Common and preventable childhood illnesses pose a stern challenge for healthcare professionals consequently adding to the global disease burden.1 Integrated Management of Childhood Illness (IMCI) strategy was developed and introduced by the World Health Organization (WHO) back in the year 1996.2 The strategy has been promoted globally with an aim to improve child healthcare especially in low- and middle-income countries.3 IMCI focuses on enhancing healthcare professionals’ knowledge, attitudes, and skills, as well as establishing a healthcare system that adheres with the recommended practices.4
Since 1996, IMCI strategy has been adopted and implemented in more than 100 countries. This was followed by a series of Multi-Country Evaluations (MCEs) to examine effectiveness of IMCI strategy in improving child health standards. However, an unexpected finding was that childhood mortality rates remained high despite the adoption and implementation of the IMCI strategy.5 Findings from recently published articles provided evidence that healthcare professionals do not adhere with the IMCI-recommended practices.6 It appeared that healthcare professionals had a tendency to trust their own skills and experiences while assessing cases and making diagnosis. While this could be true, we also propose that there is a lack of support and follow-ups by governments and healthcare policymakers to ensure actual practice of IMCI-recommended guidelines.
We are grounding our argument on the propositions made by Locock et al,7 who emphasized that for improved patient care, it is necessary that healthcare managers as well as medical professionals accept and adhere to novel clinical practices. However, to guarantee that the healthcare organizations and professionals follow novel or relatively new clinical practices, the role of governments and policymakers cannot be overlooked. It is suggested in available literature that the “opinion leaders” can have a positive influence on improving clinical practices.7 The precise definition of an “opinion leader” is rather vague, hence, we take the opportunity to define “opinion leaders” as governments’ and healthcare policymakers in the presented study.
A large number of published articles highlighted the benefits of IMCI on improved child healthcare. For example, in Tanzania, IMCI implementation resulted in 13% reduction in childhood mortality rates.8 Adoption and practice of IMCI-recommended guidelines have been positively correlated with improved child healthcare in several countries.9−13 In addition, it is believed to have positive effect on community health practices, healthcare professionals’ case assessment, and management skills.10,13,14 Still, the apparent benefits of IMCI-recommended practices have not been fully realized. Identifying the reasons that prevent IMCI-recommended practices in clinical settings is still a relatively unexplored area. There is a need for further research to examine the role of governments and healthcare policymakers as proposed by Locock et al.7
This study aims to test the hypothetical structural model to investigate the potential role of governments and healthcare policymakers in improving implementation and application of IMCI-recommended practices.
We hypothesize that once a government perceives IMCI-recommended practices as a valuable intervention, it will support its implementation using healthcare units’ management that would consequently result in more focus on IMCI-related teaching and training. We believe that with government and management support, IMCI-trained healthcare professionals will have positive behavioral intentions towards applying the recommended practices leading to higher adherence.
Methods
The study was conducted in June 2016 at Sur and Ibra Nursing Institutes, in Oman. A hypothetical structural model [Figure 1] was developed with the help of healthcare professionals and one expert of Health Information Systems. Two of the six healthcare professionals were IMCI consultants. The following constructs were agreed upon and used for the study: perceived usefulness (PU), government support (GS), management support (MS), IMCI-teaching and training (ITT), behavioral intention to use IMCI (BI), and actual use of IMCI (AU). PU, GS, MS, ITT, and BI were used as latent variables to examine their likely influence on actual use and application of IMCI-recommended practices. The model indicates the relationships between the studied constructs.
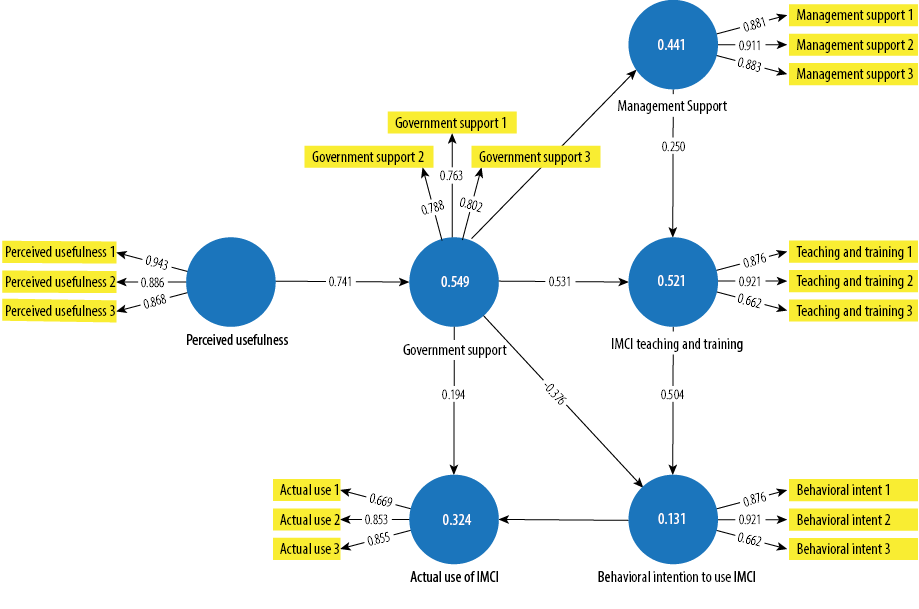
Figure 1: The hypothetical structural model of Integrated Management of Childhood Illness (IMCI).
A total of 101 healthcare professionals agreed to participate in this study. The participation was called using recruitment posters and pamphlets at Sur and Ibra Nursing Institutes. All the 101 participants had received IMCI training in the form of workshops, seminars, theoretical lectures, laboratory sessions, and field trips for a mean duration of 31.5 ± 0.4 hours.
For running a predictive statistical data analysis using Smart PLS version 3.2.6 (Ringle, Christian M., Wende, Sven, & Becker, Jan-Michael. (2015). SmartPLS 3. Bönningstedt: SmartPLS. Retrieved from http://www.smartpls.com), the minimum sample size was calculated using the heuristic method (i.e., by multiplying 10 with the largest number of independent constructs).15 Thus, the minimum sample size for successfully performing the statistics was 60. The questionnaire contained basic demographics and seven-point Likert scale items for assessing participants’ perceptions. The questionnaire was developed in English with a focus on gaining insights on how healthcare professionals perceive the role of governments in ensuring actual application of IMCI-recommended practices in clinical setting. While developing the questionnaire, the six healthcare professionals (two were IMCI experts) and one Health Information Systems’ expert went through several iterations to ensure that the language was clear and the terminologies were easily understood.
Ethical approval was obtained from the Ministry of Health, Oman. Each participant was required to give informed consent form to be eligible in the study. There were no financial incentives offered for being a part of the study.
Results
The research model was analyzed using partial least squares structural equation model (PLS-SEM) using SmartPLS version 3.2.6 for data analysis.16 It is a component-based path modeling software that is accepted as an appropriate tool when the research objective is to predict rather than testing an existing and validated theory.15 Further, the tool is robust for deviances from a multivariate distribution.17 The statistical objective of using SmartPLS is rather comparable to that of linear regression i.e., to exhibit described variance in latent variables indicated by R-squared (R2) values and to check the weight of the relations between latent variables using t-values accordingly reporting their p-values.15 SmartPLS test was performed in two steps: assessment of the reliability and validity of the measurement model, and assessment of the hypothetical structural model. The measurement model included the relationship between the studied constructs [Table 1], and the indicators that were used to measure them [Table 2].
Table 1: The relationships between the studied constructs.
|
AU |
0.730 |
0.846 |
0.649 |
12.072 |
< 0.050 |
|
BI |
0.851 |
0.911 |
0.773 |
21.119 |
< 0.050 |
|
GS |
0.691 |
0.828 |
0.616 |
19.263 |
< 0.050 |
|
ITT |
0.762 |
0.865 |
0.685 |
16.898 |
< 0.050 |
|
MS |
0.871 |
0.921 |
0.795 |
15.793 |
< 0.050 |
CA: cronbach’s alpha; CR: composite reliability; AVE: average variance extracted; AU: actual use of Integrated Management of Childhood Illness (IMCI); BI: behavioral intention to use IMCI; GS: government support; ITT: IMCI-teaching and training; MS: management support; PU: perceived usefulness.
For the measurement model, questionnaire items were thoroughly discussed and pretested by the healthcare professionals. Each construct in the questionnaire was loaded with three items. The properties of scale were measured in terms of factor loadings, discriminant validity, and internal consistency. Item loadings and their internal consistencies > 0.700 were advocated and accepted.18 All studied constructs in the model showed acceptable internal consistency. This is evident from the composite reliability scores that range between 0.828−0.927.15,18 In addition, latent variable correlations and average variance extracted (AVE) [Table 1] indicated that all the constructs shared more variance with their own indicators rather than the other constructs. Furthermore, the AVE scores for all the studied constructs were well above the minimum desired score of 0.500.19 These values highlighted acceptable internal consistency.
Table 2: The difference between structural loadings and cross-loadings.
|
Actual use 1 |
0.700 |
0.289 |
0.236 |
0.294 |
0.159 |
0.211 |
|
Actual use 2 |
0.853 |
0.464 |
0.177 |
0.466 |
0.285 |
0.088 |
|
Actual use 3 |
0.855 |
0.511 |
0.056 |
0.259 |
0.054 |
0.066 |
|
Behavioral intent 1 |
0.478 |
0.821 |
0.049 |
0.158 |
0.025 |
0.133 |
|
Behavioral intent 2 |
0.476 |
0.932 |
0.014 |
0.266 |
0.007 |
0.113 |
|
Behavioral intent 3 |
0.459 |
0.881 |
0.031 |
0.211 |
0.094 |
0.066 |
|
Government support 1 |
0.030 |
0.101 |
0.787 |
0.390 |
0.584 |
0.795 |
|
Government support 2 |
0.084 |
0.111 |
0.764 |
0.452 |
0.437 |
0.459 |
|
Government support 3 |
0.351 |
0.035 |
0.802 |
0.771 |
0.526 |
0.471 |
|
Management support 1 |
0.074 |
0.082 |
0.598 |
0.876 |
0.745 |
0.766 |
|
Management support 2 |
0.205 |
0.107 |
0.472 |
0.921 |
0.911 |
0.698 |
|
Management support 3 |
0.138 |
0.093 |
0.691 |
0.827 |
0.627 |
0.746 |
|
Perceived usefulness 1 |
0.051 |
0.085 |
0.712 |
0.433 |
0.881 |
0.943 |
|
Perceived usefulness 2 |
0.090 |
0.086 |
0.643 |
0.325 |
0.883 |
0.886 |
|
Perceived usefulness 3 |
0.070 |
0.151 |
0.641 |
0.511 |
0.862 |
0.868 |
|
Teaching and training 1 |
0.398 |
0.084 |
0.725 |
0.876 |
0.577 |
0.495 |
|
Teaching and training 2 |
0.417 |
0.189 |
0.574 |
0.921 |
0.560 |
0.460 |
AU: actual use of Integrated Management of Childhood Illness (IMCI); BI: behavioral intention to use IMCI; GS: government support; ITT: IMCI-teaching and training; MS: management support; PU: perceived usefulness.
In the structural model, GS explained 44.1% of the variance in MS. In turn, GS and MS together explained 52.2% variance in ITT. Further, ITT and GS accounted for 0.6% variance in BI. Lastly, BI and GS highlighted 32.4% variance in AU. It is worth noting that GS alone explained 13.1% and 32.4% variance in BI and AU, respectively. The effect sizes of Cohen's f2 method define and determine whether the effects indicated by path coefficients are small (0.02), medium (0.15), or large (0.35).1,20 The effect sizes below 0.02 are too weak to considered. All of the effect sizes for the total effects are > 0.02, hence, supporting their practical application. The total effects and effect sizes were exhibited in Table 3. Based on the statistical findings, the prime hypothesis was supported (i.e., R2 value, AU = 0.549 (54.9%)).
Table 3: Total effects and effect sizes.
|
AU |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
|
BI |
0.540***
f2 = 0.430 |
- |
- |
- |
- |
- |
|
GS |
0.285*
f2 = 0.060NS |
0.169NS
f2 = 0.080NS |
- |
0.697***
f2 = 0.330 |
0.664***
f2 = 0.790 |
- |
|
ITT |
0.131*
f2 = N/A |
0.242*
f2 = 0.150 |
- |
- |
- |
- |
|
MS |
0.033NS
f2 = N/A |
0.061NS
f2 = N/A |
- |
0.250*
f2 = 0.070 |
- |
- |
***p < 0.001.*p < 0.005. NS: Non significant; f2: Cohen’s f-squared; N/A: Not applicable; AU: actual use of Integrated Management of Childhood Illness (IMCI); BI: behavioral intention to use IMCI; GS: government support; ITT: IMCI-teaching and training; MS: management support; PU: perceived usefulness. Note: AU has N/A in all cells because it is an exogenous variable.
Discussion
The results from the statistical analysis support the hypothetical structural model. In addition, the overall model has loaded well. Factor loadings for each item were well above the minimum threshold.20 The composite reliability for all the studied constructs exceeded the desired value of 0.700.19 The R2 values was observed to be substantial. It was encouraging to observe that the R2 value for the central construct GS was 0.549 (54.9%). It was assuring to notice such value because even lower R2 values cannot be overlooked in predictive research.21
The study and statistical outcomes uncovered significant correlations between the studied constructs and expected influence of governments in ensuring IMCI-recommended practices. The findings from the study added to the existing knowledge base by highlighting the role of governments and healthcare policymakers towards improving child healthcare standards. These findings are supported by several studies.7,22,23 To the best of our knowledge, this study is first of its kind that investigates the role of governments in implementation and application of IMCI-recommended practices. Based on the findings, we propose that the governments and healthcare policymakers understand the paradigm shift in modern day healthcare systems. Evidently, IMCI brings potential benefits that can help reduce childhood mortality rates, however, we proposed that achieving the desired outcomes would be difficult without proactive government policies.
The study’s limitations were several and included the sample taken from the two nursing institutes had potential bias that cannot be overlooked, small sample size, the entire statistical analysis was based on participants’ opinions, and the sample did not include government officials. Nevertheless, the predictive analysis does highlight the perceived role of governments and healthcare policymakers in improving child healthcare standards. In the future, we plan to perform a qualitative study to examine and analyze the opinions of government officials and healthcare policymakers about possible strategies to implement and apply the IMCI-recommended practices in clinical settings.
Conclusions
A hypothetical structural model was developed and tested to identify the impact of governments on the implementation and actual application of IMCI-recommended practices. Government support was found to have a strong influence on the implementation and practical application of IMCI-recommended practices in clinical settings.
Disclosure
The authors declared no conflicts of interest. No funding was received for this work.
Acknowledgements
We would like to thank all the volunteer participants in the study. We would also like to thank the managements of Sur and Ibra Nursing institutes for their support.
references
- 1. Al-Araimi FA, Langrial SU. A Hypothetical Model to Predict Nursing Students’ Perceptions of the Usefulness of Pre-Service Integrated Management of Childhood Illness Training. Sultan Qaboos Univ Med J 2016 Nov;16(4):e469-e474.
- 2. Goga AE, Muhe LM, Forsyth K, Chopra M, Aboubaker S, Martines J, et al. Results of a multi-country exploratory survey of approaches and methods for IMCI case management training. Health Res Policy Syst 2009 Jul;7(1):18.
- 3. Tulloch J. Integrated approach to child health in developing countries. Lancet 1999 Sep;354(Suppl 2):SII16-SII20.
- 4. Bryce J, Boschi-Pinto C, Shibuya K, Black RE; WHO Child Health Epidemiology Reference Group. WHO estimates of the causes of death in children. Lancet 2005 Mar;365(9465):1147-1152.
- 5. Lange S, Mwisongo A, Mæstad O. Why don’t clinicians adhere more consistently to guidelines for the Integrated Management of Childhood Illness (IMCI)? Soc Sci Med 2014 Mar;104:56-63.
- 6. Ahmed HM, Mitchell M, Hedt B. National implementation of Integrated Management of Childhood Illness (IMCI): policy constraints and strategies. Health Policy 2010 Jul;96(2):128-133.
- 7. Locock L, Dopson S, Chambers D, Gabbay J. Understanding the role of opinion leaders in improving clinical effectiveness. Soc Sci Med 2001 Sep;53(6):745-757.
- 8. Bryce J, Victora CG, Habicht J-P, Vaughan JP, Black RE. The multi-country evaluation of the integrated management of childhood illness strategy: lessons for the evaluation of public health interventions. Am J Public Health 2004 Mar;94(3):406-415.
- 9. Amaral, J, Alvaro JML, Antonio JLAC, Cesar GV. Impact of IMCI health worker training on routinely collected child health indicators in Northeast Brazil. Health Policy and Planning 2005 Dec;20(suppl 1):i42-i48.
- 10. Pariyo GW1, Gouws E, Bryce J, Burnham G; Uganda IMCI Impact Study Team. Improving facility-based care for sick children in Uganda: training is not enough. Health policy planning 2005 Dec; 20(suppl 1):i58-i68.
- 11. Arifeen SE, Hoque DM, Akter T, Rahman M, Hoque ME, Begum K, et al. Effect of the Integrated Management of Childhood Illness strategy on childhood mortality and nutrition in a rural area in Bangladesh: a cluster randomised trial. Lancet 2009 Aug; 374(9687):393-403.
- 12. Wagstaff A, Bustreo F, Bryce J, Claeson M; WHO-World Bank Child Health and Poverty Working Group. Child health: reaching the poor. Am J Public Health 2004 May;94(5):726-736.
- 13. Naimoli JF, Rowe AK, Lyaghfouri A, Larbi R, Lamrani LA. Effect of the Integrated Management of Childhood Illness strategy on health care quality in Morocco. Int J Qual Health Care 2006 Apr;18(2):134-144.
- 14. Ebuehi OM. Health care for under-fives in Ile-Ife, South-West Nigeria: Effect of the Integrated Management of Childhood Illnesses (IMCI) strategy on growth and development of under-fives. Afr J Prim Health Care Fam Med 2009 June;1(1):29.
- 15. Hair JF, Ringle CM, Sarstedt M. PLS-SEM: Indeed a silver bullet. J Mark Theory Pract 2011;19(2):139-152.
- 16. Ringle CM, Wende S, Becker JM. SmartPLS 3. SmartPLS GmbH: Boenningstedt [cited 2015 Feb 24]. Available from: http://www.smartpls.com.
- 17. Gefen D, Straub DW, Rigdon EE. An update and extension to SEM guidelines for admnistrative and social science research. Manage Inf Syst Q 2011 June;35(2):iii-xiv.
- 18. Anderson JC, Gerbing DW. Structural equation modeling in practice: A review and recommended two-step approach. Psychol Bull 1988 May;103(3):411.
- 19. Nunnally JC, Bernstein IH. The assessment of reliability. Psychometric theory. 3rd ed. New York: McGraw-Hill;1994. p. 248-292.
- 20. Langrial S. Persuasive subtleties of social networking sites: Design implications for behavior change interventions. In: Theng LB, editor. Assistive Technologies for Physical and Cogn- itive Disabilities. Hershey, Pennsylvania, USA: IGI Global; 2014. pp. 191–210.
- 21. Onditi AA. Relationship between customer personality, service features and customer loyalty in the banking sector: A survey of banks in Homabay County, Kenya. Int J Bus Soc Sci 2013 Nov;4(15):132-150.
- 22. Hutchison B, Levesque JF, Strumpf E, Coyle N. Primary health care in Canada: systems in motion. Milbank Q 2011 Jun;89(2):256-288.
- 23. Dopson S, FitzGerald L, Ferlie E, Gabbay J, Locock L. No magic targets! Changing clinical practice to become more evidence based. Health Care Manage Rev 2002 Summer;27(3):35-47.