The parapharyngeal space (PPS) is a potential space located lateral to the upper pharynx. This space extends from the skull base to the hyoid bone. The three main groups of primary tumors of this space are salivary gland tumors, neurogenic tumors, and paragangliomas. The most common group is the salivary gland tumor.
Pleomorphic adenoma is the most common salivary gland tumor of PPS and due to their slow growth can remain undetected for a long time. Clinical symptoms usually start appearing when the tumor size reaches > 2.5–3.0 cm.1 Clinical manifestations include gradually increasing painless mass in the neck and/or in the oropharynx (causing dysphagia, hoarseness, obstructive sleep apnea2–4) and, rarely, difficulty breathing.5,6 With the advent of cross-sectional imaging studies incorporated along with guided fine needle aspiration cytology (FNAC), interpretation of the nature of these PPS lesions have proved to be helpful.7 Complete surgical excision is the mainstay of treatment for PPS pleomorphic adenoma and various surgical approaches have been described.
Here we report a case of giant PPS pleomorphic adenoma, presented as acute airway obstruction with stridor.
Case report
A 60-year-old male patient was admitted to the emergency department with chief complaints of increased difficulty breathing for five days leading to acute respiratory distress in the last 24 hours. The patient was unable to maintain oxygen saturation level and, hence, an emergency tracheostomy was performed in view of acute respiratory obstruction and stridor. Once the patient was stable, he was further evaluated for the cause of respiratory distress.
History revealed a mass in the oral cavity and difficulty swallowing since two years, and difficulty in breathing since one year with rapid progression since last one month. On oral examination, a huge bulge was seen over the soft palate pushing the uvula right and completely obliterating the oropharyngeal isthmus [Figure 1]. On neck examination, a
4 × 3 cm oval swelling was seen on the left side of the neck below the angle of mandible and extending up to the anterior border of sternocleidomastoid. On palpation, swelling was firm in consistency, non-tender, non-compressible, and non-pulsatile. There was no history of any medical illness. Having made a clinical impression of parapharyngeal mass, contrast computed tomography (CT) scan of the neck showed a large homogeneously enhancing mass lesion in oropharynx and nasopharynx [Figure 2]. FNAC from the neck and intraoral swelling was suggestive of a pleomorphic adenoma. After complete evaluation, surgical excision of the tumor was planned. The transcervical approach was used to gain access to the left parapharyngeal space, and the tumor was removed successfully in toto. The tumor size was measured 10 × 8.2 × 5.8 cm. Histopathology of the surgical specimen confirmed the diagnosis of pleomorphic adenoma [Figure 3]. The postoperative period was uneventful, and the tracheostomy site was closed after two weeks. The patient remained disease-free on one-year follow-up.

Figure 1: Tracheostomized patient with oropharyngeal bulge.
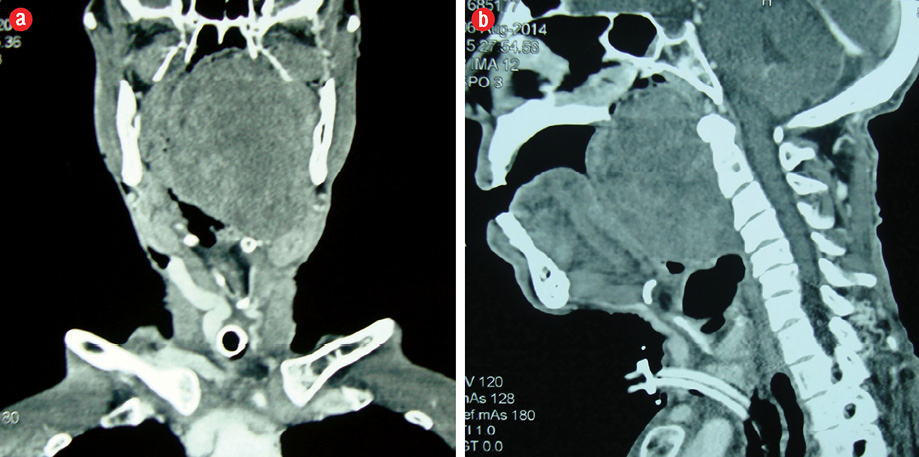
Figure 2: (a) Coronal and (b) sagittal plane computed tomography showing a large mass in the left parapharyngeal space compressing the oropharyngeal airway.
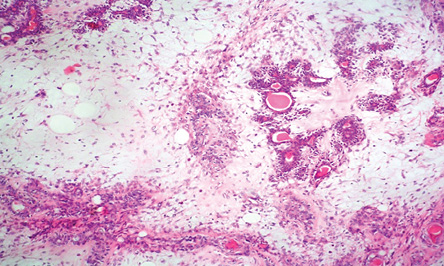
Figure 3: Microphotography showing pleomorphic adenoma. Hematoxylin and eosin stain, magnification = 40 ×.
Discussion
Pleomorphic adenoma of the minor salivary glands is commonly found in the palate followed by the lip, buccal mucosa, floor of mouth, tongue, tonsil, pharynx, retromolar area, and nasal cavity. Pleomorphic adenoma in PPS typically occurs in the deep lobe of the parotid, but rarely can develop de novo from the minor salivary gland and displaced or aberrant salivary gland tissue within a lymph node.8
In our patient, the de novo occurrence of pleomorphic adenoma is either from displaced or aberrant salivary gland tissue in PPS. The classical presentation of a benign PPS tumor is a painless submucosal swelling in the lateral pharyngeal wall with or without extension to retromandibular groove.9 As tumors enlarge, they may present with hoarseness, dysphagia, dysarthria, Horner’s syndrome,9 or with symptoms of obstructive sleep apnea.2–4 There are only two cases reported in literature worldwide who presented with acute respiratory obstruction and required tracheostomy as seen in our case.5,6
FNAC is the preferred diagnostic modality for obtaining sample for diagnosis in PPS tumor either intraorally, trascervically, or image guided. Recently, image-guided FNAC has proven useful both in terms of morphological analysis and cost and time effectiveness. CT scan and magnetic resonance imaging (MRI) are vital tools for PPS tumors, because they help to determine the extent of disease and tumor type, which in turn facilitates the planning of surgical procedure. MRI is the preferred diagnostic tool for imaging the PPS. T1-weighted images are ideal for demonstrating the normal PPS anatomy and any tumor-fat interfaces.10 Management of pleomorphic adenoma is by complete surgical excision. Although various surgical approaches have been described in the literature, the transcervical and transparotid approach are most frequently used.11 Malone et al,12 and Hamza et al,13 described the resection of PPS tumors using the transcervical approach alone in 90–100% of cases. We safely removed the tumor in toto by using a standard transcervical approach without any complications.
Conclusion
It is important to keep in mind that symptoms of upper airway obstruction may be the first presenting sign of benign tumor of PPS compressing the upper airway. A high index of suspicion should be kept to diagnose tumors of this space with unusual life-threatening presentation.
Disclosure
The authors declared no conflicts of interest.
references
- Khafif A, Segev Y, Kaplan DM, Gil Z, Fliss DM. Surgical management of parapharyngeal space tumors: a 10-year review. Otolaryngol Head Neck Surg 2005 Mar;132(3):401-406.
- 2. Morariu I, Dias A, Curran A. Giant parotid pleomorphic adenoma in parapharyngeal space causing severe obstructive sleep apnoea. Ir Med J 2012 Jun;105(6):184-185.
- 3. Veitch D, Rogers M, Blanshard J. Parapharyngeal mass presenting with sleep apnoea. J Laryngol Otol 1989 Oct;103(10):961-963.
- 4. Giddings CE, Bray D, Rimmer J, Williamson P. Pleomorphic adenoma and severe obstructive sleep apnoea. J Laryngol Otol 2005 Mar;119(3):226-229.
- 5. Moraitis D, Papakostas K, Karkanevatos A, Coast GJ, Jackson SR. Pleomorphic adenoma causing acute airway obstruction. J Laryngol Otol 2000 Aug;114(8):634-636.
- 6. Chijiwa H, Mihoki T, Shin B, Sakamoto K, Umeno H, Nakashima T. Clinical study of parapharyngeal space tumours. J Laryngol Otol Suppl 2009;123(31):100-103.
- 7. Whyte AM, Hourihan MD. The diagnosis of tumours involving the parapharyngeal space by computed tomography. Br J Radiol 1989 Jun;62(738):526-531.
- 8. Kim SH. Simultaneous primary pleomorphic adenoma in parotid gland and minor salivary gland in the parapharyngeal space. J Laryngol Otol 2001 Oct;115(10):829-830.
- 9. Hughes KV III, Olsen KD, McCaffrey TV. Parapharyngeal space neoplasms. Head Neck 1995 Mar-Apr;17(2):124-130.
- 10. Burke CJ, Thomas RH, Howlett D. Imaging the major salivary glands. Br J Oral Maxillofac Surg 2011 Jun;49(4):261-269.
- 11. Mendelsohn AH, Bhuta S, Calcaterra TC, Shih HB, Abemayor E, St John MA. Parapharyngeal space pleomorphic adenoma: a 30-year review. Laryngoscope 2009 Nov;119(11):2170-2174.
- 12. Malone JP, Agrawal A, Schuller DE. Safety and efficacy of transcervical resection of parapharyngeal space neoplasms. Ann Otol Rhinol Laryngol 2001 Dec;110(12):1093-1098.
- 13. Hamza A, Fagan JJ, Weissman JL, Myers EN. Neurilemomas of the parapharyngeal space. Arch Otolaryngol Head Neck Surg 1997 Jun;123(6):622-626.