A 40-year-old Omani female presented with history of bilateral loin pain with no urinary symptoms. On examination, she had epigastric tenderness, but an otherwise normal examination. Ultrasound of the urinary tract was unremarkable; however, a sizable mass was incidentally noted. Subsequently, a computed tomography (CT) scan was performed [Figure 1].
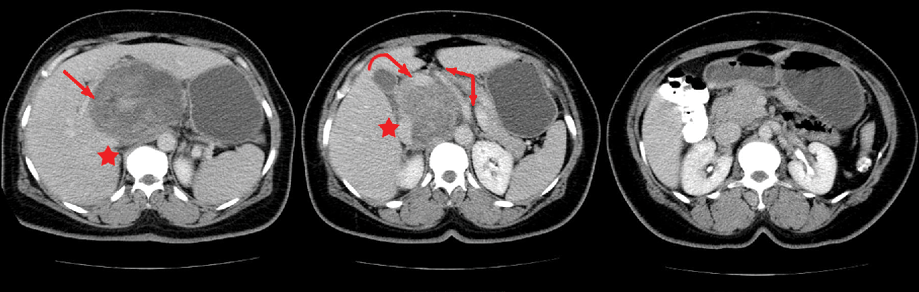
Figure 1: Contrast-enhanced CT scan revealed a sizable heterogeneous complex mass (long arrow) with cystic and solid components that was centered upon the porta hepatis reaching the retroperitoneum. It was seen intimately related to major vessels; the celiac trunk with hepatic artery (two-headed arrow) antero-medially and the portal vein (curved arrow) anteriorly. The inferior vena cava (IVC) (star) was seen attenuated posterolaterally.
Question
What is the most likely diagnosis?
- Gastrointestinal stromal tumor (GIST)
- Liposarcoma
- Lymphoma
- Retroperitoneal leiomyosarcoma
- Malignant fibrous histiocytoma
Answer
d. Retroperitoneal leiomyosarcoma
Discussion
Retroperitoneal leiomyosarcoma (LMS) is considered the second most common primary retroperitoneal malignancy (after liposarcoma).1 It occurs during the fifth to sixth decades of life with a male/female ratio of 1:6. It originates from retroperitoneal space without attachment to organs or from the wall of inferior vena cava (IVC).1 Clinically, it may represent with abdominal mass, pain, weight loss, nausea, vomiting, abdominal distension, change in defecation habits, leg edema, back or radicular pain, and frequent urination.1 Retroperitoneal leiomyosarcomas are typically well-circumscribed with a mean diameter of 16 cm, and often contain intratumoral necrosis and hemorrhage. Histologically, a typical pattern of interlacing, sweeping bundles of elongated spindle-shaped cells, and blunt-ended nuclei can be seen.2
Initially, adjacent structures are displaced, but direct extension may occur later.
Distant metastases occur in less than half of patients
(typically to the liver, lungs, brain, and peritoneum), and are frequently hematogenous.
On CT and magnetic resonance imaging (MRI), leiomyosarcomas usually have attenuation similar to muscle, being of low to intermediate signal intensity on T1-weighted imaging, and heterogeneous intermediate to high signal intensity on T2-weighted imaging.3 Central breaking down is common and seen as foci with low attenuation on CT while on MRI it appears of low signal on T1-weighted image with high T2-weighted signal intensity. Fat and calcification are not typical findings. The enhancement of leiomyosarcomas is usually delayed compared to the enhancement of the surrounding skeletal muscles.3
The main differential diagnosis includes liposarcoma, malignant fibrous histiocytoma, and lymphoma.1
Complete surgical removal is the treatment of choice for retroperitoneal leiomyosarcoma.3 Retroperitoneal leiomyosarcomas have a poor prognosis.4 Many patients have unresectable disease at the time of presentation secondary to infiltration of the intrahepatic IVC, hepatic veins, right atrium, or metastatic disease.4 Local recurrence after resection was seen in 40-77% of patients.
Disclosure
No conflicts of interest, financial or otherwise, were declared by the authors.
references
- 1. Dahnert WF. Urogenital Tract Radiology Review Manual. 6th Ed. Lippincott Williams & Wilkins. 2007 [cited December 2015]. Available from http://www.msdlatinamerica.com.
- 2. Dalainas I. Vascular smooth muscle tumors: Review of the literature. International Journal of Surgery, 2008 Apr; 6(2):157-163.
- 3. Hamm B, Ros PR, editors. Abdom Imaging. Volume 1. Springer-Verlag: Berlin Heidelberg; 2013.
- 4. Elsayes KM, editor. Cross-Sectional Imaging of the Abdomen and Pelvis: A Practical Alogarithmic Approach. Springer-Verlag: New York; 2015.