the CR group and three in the MR group were found to have remnant adhesions and underwent hysteroscopic adhesiolysis in the same sitting. Another hysteroscopy was repeated for these five cases after two months, which showed flimsy adhesions in one case in the CR group and was broken successfully with the hysteroscope itself. The remaining four cases showed a normal cavity.
Table 2: Operative outcomes.
|
Cervical dilatation time, minutess |
2.6 ± 1.1 |
1.4 ± 1.0 |
< 0.001 |
|
Operation time, minutess |
17.0 ± 2.5 |
16.1 ± 2.3 |
0.140 |
|
Postoperative pain score at 30 minutes |
8.5 ± 0.5 |
7.8 ± 0.7 |
< 0.001 |
|
Postoperative pain score at 2 hours |
4.3 ± 0.7 |
4.0 ± 0.6 |
0.110 |
CL: cervical laceration; UP: uterine perforation; CR: conventional resectoscope; MR: mini-resectoscope; SD: standard deviation.
*p-value based on Fisher’s exact test. Other p-values were based on Student’s t-independent test.
After the surgery, all amenorrheic patients (n = 9) in both groups resumed menstruation. Out of the total 21 cases with hypomenorrhea, 12 cases (57.1%) started having normal menstrual flow following surgery. However, nine cases continued to have hypomenorrhea [Table 3]. Sixteen patients were able to conceive following the surgery (seven in the CR group and nine in the MR group). This included nine term pregnancies, three ongoing pregnancies, one ectopic pregnancy, and three abortions. There was no case of cervical incompetence or preterm delivery. The two groups did not show a statistical difference in their menstrual and reproductive outcome.
Table 3: Outcome parameters following adhesiolysis.
|
Resolution of amenorrhea postsurgery |
6/6 (100) |
3/3 (100) |
1.000 |
|
Resumption of normal menses in hypomenorrheic patients |
6/12 (50.0) |
6/9 (66.7) |
0.660 |
|
Remnant adhesions on relook hysteroscopy |
2/30 (6.7) |
3/30 (10.0) |
0.990 |
|
Total conceptions |
7/30 (23.3) |
9/30 (30.0) |
0.560 |
|
Term pregnancy |
3/30 (10.0) |
6/30 (20.0) |
0.470 |
|
Ongoing pregnancy |
1/30 (3.3) |
2/30 (6.7) |
0.990 |
|
Ectopic pregnancy |
0/30 (0.0) |
1/30 (3.3) |
0.990 |
CR: conventional resectoscope; MR: mini-resectoscope.
Discussion
To date, there are no randomized trials available comparing the conventional larger diameter (9 mm) resectoscope to the new mini-resectoscope looking at the efficacy, complications, and long-term effect on fertility potential after hysteroscopic adhesiolysis. Reducing the diameter of hysteroscopes by 1–2 mm, decreases its size by 50% and 75%, respectively, leading to a considerable difference in the ease of insertion and also reduces the pain of the
procedure significantly.16
We encountered difficulty in cervical dilatation in seven cases in the CR group versus only two cases in the MR group. Dilatation required in the MR group was up to 5 mm, compared with 10 mm dilatation in the CR group. The pain scores of the patients calculated 30 minutes after surgery were significantly less in the MR group compared with the CR group.
There were no complications during entry of the resectoscope (e.g., cervical trauma or uterine perforation) in the MR group compared with four cases in the CR group. Smaller diameter scopes can counteract difficulties encountered during the hysteroscope introduction. This is especially important in cases of intrauterine adhesions, which can be associated with fibrosis at the cervical canal and have a narrow cavity, and thus are known to be associated with higher chances of uterine perforation. The cervical dilatation time was also significantly less in the MR group.
Another study also demonstrated that with mini-hysteroscopy, surgeon experience is less important for the success and acceptability of the procedure.17,18 The use of mini-resectoscope was suggested by the authors, especially for less experienced surgeons and in cases where dilatation and approach to the uterine cavity is expected to be difficult.17 Certain doubts were raised initially about the vision with the mini-hysteroscope, due to the smaller size of the lens. However, numerous studies have shown the vision of diagnostic office hysteroscopy to be comparable to that of the larger diameter hysteroscopes owing to the high quality of the rod-lens system of the mini-resectoscope.16 In our study, the surgeon did not face any problem in the visualization and found the image quality of the two systems to be similar.
Risk of reformation of intrauterine synechiae after surgery is a concern. Most authors have suggested evaluation of the endometrial cavity after surgery for remnant adhesions after six to eight weeks. Transvaginal sonography preferably three-dimensional or hysterosalpingography, or a second-look hysteroscopy, can be performed for this purpose. In our study, a second-look hysteroscopy was done to evaluate the cavity after six weeks which allows excision of the remnant adhesions during the same procedure. Numerous modalities are in use to prevent postoperative adhesion formation, such as fluid agents (seprafilm, hyaluronic acid), mechanical agents (intrauterine device), and postoperative hormonal treatment (estroprogestative treatment).17,18 However, none have been shown to prevent adhesions or improve the reproductive outcome.17–19 Hormonal therapy with estradiol valerate was used in our study for this purpose. Estrogens help by inducing endometrial growth when used alone or in combination
with progesterone.2
There was an improvement in the menstrual outcome in both groups after surgery (68.7%). All patients with amenorrhea resumed menses. Similarly, other studies have shown an improvement in menstrual outcome in 60–100% of women postsurgery.12,20–22 Out of the total 60 infertile cases, 26.7% conceived; 56.2% of these had a successful pregnancy outcome. There was no statistically significant difference between the two groups. Likewise, Chen et al,23 observed a conception rate of 48.2% among women undergoing hysteroscopic adhesiolysis at their center in China, with a live birth rate of 85.6%. In a systematic review of 28 studies, the pregnancy rate ranged from 12.5% to 100%, with the majority of studies showing a pregnancy rate of 40.9% to 66.67%.24
Studies have reported good results of outpatient hysteroscopic polypectomy with mini-resectoscope, avoiding the need for general or regional anesthesia.25,26 However, in our experience, cases of intrauterine adhesions require cervical dilatation and dilatation is often difficult. Hence, general anesthesia was administered in our study. A prospective study was conducted by Sanad and Aboulfotouh, assessing the efficacy of the mini-resectoscope for hysteroscopic adhesiolysis under general anesthesia in 61 patients with infertility or recurrent pregnancy losses.12 They reported a significant improvement in menstrual outcome in 60.7% of patients complaining of amenorrhea/hypomenorrhea. They reported a change in the pregnancy rate from 18% presurgery to 65.5% postsurgery, and the live birth rate was 36%.12
A recent Cochrane review evaluating the effectiveness of the hysteroscopic treatment of various intrauterine pathologies (intrauterine adhesions, endometrial polyps, submucous fibroids or uterine septum) in women with subfertility, concluded that further randomized studies are needed to provide definite evidence.27
To the best of our knowledge, our study is the only study so far in which the conventional larger diameter resectoscope has been compared with the mini-resectoscope for hysteroscopic adhesiolysis. Our study was a randomized, prospective study and we were able to rule out all other factors which could have caused infertility or menstrual problems. Extensive follow-up data was collected for all patients, regarding the effect on the menstrual and reproductive parameters.
Conclusion
Our study has further supported hysteroscopic adhesiolysis with the mini-resectoscope, showing comparable efficacy to conventional resectoscope in terms of the menstrual and reproductive outcome, good vision, ease of entry of the resectoscope, and significantly reduced operative morbidity. Further, larger randomized studies with high quality data comparing conventional resectoscope and mini-resectoscope are required for more
definitive evidence.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
references
- 1. Yu D, Wong Y-M, Cheong Y, Xia E, Li T-C. Asherman syndrome–one century later. Fertil Steril 2008 Apr;89(4):759-779.
- 2. Schenker JG, Margalioth EJ. Intrauterine adhesions: an updated appraisal. Fertil Steril 1982 May;37(5):593-610.
- 3. Advancing Minimally Invasive Gynecology Worldwide AA; AAGL Advancing Minimally Invasive Gynecology Worldwide. AAGL practice report: practice guidelines for management of intrauterine synechiae. J Minim Invasive Gynecol 2010 Jan-Feb;17(1):1-7.
- 4. Valle RF, Sciarra JJ. Intrauterine adhesions: hysteroscopic diagnosis, classification, treatment, and reproductive outcome. Am J Obstet Gynecol 1988 Jun;158(6 Pt 1):1459-1470.
- 5. March CM, Israel R, March AD. Hysteroscopic management of intrauterine adhesions. Am J Obstet Gynecol 1978 Mar;130(6):653-657.
- 6. Marsh FA, Rogerson LJ, Duffy SR. A randomised controlled trial comparing outpatient versus daycase endometrial polypectomy. BJOG 2006 Aug;113(8):896-901.
- 7. Cooper NA, Smith P, Khan KS, Clark TJ. Vaginoscopic approach to outpatient hysteroscopy: a systematic review of the effect on pain. BJOG 2010 Apr;117(5):532-539.
- 8. Bettocchi S, Ceci O, Nappi L, Di Venere R, Masciopinto V, Pansini V, et al. Operative office hysteroscopy without anesthesia: analysis of 4863 cases performed with mechanical instruments. J Am Assoc Gynecol Laparosc 2004 Feb;11(1):59-61.
- 9. Cicinelli E, Parisi C, Galantino P, Pinto V, Barba B, Schonauer S. Reliability, feasibility, and safety of minihysteroscopy with a vaginoscopic approach: experience with 6,000 cases. Fertil Steril 2003 Jul;80(1):199-202.
- 10. van Kerkvoorde TC, Veersema S, Timmermans A. Long-term complications of office hysteroscopy: analysis of 1028 cases. J Minim Invasive Gynecol 2012 Jul-Aug;19(4):494-497.
- 11. Bougie O, Lortie K, Shenassa H, Chen I, Singh SS. Treatment of Asherman’s syndrome in an outpatient hysteroscopy setting. J Minim Invasive Gynecol 2015 Mar-Apr;22(3):446-450.
- 12. Sanad AS, Aboulfotouh ME. Hysteroscopic adhesiolysis: efficacy and safety. Arch Gynecol Obstet 2016 Aug;294(2):411-416.
- 13. National Collaborating Centre for Women’s and Children’s Health (UK). Fertility: Assessment and Treatment for People with Fertility Problems. London: Royal College of Obstetricians & Gynaecologists. 2013 [cited 2017 Mar 19]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK247932/.
- 14. Practice Committee of American Society for Reproductive Medicine. Current evaluation of amenorrhea. Fertil Steril 2008 Nov;90(5)(Suppl):S219-S225.
- 15. Munro MG, Critchley HO, Broder MS, Fraser IS; FIGO Working Group on Menstrual Disorders. FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. Int J Gynaecol Obstet 2011 Apr;113(1):3-13.
- 16. Cicinelli E. Diagnostic minihysteroscopy with vaginoscopic approach: rationale and advantages. J Minim Invasive Gynecol 2005 Sep-Oct;12(5):396-400.
- 17. Tonguc EA, Var T, Yilmaz N, Batioglu S. Intrauterine device or estrogen treatment after hysteroscopic uterine septum resection. Int J Gynaecol Obstet 2010 Jun;109(3):226-229.
- 18. Thubert T, Dussaux C, Demoulin G, Rivain A-L, Trichot C, Deffieux X. Influence of auto-cross-linked hyaluronic acid gel on pregnancy rate and hysteroscopic outcomes following surgical removal of intra-uterine adhesions. Eur J Obstet Gynecol Reprod Biol 2015 Oct;193:65-69.
- 19. Roy KK, Negi N, Subbaiah M, Kumar S, Sharma JB, Singh N. Effectiveness of estrogen in the prevention of intrauterine adhesions after hysteroscopic septal resection: a prospective, randomized study. J Obstet Gynaecol Res 2014 Apr;40(4):1085-1088.
- 20. Chen FP, Soong YK, Hui YL. Successful treatment of severe uterine synechiae with transcervical resectoscopy combined with laminaria tent. Hum Reprod 1997 May;12(5):943-947.
- 21. Al-Inany H. Intrauterine adhesions. An update. Acta Obstet Gynecol Scand 2001 Nov;80(11):986-993.
- 22. Yu D, Li T-C, Xia E, Huang X, Liu Y, Peng X. Factors affecting reproductive outcome of hysteroscopic adhesiolysis for Asherman’s syndrome. Fertil Steril 2008 Mar;89(3):715-722.
- 23. Chen L, Zhang H, Wang Q, Xie F, Gao S, Song Y, et al. Reproductive Outcomes in Patients With Intrauterine Adhesions Following Hysteroscopic Adhesiolysis: Experience From the Largest Women’s Hospital in China. J Minim Invasive Gynecol 2017 Feb;24(2):299-304.
- 24. Johary J, Xue M, Zhu X, Xu D, Velu PP. Efficacy of estrogen therapy in patients with intrauterine adhesions: systematic review. J Minim Invasive Gynecol 2014 Jan-Feb;21(1):44-54.
- 25. Dealberti D, Riboni F, Cosma S, Pisani C, Montella F, Saitta S, et al. Feasibility and Acceptability of Office-Based Polypectomy With a 16F Mini-Resectoscope: A Multicenter Clinical Study. J Minim Invasive Gynecol 2016 Mar-Apr;23(3):418-424.
- 26. Dealberti D, Riboni F, Prigione S, Pisani C, Rovetta E, Montella F, et al. New mini-resectoscope: analysis of preliminary quality results in outpatient hysteroscopic polypectomy. Arch Gynecol Obstet 2013 Aug;288(2):349-353.
- 27. Bosteels J, Kasius J, Weyers S, Broekmans FJ, Mol BW, D’Hooghe TM. Hysteroscopy for treating subfertility associated with suspected major uterine cavity abnormalities. Cochrane Database Syst Rev 2015 Feb;(2):CD009461.