| How to cite this article
Zayyan M, Suhyb SR, Laurel NO'C. The Use of Total Cervical Occlusion along with McDonald Cerclage in Patientswith Recurrent Miscarriage or Preterm Deliveries. Oman Med J 2012 Jan; 27(1):63-65.
How to cite this URL
Zayyan M, Suhyb SR, Laurel NO'C. The Use of Total Cervical Occlusion along with McDonald Cerclage in Patientswith Recurrent Miscarriage or Preterm Deliveries. Oman Med J 2012 Jan; 27(1):63-65. Available from http://www.omjournal.org/fultext_PDF.aspx?DetailsID=199&type=fultext
Abstract
Objectives: To study the fetal outcome with the use of McDonaldcerclage and total cervical occlusion in women with recurrentmid-trimester miscarriages or preterm deliveries, as well ascomplications of total cervical occlusion in the women.
Methods: Prospective descriptive observational study on patientswith two or more mid-trimester miscarriages, deliveries before 36weeks, or patients who have experienced failure of transvaginalcerclage.
Results: Twenty-six women were studied. Of these, 92% deliveredat term. Two women delivered at 33 and 35 weeks, respectively.There was one neonatal death. Take home baby rate was 96.2%.There was no serious maternal morbidity among the patients.
Conclusion: The addition of external cervical OS occlusion toMcDonald cerclage could improve fetal outcome in women withrecurrent mid-trimester miscarriages and preterm deliveries.
Keywords: Total cervical occlusion; McDonald cerclage;Recurrent mid-trimester miscarriage; Preterm delivery.
Introduction
Recurrent miscarriage is a distressful condition and recurrentmid-trimester miscarriage in particular is disturbing to physicianand patient alike, because the loss is that of a normal fetus inadvancing stages of gestation. This form of miscarriage andpreterm births appear to have similar etiologies, which includecervical weakness and/or ascending infection.1,2,3,4,5
Cervical weakness is often over-diagnosed as a cause of midtrimestermiscarriage. There is also no satisfactory objectivetest that can identify women with cervical weakness in the nonpregnantstate.6 Even though transvaginal ultrasound assessmentof the cervix during pregnancy has been found to be useful inpredicting preterm birth in some cases of suspected cervicalweakness,3 treatment of cervical incompetence with cervicalcerclage may not actually result in improved perinatal survival.7,8 Furthermore, meta analysis of trials on McDonald cerclage havefailed to show a lower rate of preterm delivery before 28 and 34 weeks in women assigned to cervical cerclage.4,6
These body of evidence point to probably more than just cervicalweakness as a cause of late trimester miscarriage and pretermbirths.8-11 Ascending infection may be an important contributoryfactor to mid-trimester miscarriage and preterm delivery.9-11 The evidence for this is the high frequency of finding organisms in theamniotic fluid which are also present in the vagina in patients withpreterm labor.11-13 Infection from the vagina may be as a result ofloss of the protective cervical mucus plug (the operculum), whichserves as an effective mechanical barrier between the vagina andthe uterus and protects the feto-maternal unit from ascendinginfection during pregnancy.14,15
The essence of total cervical occlusion is to preserve the cervicalmucus plug and prevent ascending infection and subsequentinitiation of miscarriage and preterm birth. The use of cervicalocclusion along with McDonald cerclage is presented in 26 patients in this study. Both procedures are simple and technicallyeasy to perform.
Methods
This is a prospective observational study conducted over a periodof twenty months on all patients presenting with recurrent midtrimestermiscarriage or delivery before 36 weeks to a privateobstetric facility that serves as a referral center for obstetric andgynecologic cases in Kaduna Nigeria between 1st April 2008 and 31st December 2009. Patients with two previous miscarriages inmid-trimester or preterm delivery who had agreed to participatein the trial between 1st April 2008 and 31st December 2009 wereincluded in the study. Patients had a history of two consecutivemid-trimester miscarriages or delivery before 36 weeks, andpatients who have previously had a McDonald’s or Shirodkar’scerclage with suboptimal results. This is defined as delivery before36 weeks gestation despite the cerclage.
The inclusion criteria was as follows: 1) At least two previousmid-trimester miscarriages from diagnosed or suspected cervicalweakness; 2) Failed McDonalds or Shirodkar’s cerclage; 3) Nomedical complication in current pregnancy or previous pregnancies; 4) Singleton pregnancy with normal fetus on ultrasound scans; 5) Consent to participate in the study. While the exclusion criteria forthis study included the following: 1) Vaginal discharge, rupturedor bulging membranes; 2) Medical disorder in current or previouspregnancy including HIV; 3) Bleeding in early pregnancy; and 4)Fetal anomaly.
Eligible patients had a transvaginal ultrasound scan done toconfirm cervical length of less than 2.5 cm or internal OS diameterof 0.8 cm or more in the current pregnancy. A McDonald cerclagewas performed with merselene tape under general anesthetic at thelevel of the internal cervical OS (as described by McDonalds),16 and total external cervical OS occlusion was performed with nylon 2/0 or 3/0 ethicon suture on a curved needle between 13 and 16weeks of gestation.
The cervical occlusion was placed transversely along theexternal cervical OS below the McDonalds suture to occludeexternal cervical OS using the anterior and posterior lips of thecervix with the nylon suture, (Fig. 1). The external cervical OS is totally occluded in continuous nylon suture starting from oneend to the other. The suture was tied and left long enough tofacilitate removal. Routine postoperative care using salbutamoland prophylactic antibiotics were given.
The patients were discharged as appropriate and routineantenatal care continued. At 37 weeks of gestation or with theonset of labor if earlier, both sutures were removed and the patientswere allowed to deliver as appropriate. The maternal outcome interms of infection, hemorrhage, trauma difficulty with removalor increased operative delivery and fetal outcome in terms of fetalweight and perinatal survival were observed and data is analyzedusing simple frequency tables.
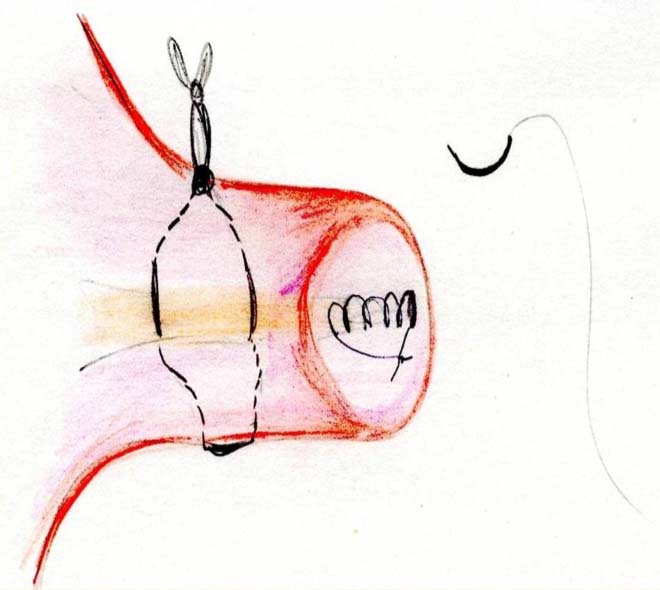
Figure 1: Diagram to show method of double cerclage. McDonald’sand total cervical occlusion.
Results
Twenty-six patients who fulfilled the criteria were followed up tothe time of delivery. The age range of the patients was 23 to 36 yearswith a mean age of 26.8 years. The patients have had fetal wastageof between two to eight with an average of four mid-trimesterlosses in the group. The profiles of the patients are presented in Tables 1 and 2.
Failed cervical cerclage in a previous pregnancy was observedin 6 out of 26 patients (23.8%). There were three patients whohad more than one failed cervical cerclage, including one withthree-failed cervical suture with subsequent fetal loss. However, there were no intra or postoperative complications in terms ofhemorrhage, infection, or ruptured membranes. Though, one patient who was delivered by cesarean section presented withincompletely removed nylon suture two weeks after discharge.
In terms of the mode of delivery; 22 patients had normal vaginal delivery, while two patients had vacuum delivery and two had cesarean sections. The indications for the cesarean section were two previous cesarean sections in one patient, and poor progress inlabor for the other patient. With regards to fetal outcome; 25 ofthe total 26 patients (96.2%) took their babies home. Overall, 24(92.3%) patients delivered at term, while two patients delivered at33 and 35 weeks respectively; one following spontaneous ruptureof membranes at 33 weeks and the other with preterm labor at 35 weeks. The fetus delivered at thirty three weeks died after 48 hours from respiratory distress. This loss, 1 in 26 patients (3.8%)was the only fetal wastage observed. In this study, there was no extreme low birth weight as all the babies weighed greater than 1.5 kg. The baby delivered at 33 weeks weighed 1.9 kg. Over 80% of the patients had normal birth weight for the area of study.
Table 1: Age of Patients with Recurrent Miscarriage.
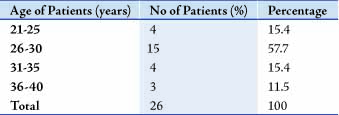
Table 2: Number of Miscarriages Experienced by the Patients.
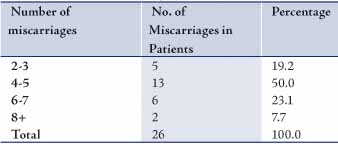
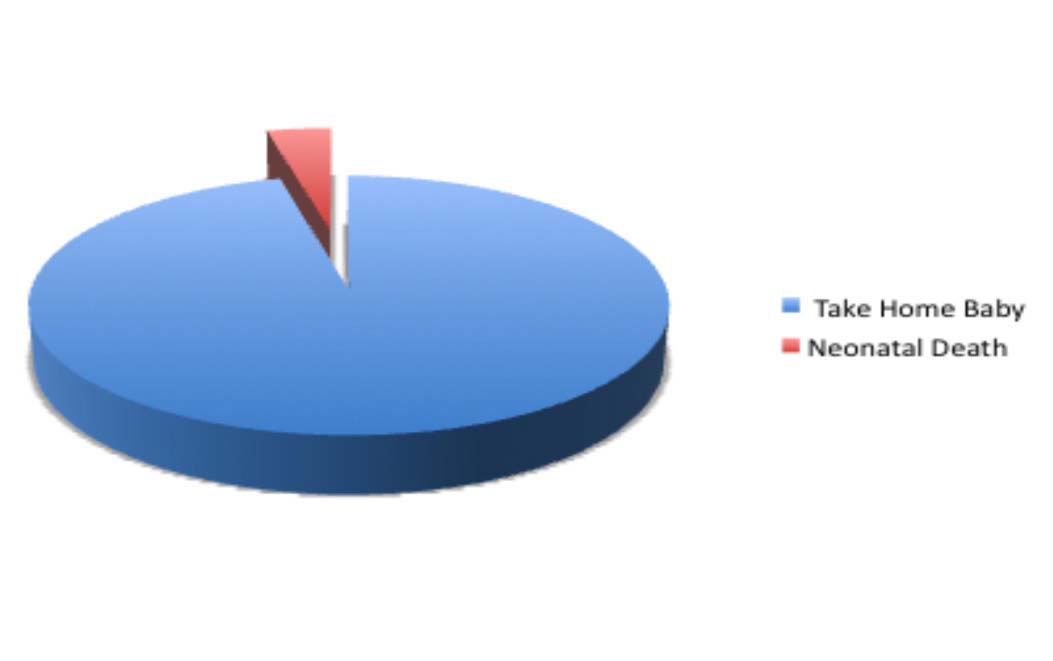
Figure 2: Fetal Outcome at Delivery
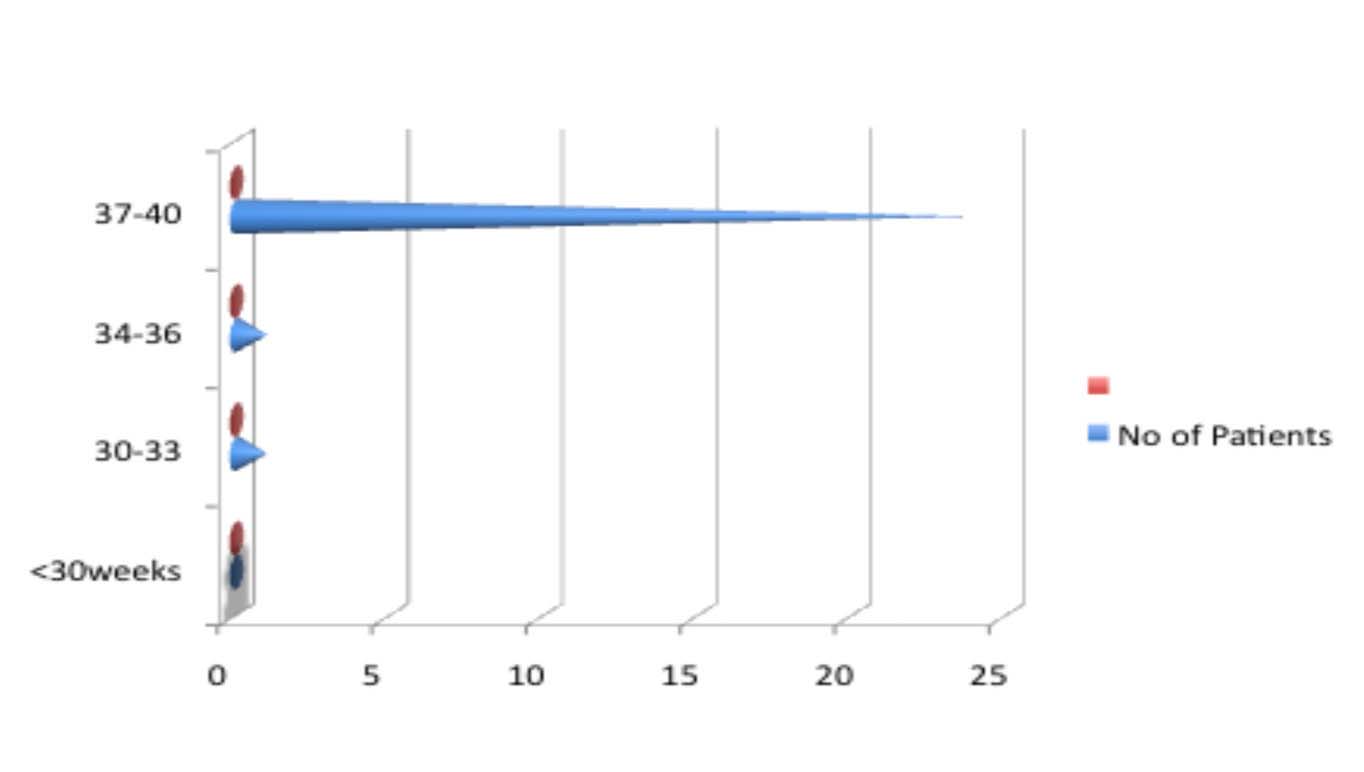
Figure 3: Gestational age at time of delivery following use ofMcDonald with Cervical Occlusion.
Discussion
The use of early total cervical occlusion (ETCO) was introduced in 1980 but has not been popularized until of recent, whenten countries participated in a randomized controlled trial toevaluate its effectiveness.17,18 In this study, which is a prospective observational study of 26 patients who had both McDonald cerclage and early total cervical occlusion; there was only one delivery at 33 weeks and eventual fetal loss. The success rate of 96.2% is superiorto 89% observed from performing a trans-abdominal cerclage.19,20 This is especially important if the simplicity of the procedure and the ability of the patients to achieve normal delivery are taken into consideration. The observed cesarean section rate of 7.7% is in keeping with normal rate for the unit of 10%.
Furthermore, 23.8% of the patients reported here had failed transvaginal cerclage in their previous pregnancies, but subsequently delivered at term following the addition of total cervical occlusion to McDonald cerclage. There was no significant postoperative morbidity observed in this study, which is similar to the findings observed in studies involving larger numbers of patients.18 Also, cervical scarring was not observed in any of the patients. If other studies continue to support these results, then the role of retaining the cervical mucus plug in preventing mid trimester pregnancy loss and preterm delivery will be not only be substantiated, but two simple vaginal procedures could be used toimprove pregnancy outcome.
Conclusion
The addition of total cervical occlusion to transvaginal cerclage has improved fetal outcome in patients with recurrent pregnancy without increasing maternal morbidity or cesarean section rate.
Acknowledgements
We acknowledge Dr. Dee Mc Cormack’s instructions from Prof. Secher who introduced us to this procedure (with illustrativediagram). No conflicts of interest to declare.
References
1. Romero R, Espinoza J, Mazor M. Can endometrial infection/inflammationexplain implantation failure, spontaneous abortion, and preterm birth afterin vitro fertilization? Fertil Steril 2004 Oct;82(4):799-804.
2. Owen J, Yost N, Berghella V, Thom E, Swain M, Dildy GA III, et al; NationalInstitute of Child Health and Human Development, Maternal-FetalMedicine Units Network. Mid-trimester endovaginal sonography in womenat high risk for spontaneous preterm birth. JAMA 2001 Sep;286(11):1340-1348.
3. Macdonald R, Smith P, Vyas S. Cervical incompetence: the use oftransvaginal sonography to provide an objective diagnosis Utrasound. ObstetGynecol 2001 Sep;18(3):211-216.
4. Althuisius SM, Dekker GA, van Geijn HP, Bekedam DJ, Hummel P. Cervicalincompetence prevention randomized cerclage trial (CIPRACT): studydesign and preliminary results. Am J Obstet Gynecol 2000 Oct;183(4):823-829.
5. Rust OA, Atlas RO, Jones KJ, Benham BN, Balducci J. A randomized trialof cerclage versus no cerclage among patients with ultrasonographicallydetected second-trimester preterm dilatation of the internal os. Am J ObstetGynecol 2000 Oct;183(4):830-835.
6. MRC/RCOG Working Party on Cervical Cerclage. Final report ofthe Medical Research Council/Royal College of Obstetricians andGynaecologists multicentre randomised trial of cervical cerclage. Br J ObstetGynaecol 1993 Jun;100(6):516-523.
7. Harger JH. Cerclage and cervical insufficiency: an evidence-based analysis.Obstet Gynecol 2002 Dec;100(6):1313-1327.
8. Rust OA, Atlas RO, Reed J, van Gaalen J, Balducci J. Revisiting the shortcervix detected by transvaginal ultrasound in the second trimester: whycerclage therapy may not help. Am J Obstet Gynecol 2001 Nov;185(5):1098-1105.
9. Berghella V, Odibo AO, To MS, Rust OA, Althuisius SM. Cerclage for shortcervix on ultrasonography: meta-analysis of trials using individual patientleveldata. Obstet Gynecol 2005 Jul;106(1):181-189.
10. Althuisius S, Dekker G. Controversies regarding cervical incompetence,short cervix, and the need for cerclage. Clin Perinatol 2004 Dec;31(4):695-720, v-vi.
11. Minkoff H. Prematurity: infection as an etiologic factor. Obstet Gynecol1983 Aug;62(2):137-144.
12. Romero R, Mazor M, Wu YK, Sirtori M, Oyarzun E, Mitchell MD, etal. Infection in the pathogenesis of preterm labor. Semin Perinatol 1988Oct;12(4):262-279.
13. Romero R, Sirtori M, Oyarzun E, Avila C, Mazor M, Callahan R, et al.Infection and labor. V. Prevalence, microbiology, and clinical significance ofintraamniotic infection in women with preterm labor and intact membranes.Am J Obstet Gynecol 1989 Sep;161(3):817-824.
14. Cassell GH, Davis RO, Waites KB, Brown MB, Marriott PA, Stagno S,et al. Isolation of Mycoplasma hominis and Ureaplasma urealyticum fromamniotic fluid at 16-20 weeks of gestation: potential effect on outcome ofpregnancy. Sex Transm Dis 1983 Oct-Dec;10(4)(Suppl):294-302.
15. Gray DJ, Robinson HB, Malone J, Thomson RB Jr. Adverse outcome inpregnancy following amniotic fluid isolation of Ureaplasma urealyticum.Prenat Diagn 1992 Feb;12(2):111-117.
16. Secher NJ, McCormack CD, Weber T, Hein M, Helmig RB. Cervicalocclusion in women with cervical insufficiency: protocol for a randomised,controlled trial with cerclage, with and without cervical occlusion. BJOG2007 May;114(5):1-6.
17. Hein M, Valore EV, Helmig RB, Uldbjerg N, Ganz T. Antimicrobial factorsin the cervical mucus plug. Am J Obstet Gynecol 2002 Jul;187(1):137-144.
18. McDonald, I. A.: Suture of the cervix for inevitable miscarriage. J. Obstet. &Gynaecol. Brit. C’wlth., 1957, 64:346-350.
19. Saling E, Schumacher E. Total surgical cervical occlusion. Conclusionsfrom data of several clinica, which use total surgical cervical occlusion. ZGeburtshilfe Neonatol 1996 May-Jun;200(3):82-87.
20. Saling E, Schumacher E. Results of follow-up of mothers with previoussurgical “total cervical cerclage” also with reference to neonatal dataGeburtshilfe Neonatol. Jul-1997 Aug; 201(4):122-7.
|